Airway Management and Endotracheal Intubation
Stephen O. Heard
Margaret M. Hudlin
Shubjeet Kaur
In the emergency room and critical care environment, management of the airway to ensure optimal ventilation and oxygenation is of prime importance. Although initial efforts should be directed toward improving oxygenation and ventilation without intubating the patient [1], these interventions may fail and the placement of an endotracheal tube may be required. Although endotracheal intubation is best left to the trained specialist, emergencies often require that the procedure be performed before a specialist arrives. Because intubated patients are commonly seen in the intensive care unit (ICU) and coronary care unit, all physicians who work in these environments should be skilled in the techniques of airway management, endotracheal intubation, and management of intubated patients.
Anatomy
An understanding of the techniques of endotracheal intubation and potential complications is based on knowledge of the anatomy of the respiratory passages [2]. Although a detailed anatomic description is beyond the scope of this book, an understanding of some features and relationships is essential to performing intubation.
Nose
The roof of the nose is partially formed by the cribriform plate. The anatomic proximity of the roof to intracranial structures dictates that special caution be exercised during nasotracheal intubations. This is particularly true in patients with significant maxillofacial injuries.
The mucosa of the nose is provided with a rich blood supply from branches of the ophthalmic and maxillary arteries, which allow air to be warmed and humidified. Because the conchae provide an irregular, highly vascularized surface, they are particularly susceptible to trauma and subsequent hemorrhage. The orifices from the paranasal sinuses and nasolacrimal duct open onto the lateral wall. Blockage of these orifices by prolonged nasotracheal intubation may result in sinusitis [3].
Mouth and Jaw
The mouth is formed inferiorly by the tongue, alveolar ridge, and mandible. The hard and soft palates compose the superior surface, and the oropharynx forms the posterior surface. Assessment of the anatomic features of the mouth and jaw is essential before orotracheal intubation. A clear understanding of the anatomy is also essential when dealing with a patient who has a difficult airway and when learning how to insert newer airway devices such as the laryngeal mask airway (LMA; discussed in the section Management of the Difficult Airway).
Nasopharynx
The base of the skull forms the roof of the nasopharynx, and the soft palate forms the floor. The roof and the posterior walls of the nasopharynx contain lymphoid tissue (adenoids), which may become enlarged and compromise nasal airflow or become injured during nasal intubation, particularly in children. The eustachian tubes enter the nasopharynx on the lateral walls and may become blocked secondary to swelling during prolonged nasotracheal intubation.
Oropharynx
The soft palate defines the beginning of the oropharynx, which extends inferiorly to the epiglottis. The palatine tonsils protrude from the lateral walls and in children occasionally become so enlarged that exposure of the larynx for intubation becomes difficult. A large tongue can also cause oropharyngeal obstruction. Contraction of the genioglossus muscle normally moves the tongue forward to open the oropharyngeal passage during inspiration. Decreased tone of this muscle (e.g., in the anesthetized state) can cause obstruction. The oropharynx connects the posterior portion of the oral cavity to the hypopharynx.
Hypopharynx
The epiglottis defines the superior border of the hypopharynx, and the beginning of the esophagus forms the inferior boundary. The larynx is anterior to the hypopharynx. The pyriform sinuses that extend around both sides of the larynx are part of the hypopharynx.
