Toxicology
Med Lett Drugs Ther 2002;44:21; Crit Care Med 2003;31:2794
25.1 Activated Charcoal
The use of activated charcoal has become ubiquitous in overdose rx. Knowing the complications and significance of such is of paramount importance. One study found that multidose activated charcoal can lead to the following complications (Ann EM 2003;41:370):
Aspiration (0.5% incidence with no deaths) vs 1.6% incidence with 8.5% mortality rate (control group with 0.4% mortality) in competing study (Crit Care Med 2004;32:88)
Hypernatremia (6% incidence)
Hypermagnesemia (3.1% incidence)
Corneal abrasion (0.1% incidence)
Of note, gi obstruction was not seen in this series. Yet, a study of healthy volunteers finds that many minor effects can have an effect on ability to successfully complete an rx with activated charcoal, and the following effects were found when compared to controls (only those with differences shown here) (Hawaii Med J 2002;61:251):
Constipation or abdominal fullness (50% incidence)
Nausea (20% incidence)
Vomiting (8% incidence), may be as high as 26% incidence (J Toxicol Clin Toxicol 2002;40:775)
Diarrhea (8% incidence)
Finally, whether single-dose oral activated charcoal makes a difference in the rx of relatively low-risk, self-poisoned pts is controversial and looking at clinical deterioration, length of stay in the ER or hospital, and complication rates show no difference in one study (Am J Ther 2002;9:301). Important to note that significantly acute ingestions with potentially serious sequela (hydrocarbons including acetaminophen > 140 mg/kg, crack cocaine, mushrooms, caustic agents, heavy metals, lithium or iron) were all excluded from this study.
25.2 Acetaminophen
Cause: Ingestion.
Epidem: Most common reason for call to Poison Control; increased risk of toxicity in those with chronic disease, malnourishment, or liver disease (interestingly, chronic alcoholism can lead to these risk factors).
Pathophys: Causes liver failure secondary to metabolite which depletes reduced glutathione and perhaps secondary release of mitochondrial Ca. Stages will be covered below, and Stage I is within 24 hr Stage II is 24-48 hr, Stage III is 72-96 hr, and Stage IV is 96 hr-2 wks.
Sx: H/o ingestion > 10 gm in adult in < 24 hr, peds > 140 mg/kg single dose.
Stage I: Nausea, vomiting.
Stage II: Abdominal pain, not urinating.
Stage III: Laboratory abnormalities.
Stage IV: Declaration of liver injury—either improving or failing.
Si: None specific
Stage I: Clammy and pale skin.
Stage II: RUQ abdominal pain.
Stage III: Laboratory abnormalities.
Stage IV: Declaration of liver injury—either improving or failing.
Crs.: Most LFT abnormalities are transient, yet may be the harbinger of a fatal reaction.
Cmplc: Co-ingestions (ethanol, anticonvulsants) can amplify toxic effects, or cause delayed symptoms and peak levels; nomogram not accurate in circumstances where co-ingested materials (cold remedies) alter uptake (Brit J Clin Pharmacol 1999;48:278).
Lab: Acetaminophen level at 4, 8, and 12 hr (see Figure 25.1) gives prognostic data (Am J Hlth Syst Pharm 1999;56:1081), and upon arrival to ER (Scand J Gastroenterol 1999;34:723); liver profile; salicylate level; ethanol level; CBC with diff; PT/PTT; urine toxic drug screen; EKG. Possible use of urine acetaminophen to r/o ingestion (J Toxicol Clin Toxicol 1999;37:769).
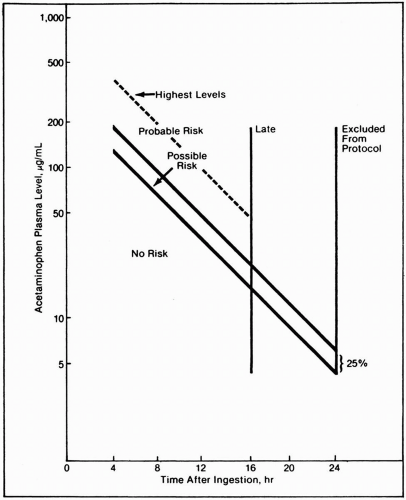 Figure 25.1 Study design nomogram. Possible risk is 25% below nomogram for multiclinic open-study purpose only. Reproduced with permission from Rumack BH, et al., Acetaminophen overdose. Arch IM 1981;141:380. |
Emergency Management:
Acetylcysteine po 140 mg/kg load then 70 mg/kg every 4 hr for a total of 18 doses (Arch IM 1981;141:380). Iv as efficacious (J Toxicol Clin Toxicol 1999;37:759) and use of the ingestion form for iv administration is safe (Ann EM 2003;42:9); doses are the same of 3% solution infused over 1 hr (Crit Care Med 1998;26:40).