Larynx
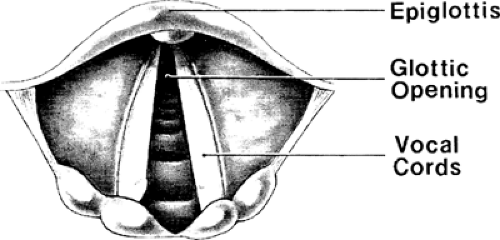
The larynx (Fig. 1-1) is bounded by the hypopharynx superiorly and is continuous with the trachea inferiorly. The thyroid, cricoid, epiglottic, cuneiform, corniculate, and arytenoid cartilages compose the laryngeal skeleton. The thyroid and cricoid
cartilages are readily palpated in the anterior neck. The cricoid cartilage articulates with the thyroid cartilage and is joined to it by the cricothyroid ligament. When the patient’s head is extended, the cricothyroid ligament can be pierced with a scalpel or large needle to provide an emergency airway (see Chapter 12). The cricoid cartilage completely encircles the airway. It is attached to the first cartilage ring of the trachea by the cricotracheal ligament. The anterior wall of the larynx is formed by the epiglottic cartilage, to which the arytenoid cartilages are attached. Fine muscles span the arytenoid and thyroid cartilages, as do the vocal cords. The true vocal cords and space between them are collectively termed the glottis (Fig. 1-2). The glottis is the narrowest space in the adult upper airway. In children, the cricoid cartilage defines the narrowest portion of the airway. Because normal phonation relies on the precise apposition of the true vocal cords, even a small lesion can cause hoarseness. Lymphatic drainage to the true vocal cords is sparse. Inflammation or swelling caused by tube irritation or trauma may take considerable time to resolve. The superior and recurrent laryngeal nerve branches of the vagus nerve innervate the structures of the larynx. The superior laryngeal nerve supplies sensory innervation from the inferior surface of the epiglottis to the superior surface of the vocal cords. From its takeoff from the vagus nerve, it passes deep to both branches of the carotid artery. A large internal branch pierces the thyrohyoid membrane just inferior to the greater cornu of the hyoid. This branch can be blocked with local anesthetics for oral or nasal intubations in awake patients. The recurrent laryngeal branch of the vagus nerve provides sensory innervation below the cords. It also supplies all the muscles of the larynx except the cricothyroid, which is innervated by the external branch of the superior laryngeal nerve.
cartilages are readily palpated in the anterior neck. The cricoid cartilage articulates with the thyroid cartilage and is joined to it by the cricothyroid ligament. When the patient’s head is extended, the cricothyroid ligament can be pierced with a scalpel or large needle to provide an emergency airway (see Chapter 12). The cricoid cartilage completely encircles the airway. It is attached to the first cartilage ring of the trachea by the cricotracheal ligament. The anterior wall of the larynx is formed by the epiglottic cartilage, to which the arytenoid cartilages are attached. Fine muscles span the arytenoid and thyroid cartilages, as do the vocal cords. The true vocal cords and space between them are collectively termed the glottis (Fig. 1-2). The glottis is the narrowest space in the adult upper airway. In children, the cricoid cartilage defines the narrowest portion of the airway. Because normal phonation relies on the precise apposition of the true vocal cords, even a small lesion can cause hoarseness. Lymphatic drainage to the true vocal cords is sparse. Inflammation or swelling caused by tube irritation or trauma may take considerable time to resolve. The superior and recurrent laryngeal nerve branches of the vagus nerve innervate the structures of the larynx. The superior laryngeal nerve supplies sensory innervation from the inferior surface of the epiglottis to the superior surface of the vocal cords. From its takeoff from the vagus nerve, it passes deep to both branches of the carotid artery. A large internal branch pierces the thyrohyoid membrane just inferior to the greater cornu of the hyoid. This branch can be blocked with local anesthetics for oral or nasal intubations in awake patients. The recurrent laryngeal branch of the vagus nerve provides sensory innervation below the cords. It also supplies all the muscles of the larynx except the cricothyroid, which is innervated by the external branch of the superior laryngeal nerve.
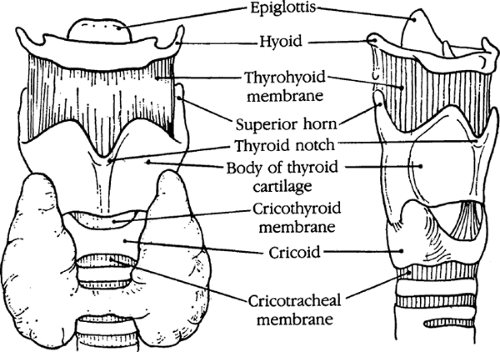 FIGURE 1-1. Anatomy of the larynx, anterior and lateral aspects. [From Ellis H: Anatomy for Anaesthetists. Oxford, Blackwell Scientific, 1963, with permission.] |
Trachea
The adult trachea averages 15 cm long. Its external skeleton is composed of a series of C-shaped cartilages. It is bounded posteriorly by the esophagus and anteriorly for the first few cartilage rings by the thyroid gland. The trachea is lined with ciliated cells that secrete mucus; through the beating action of the cilia, foreign substances are propelled toward the larynx. The carina is located at the fourth thoracic vertebral level (of relevance when judging proper endotracheal tube positioning on chest radiograph). The right main bronchus takes off at a less acute angle than the left, making right main bronchial intubation more common if the endotracheal tube is in too far.