Activated charcoal 1 gm/kg (J Toxicol Clin Toxicol 1999;37:753) if given within an hr of ingestion; do not use Sorbitol as cathartic in these cases, but sodium sulfate instead, if cathartic needed. No data that charcoal impedes absorption of acetylcysteine, but some advocate giving extra acetylcysteine in loading dose such as 150 mg/kg. The usefulness of activated charcoal in acetaminophen overdose cases is being more scrutinized.
Studies have shown that hypothyroidism and cimetidineinduced delayed gastric emptying may have had a small beneficial effect in certain populations, but PTU and cimetidine are not advocated as emergency medicine treatment.
25.3 Antidepressants
Cause: Tricyclic antidepressants (TCAs) are discussed here, with MAO inhibitors and SSRIs (discussion in Acute Serotonin Syndrome on p249). St. John’s Wort is a weak MAO inhibitor. Cyclobenzaprine (Flexeril) is similar to TCAs.
Pathophys: The mortal effect of TCAs has to do with Na-channel blockade in the myocardium. Na-channel blockade causes decreased ionotropic action, conduction defects (heart block, widening QRS, ectopic beats), and resulting hypotension (Am J Emerg Med 1988;6:439). The anticholinergic effects and
α-blocking effects may cause symptoms, but these are usually secondary and not fatal.
α-blocking effects may cause symptoms, but these are usually secondary and not fatal.
Sx: Anticholinergic symptoms—dry mouth, dry skin, confusion, palpitations.
Si: Tachycardia, altered mental status, hypotension, seizures, coma.
Crs: When these problems occur, they do so rapidly—altered mental status (J Toxicol Clin Toxicol 1992;30:161), cardiac conduction defects, arrhythmias, and seizures are poor prognostic indicators (Am J Emerg Med 1986;4:496). Hypotension due to cardiogenic shock has high mortality.
Cmplc: ARDS (Chest 1989;96:852; Ann Pharmacother 1993;27:572), pancreatitis (J Toxicol Clin Toxicol 1994;32:425).
Diff Dx: Consider other similar toxic overdoses (wide QRS with seizures), such as cocaine, lithium, phenothiazines, antihistamines, carbamazepine, quinidine, quinine, propoxyphene, propranolol, phenothiazines, bupivicaine, and lidocaine.
Lab: EKG looking for right axis deviation (Ann EM 1989;18:348), wide QRS, or prolonged QT (Am J Cardiol 1986;57:1154); glucoscan; CBC with diff; metabolic profile; ABG; ethanol level; acetaminophen level; salicylate level; urine toxic drug screen.
Emergency Management:
Airway, O2
Iv access, consider naloxone and thiamine 100 mg iv as overdose/coma protocol.
Gastric lavage if within 1 hr of presentation, followed by activated charcoal 1 gm/kg—activated charcoal is the most important tool (J Emerg Med 1995;13:203); Be prepared to protect the airway if necessary, since sudden deterioration is a possibility.
NaHCO3 1-2 mg/kg iv bolus, followed by 2 cc/kg/hr drip of 1 L of D5W with 2-3 amps of NaHCO3 added. Use NaHCO3 if wide QRS (> 0.1 sec), refractory hypotension or cardiac
arrhythmias noted. Goal of rx is pH 7.50-7.55 (J Toxicol Clin Toxicol 2004;42:1).
Lidocaine is second line drug for arrhythmias, and would avoid use of disopyramide, imipramine, procainamide, quinidine, flecainide, propafenone, β-blockers, and Ca channel blockers.
Role of phenytoin to be elucidated for cardiac arrhythmias (Ann EM 1981;10:270).
Benzodiazepines for seizures, followed by phenobarbital.
Hypotension refractory to fluids and NaHCO3 should be treated with norepinephrine 2-20 µg/min, avoid dopamine (Am J Emerg Med 1988;6:566).
Refractory arrhythmia/complex widening, despite sodium bicarbonate and an alkalemic blood gas, and refractory hypotension, despite iv fluids and norepinephrine, may prompt use of hypertonic NaCl (7.5% solution) as a 200 cc bolus (Ann EM 2003;42:20).