Emergency Airway Management
In an emergency situation, establishing adequate ventilation and oxygenation assumes primary importance [4]. Too frequently, inexperienced personnel believe that this requires immediate intubation; however, attempts at intubation may delay establishment of an adequate airway. Such efforts are time consuming, can produce hypoxemia and arrhythmias, and may induce bleeding and regurgitation, making subsequent attempts to intubate significantly more difficult and contributing to significant patient morbidity and even mortality [5,6]. Some simple techniques and principles of emergency airway management can play an important role until the arrival of an individual who is skilled at intubation.
Airway Obstruction
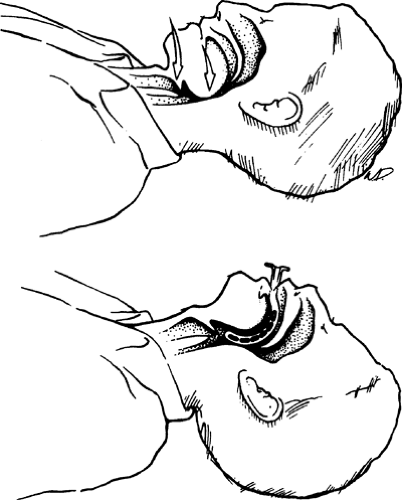
Compromised ventilation often results from upper airway obstruction by the tongue, by substances retained in the mouth, or by laryngospasm. Relaxation of the tongue and jaw leading to a reduction in the space between the base of the tongue and the posterior pharyngeal wall is the most common cause of upper airway obstruction. Obstruction may be partial or complete. The latter is characterized by total lack of air exchange. The former is recognized by inspiratory stridor and retraction of neck and intercostal muscles. If respiration is inadequate, the head-tilt–chin-lift or jaw-thrust maneuver should be performed. In patients with suspected cervical spine injuries, the jaw-thrust maneuver (without the head tilt) may result in the least movement of the cervical spine. To perform the head-tilt maneuver, place a palm on the patient’s forehead and apply pressure to extend the head about the atlantooccipital joint. To perform the chin lift place several fingers of the other hand in the submental area and lift the mandible. Care must be taken to avoid airway obstruction by pressing too firmly on the soft tissues in the submental area. To perform the jaw thrust lift up on the angles of the mandible [4] (Figure 1-3). Both of these maneuvers open the oropharyngeal passage. Laryngospasm can be treated by maintaining positive airway pressure using a face mask and bag valve device (see the following section). If the patient resumes spontaneous breathing, establishing this head position may constitute
sufficient treatment. If obstruction persists, a check for foreign bodies, emesis, or secretions should be performed [7].
sufficient treatment. If obstruction persists, a check for foreign bodies, emesis, or secretions should be performed [7].
Use of Face Mask and Bag Valve Device
If an adequate airway has been established and the patient is not breathing spontaneously, oxygen can be delivered via face mask and a bag valve device. It is important to establish a tight fit with the face mask, covering the patient’s mouth and nose. To perform this procedure apply the mask initially to the bridge of the nose and draw it downward toward the mouth, using both hands. The operator stands at the patient’s head and presses the mask onto the patient’s face with the left hand. The thumb should be on the nasal portion of the mask, the index finger near the oral portion, and the rest of the fingers spread on the left side of the patient’s mandible so as to pull it slightly forward. The bag is then alternately compressed and released with the right hand. A good airway is indicated by the rise and fall of the chest; moreover, lung-chest wall compliance can be estimated from the amount of pressure required to compress the bag. The minimum effective insufflation pressure should be used to decrease the risk of insufflating the stomach with gas and subsequently increase the risk of aspiration.
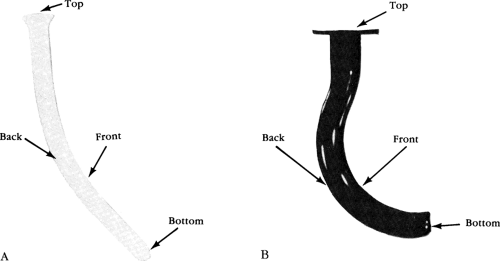 FIGURE 1-4. Nasopharyngeal (A) or oropharyngeal (B) airways can be used to relieve soft tissue obstruction if elevating the mandible proves ineffective. |
Airway Adjuncts
If proper positioning of the head and neck or clearance of foreign bodies and secretions fails to establish an adequate airway, several airway adjuncts may be helpful if an individual who is skilled in intubation is not immediately available. An oropharyngeal or nasopharyngeal airway occasionally helps to establish an adequate airway when proper head positioning alone is insufficient (Figs. 1-4 and 1-5). The oropharyngeal airway is semicircular and made of plastic or hard rubber. The two types are the Guedel airway, with a hollow tubular design, and the Berman airway, with airway channels along the sides. Both
types are most easily inserted by turning the curved portion toward the palate as it enters the mouth. It is then advanced beyond the posterior portion of the tongue and rotated downward into the proper position (Fig. 1-5). Often, depressing the tongue or moving it laterally with a tongue blade helps to position the oropharyngeal airway. Care must be exercised not to push the tongue into the posterior pharynx, causing or exacerbating obstruction. Because insertion of the oropharyngeal airway can cause gagging or vomiting, or both, it should be used only in unconscious patients.
types are most easily inserted by turning the curved portion toward the palate as it enters the mouth. It is then advanced beyond the posterior portion of the tongue and rotated downward into the proper position (Fig. 1-5). Often, depressing the tongue or moving it laterally with a tongue blade helps to position the oropharyngeal airway. Care must be exercised not to push the tongue into the posterior pharynx, causing or exacerbating obstruction. Because insertion of the oropharyngeal airway can cause gagging or vomiting, or both, it should be used only in unconscious patients.
 FIGURE 1-6. The proper position of the nasopharyngeal airway. [From Textbook of Advanced Cardiac Life Support. Dallas, American Heart Association, 1997, with permission.] |
The nasopharyngeal airway is a soft tube approximately 15 cm long that is made of rubber or plastic (Figs. 1-4 and 1-6). It is inserted through the nostril into the posterior pharynx. Before insertion, the airway should be lubricated with an anesthetic gel, and, preferably, a vasoconstrictor should be administered into the nostril. The nasopharyngeal airway should not be used in patients with extensive facial trauma or cerebrospinal rhinorrhea, as it could be inserted through the cribriform plate into the brain.
Indications for Intubation
The indications for endotracheal intubation can be divided into four broad categories: (a) acute airway obstruction, (b) excessive pulmonary secretions or inability to clear secretions adequately, (c) loss of protective reflexes, and (d) respiratory failure [Table 1-1].
Preintubation Evaluation
Even in the most urgent situation, a rapid assessment of the patient’s airway anatomy can expedite the choice of the proper route for intubation, the appropriate equipment, and the most useful precautions to be taken. In the less emergent situation, several minutes of preintubation evaluation can decrease the likelihood of complications and increase the probability of successful intubation with minimal trauma.
Anatomic structures of the upper airway, head, and neck must be examined, with particular attention to abnormalities that might preclude a particular route of intubation. Evaluation of cervical spine mobility, temporomandibular joint function, and dentition is important. Any abnormalities that might prohibit alignment of the oral, pharyngeal, and laryngeal axes should be noted.
TABLE 1-1. Indications for Endotracheal Intubation | |
|---|---|
|
Cervical spine mobility is assessed by flexion and extension of the neck (performed only after ascertaining that no cervical spine injury exists). The normal range of neck flexion-extension varies from 165 to 90 degrees, with the range decreasing approximately 20% by age 75 years. Conditions associated with decreased range of motion include any cause of degenerative disk disease (e.g., rheumatoid arthritis, osteoarthritis, ankylosing spondylitis), previous trauma, or age older than 70 years. Temporomandibular joint dysfunction can occur in any form of degenerative arthritis (particularly rheumatoid arthritis), in any condition that causes a receding mandible, and in rare conditions such as acromegaly.