Perhaps Fab or single chain Fv fragment (sFv) fragments for desipramine overdose (Toxicol Lett 1995;82-83:801).
Consider extracorporeal circulation, if not responding to usual methods (Am J Emerg Med 1994;12:456).
Admission for continuous cardiac monitoring for 24 hr if not toxic (Jama 1985;254:1772).
25.4 Arsenic (Acute and Chronic Types)
Cause: Insecticides and herbicides, especially crab grass killers.
Epidem: Arsenic associated water poisoning puts millions of people at risk in many parts of the world (Int J Hyg Environ Hlth 2003;206:323; Bull World Hlth Organ 2000;78:1093; J Water Hlth 2003;1:73).
Pathophys: Blocks Krebs cycle.
Sx:
Acute: Nausea, vomiting and diarrhea with esophageal and epigastric pain; immediate “rice water” then bloody stool; CHF (myocardiopathy), with risk of increased QT and torsades de pointes or ventricular tachycardia, treat with pacer or MgSO4.
Chronic: Vague malaise.
Si:
Acute: Dyspnea, guaiac-positive stools.
Crs: After several days mucous membrane inflammation, rashes, hematologic, ATN, encephalopathy, painful peripheral, sensory, and motor neuropathy after 7-14 d.
Cmplc: Lung cancer incidence increased (Jama 2004;292:2984); r/o similar toxicity from arsine gas from industrial exposure in semiconductor industry.
Lab:
Chemistries: in acute, spot urine level; in chronic, arsenic tissue levels in bone, nails, hair (pubic best, since fast-growing and sweat adds Hg); normal levels = 3-13 µgm/100 gm; 24-h urine arsenic level, fewer false positives than blood levels, but will be back to normal when presents with neuropathy, but can bring it out with dimercaprol.
X-ray: KUB shows radiodense cast of stomach or gi tract acutely.
Emergency Management:
Dimercaprol (BAL, British anti-Lewisite) 3-5 mg/kg im q 4 hr over several d; within first 24-36 hr to chelate arsenic and reverse symptoms (Am J Emerg Med 1988;6:602). Few
complications at these doses in adults or children (Am J Emerg Med 1995;13:432).
Succimer, aka DMSA (2,3-dimercaptosuccinic acid) treatment (Am J Emerg Med 1995;13:432) (see Emergency Management in Lead p466 for dosing)
D-penicillamine 125 mg or 250 mg po qd as alternative therapy (Vet Hum Toxicol 1981;23:164).
25.5 Benzodiazepine
Cause: Ingestion or parenteral use of benzodiazepines; mixed overdoses common (J Forensic Sci 1997:155).
Epidem: Common intentional overdose, occasionally miscalculated medicine dosing.
Sx/Si: Nonspecific; sleepiness.
Crs: Most recover from pure ingestions; the elderly may present as being delirious.
Cmplc: Co-ingestions usually cause most problems with coma, respiratory depression, or hypotension; withdrawal from benzodiazepines may precipitate seizures—avoid this if at all possible.
Lab: Search for co-ingestions with ethanol level; acetaminophen level; salicylate level; CBC with diff; metabolic profile; urine toxic drug screen; EKG.
Emergency Management:
Airway support; iv access and fluid bolus if hypotensive; consider activated charcoal 1 gm/kg po if < 1-2 hr since ingestion and competent airway.
Do not reverse with flumazenil (Romazicon) (Crit Care Med 1992;20:1733; Am J Emerg Med 1992;10:184) unless adverse
side effect of parenteral sedation in ER or hospital inpatient who is not ethanol or benzodiazepine dependent. Otherwise, may precipitate seizure. Dose of flumazenil is 1 mg over 3 min every 1 hr prn.
25.6 Carbon Monoxide
Cause: Carbon monoxide (CO) inhalation, from combustible sources.
Epidem: Common sources are car exhaust, cigarette or any fire smoke, gas appliances with closed space inhalation.
Pathophys: CO has a 200X affinity for Hgb than O2, with a slow dissociation rate (Circ 1981;63:253A): It shifts the Hgb dissociation curve to the left, which means that it also decreases O2 dissociation.
Sx: Cherry red skin; headache; dizziness; altered mental status (Arch Surg 1973;107:851)—30-40 mg% CO; coma— > 40 mg% CO.
Si: Cherry red skin; retinal hemorrhages.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree