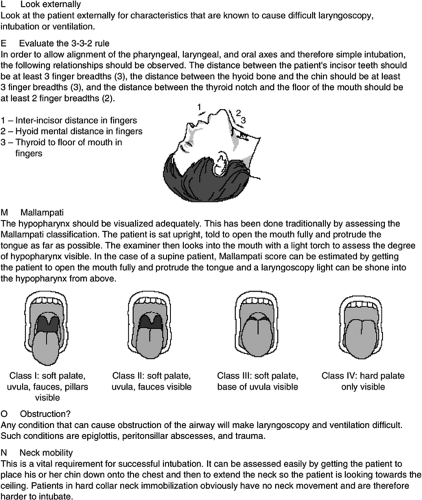
Examination of the oral cavity is mandatory. Loose, missing, or chipped teeth and permanent bridgework are noted, and removable bridgework and dentures should be taken out. Mallampati et al. [8] (Fig. 1-7) developed a clinical indicator based on the size of the posterior aspect of the tongue relative to the size of the oral pharynx. The patient should be sitting, with the head fully extended, protruding the tongue and phonating [9]. When the faucial pillars, the uvula, the soft palate, and the posterior pharyngeal wall are well visualized, the airway is classified as class I, and a relatively easy intubation can be anticipated. When the faucial pillars and soft palate (class II) or soft palate only (class III) are visible, there is a greater chance of problems
visualizing the glottis during direct laryngoscopy. Difficulties in orotracheal intubation may also be anticipated if (a) the patient is an adult and cannot open his or her mouth more than 40 mm (two finger breadths), (b) the distance from the thyroid notch to the mandible is less than three finger breadths (less than or equal to 7 cm), (c) the patient has a high arched palate, or (d) the normal range of flexion-extension of the neck is decreased (less than or equal to 80 degrees) [10]. The positive predictive values of these tests alone or in combination are not particularly high; however, a straightforward intubation can be anticipated if the test results are negative [11]. However, in the emergency setting, only about 30% of airways can be assessed in this fashion [12]. A different evaluation method (LEMON) has been devised by Murphy and Walls [13]. LEMON stands for look, evaluate, Mallampati class, obstruction, and neck mobility (Fig. 1-7). In the emergency setting, there are still limitations with the use of LEMON. However, using elements of LEMON that could be incorporated into the emergency evaluation of patients, Reed et al. [14] found that large incisors, a reduced interincisor distance, and a reduced distance between the thyroid and floor of the mouth were associated with a limited laryngoscopic view in emergency department patients.
visualizing the glottis during direct laryngoscopy. Difficulties in orotracheal intubation may also be anticipated if (a) the patient is an adult and cannot open his or her mouth more than 40 mm (two finger breadths), (b) the distance from the thyroid notch to the mandible is less than three finger breadths (less than or equal to 7 cm), (c) the patient has a high arched palate, or (d) the normal range of flexion-extension of the neck is decreased (less than or equal to 80 degrees) [10]. The positive predictive values of these tests alone or in combination are not particularly high; however, a straightforward intubation can be anticipated if the test results are negative [11]. However, in the emergency setting, only about 30% of airways can be assessed in this fashion [12]. A different evaluation method (LEMON) has been devised by Murphy and Walls [13]. LEMON stands for look, evaluate, Mallampati class, obstruction, and neck mobility (Fig. 1-7). In the emergency setting, there are still limitations with the use of LEMON. However, using elements of LEMON that could be incorporated into the emergency evaluation of patients, Reed et al. [14] found that large incisors, a reduced interincisor distance, and a reduced distance between the thyroid and floor of the mouth were associated with a limited laryngoscopic view in emergency department patients.
Equipment for Intubation
Assembly of all appropriate equipment before attempted intubation can prevent potentially serious delays in the event of an unforeseen complication. Most equipment and supplies are readily available in the ICU but must be gathered so they are immediately at hand. A supply of 100% oxygen and a well-fitting mask with attached bag valve device are mandatory, as is suctioning equipment, including a large-bore tonsil suction attachment (Yankauer) and suction catheters. Adequate lighting facilitates airway visualization. The bed should be at the proper height, with the headboard removed and the wheels locked. Other necessary supplies include gloves, Magill forceps, oral and nasal airways, laryngoscope handle and blades (straight and curved), endotracheal tubes of various sizes, stylet, tongue depressors, a syringe for cuff inflation, and tape for securing the endotracheal tube in position. Table 1-2 is a checklist of supplies needed.
It is particularly important that an adequate number of personnel be available to assist the operator. Endotracheal intubation and emergency airway management are not one-person jobs. While the operator is performing a rapid preintubation assessment, ICU personnel should be gathering equipment. During and before intubation, a respiratory therapist should be present whose sole concerns should be assisting in airway control before intubation and providing adequate oxygenation. It is helpful to have another assistant present who is familiar with the procedure and equipment and who should be ready to hand items to the operator on request.
Laryngoscopes
The two-piece laryngoscope has a handle containing batteries that power the bulb in the blade. The blade snaps securely into the top of the handle, making the electrical connection. Failure of the bulb to illuminate suggests improper blade positioning, bulb failure, a loose bulb, or dead batteries. Modern laryngoscope blades with fiberoptic lights obviate the problem of bulb failure. Many blade shapes and sizes are available. The two most commonly used blades are the curved (MacIntosh) and straight (Miller) blades (Fig. 1-8). Although pediatric blades are available for use with the adult-sized handle, most anesthesiologists prefer a smaller handle for better control in the pediatric population. The choice of blade shape is a matter of personal preference and experience; however, one study has suggested that less force and head extension are required when performing direct laryngoscopy with a straight blade [15].
TABLE 1-2. Equipment Needed for Intubation | |
|---|---|
|
Endotracheal Tubes
The internal diameter of the endotracheal tube is measured using both millimeters and French units. This number is stamped on the tube. Tubes are available in 0.5-mm increments, starting at 2.5 mm. Lengthwise dimensions are also marked on the tube in centimeters, beginning at the distal tracheal end.
Selection of the proper tube diameter is of utmost importance and is a frequently underemphasized consideration. The resistance to airflow varies with the fourth power of the radius of the endotracheal tube. Thus, selection of an inappropriately small tube can significantly increase the work of breathing. Moreover, certain diagnostic procedures (e.g., bronchoscopy) done through endotracheal tubes require appropriately large tubes (see Chapter 9). In general, the larger the patient, the larger the endotracheal tube that should be used. Approximate guidelines for tube sizes and lengths by age are summarized inTable 1-3. Most adults should be intubated with an endotracheal tube that has an inner diameter of at least 8.0 mm, although occasionally nasal intubation in a small adult requires a 7.0-mm tube.
Endotracheal Tube Cuff
Endotracheal tubes have low-pressure, high-volume cuffs to reduce the incidence of ischemia-related complications. Tracheal ischemia can occur any time cuff pressure exceeds capillary pressure (approximately 32 mm Hg), thereby causing inflammation, ulceration, infection, and dissolution of cartilaginous rings. Failure to recognize this progressive degeneration sometimes results in erosion through the tracheal wall (into the innominate artery if the erosion was anterior or the esophagus if the erosion was posterior) or long-term sequelae of tracheomalacia or tracheal stenosis. With cuff pressures of 15 to 30 mm Hg, the low-pressure, high-volume cuffs conform well to the tracheal wall and provide an adequate seal during positive-pressure ventilation. Although low cuff pressures can cause some damage (primarily ciliary denudation), major complications are rare. Nevertheless, it is important to realize that a low-pressure, high-volume cuff can be converted to a high-pressure cuff if sufficient quantities of air are injected into the cuff.
Anesthesia Before Intubation
Because patients who require intubation often have a depressed level of consciousness, anesthesia is usually not required. If intubation must be performed on the alert, responsive patient, sedation or general anesthesia exposes the individual to potential pulmonary aspiration of gastric contents because protective reflexes are lost. This risk is a particularly important consideration if the patient has recently eaten and must be weighed against the risk of various hemodynamic derangements that may occur secondary to tracheal intubation and initiation of positive-pressure
ventilation. Laryngoscopy in an inadequately anesthetized patient can result in tachycardia and an increase in blood pressure. This may be well tolerated in younger patients but may be detrimental in a patient with coronary artery disease or raised intracranial pressure. Sometimes laryngoscopy and intubation may result in a vasovagal response, leading to bradycardia and hypotension. Initiation of positive-pressure ventilation in a hypovolemic patient can lead to hypotension from diminished venous return.
ventilation. Laryngoscopy in an inadequately anesthetized patient can result in tachycardia and an increase in blood pressure. This may be well tolerated in younger patients but may be detrimental in a patient with coronary artery disease or raised intracranial pressure. Sometimes laryngoscopy and intubation may result in a vasovagal response, leading to bradycardia and hypotension. Initiation of positive-pressure ventilation in a hypovolemic patient can lead to hypotension from diminished venous return.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree