Orthopedics
16.1 Bursitis/Tendonitis
Cause: Inflammation of bursa or tendons; may be infectious in etiology—especially olecranon and prepatellar areas (Septic Arthritis p340).
Epidem: Common.
Pathophys: Overuse or acute stress phenomenon; multifocal bursitis may be associated with homozygous homocystinuria (J Inherit Metab Dis 1999;22:185).
Sx: Pain of specific joint; remember referred pain, such as neck to any location in upper extremity, back to hip, hip to knee, etc.
Si: Pain with palpation in bursitis; pain with range of motion in tendonitis—have pt hold specific position in opposition to your force to isolate specific area; Finkelstein’s test in de Quervain’s tendonitis.
Crs: Acute with resolution within 2 wks or chronic, if more protracted.
Cmplc: Chronic pain.
Diff Dx: Arthritis; ligamentous sprain; rarely due to sea urchin spines that does not resolve until spines removed (Joint Bone Spine 2000;67:94); consider carpal tunnel syndrome for wrist pain syndromes, which is best treated with corticosteroid injection or splinting, and not NSAIDs (Ann Fam Med 2004;2:267).
Lab: Consider plain radiographs if suspicious for significant fracture. Consider needle aspiration if non-prosthetic joint to ascertain etiology.
Emergency Management:
Inject with anesthetic agent (lidocaine, bupivicaine) and steroids—pro study of anserine bursitis (South Med J 2000;93:207), equivocal for shoulder tendonitis (Scand J Rheumatol 1985;14:76) and perhaps neg for Achilles tendonitis (Clin J Sport Med 1996;6:245); tendonitis (such as de Quervain’s) does not require the injection to be in the tendon sheath to be effective.
Splinting of shoulder or elbow (tennis elbow) for example—if using sling, be sure to have daily shoulder movements to avoid adhesive capsulitis. Heel cup for plantar fasciitis or Achilles tendonitis (Brit J Sports Med 1981;15:117).
Ice for 24-48 hr.
Acetaminophen and NSAIDs about equal efficacy in traumatic situations (Curr Opin Rheumatol 2000;12:150), NSAIDs better in inflammatory realms (RA, gout, etc); im ketorolac as efficacious as po ibuprofen (Acad Emerg Med 1998;5:118; Ann EM 1995;26:117).
Dimethyl sulfoxide of no help (Med Sci Sports Exerc 1981;13:215).
16.2 Dislocations
Cause: Usually traumatic, although those with joint laxity due to connective tissue disorder may need minimal trauma. Less force needed for recurrent injuries. In peds, remember to consider child abuse. Consider complication of seizure.
Epidem: Variable.
Pathophys: If fracture of joint surface, may go on to arthritis.
Si: Tenderness; decreased to no range of motion of affected joint; deformity—palpate location of dislocated part; check distal neurovascular status; intra-articular edema.
Crs: Reduction curative, coincident fracture may prolong rehabilitation.
Cmplc: Fracture, neurovascular damage.
Lab: Plain radiographs—2 pictures 90° from each other. The Y-view in shoulder dislocations is key. Post-reduction views are standard, yet necessity in some areas [shoulder (Ann EM 1996;28:399)] has been questioned.
Emergency Management:
Iv access for pain control.
Local block such as digital, radial nerve, or median nerve, if feasible.
Ortho consult for all dislocations with neurologic or vascular compromise.
Procedural sedation with midazolam should be considered for reduction of large joints such as ankle, elbow, shoulder, etc.
Steady and gradual traction over 2-5 min is more effective than more force attempted quickly.
Get post-reduction films.
Specific examples:
Ankle: Obvious deformity should be reduced if possible to prevent skin tearing/breakdown—easiest to reduce ankle with both hip and knee flexed (to 90° if possible) so that muscles to the Achilles tendon are relaxed. Most of these have coincident fractures. Most fracture fragments will move during reduction, so patient should be well sedated so that there is minimal muscle tension during the maneuver to avoid injury to the articular cartilage.
Digit: Digital block, being sure to infiltrate the dorsal surface on the hand and the plantar surface on the foot to get a complete block. Reduction should first have outward traction in
the direction of the long axis of the dislocated phalanx. With other hand, move the base of the dislocated bone toward its natural position. Then move the long axis of the phalanx to its natural neutral position, so that the digit is now normally aligned.
Elbow: Five types of elbow dislocations:
Peds: Nursemaid elbow dislocations are pediatric dislocations of the radial head, and these are uncommon in adults. To reduce a pediatric nursemaid elbow, place your thumb over the radial head, extend the elbow and supinate the forearm, and then flex the forearm. A pop may be felt or heard.
Adult: The elbow may dislocate posteriorly (most common), anteriorly, laterally, medially, or the radius and ulna may diverge laterally and medially, respectively. Reduction may be accomplished with procedural sedation. Have an assistant anchor the humerus while distracting the elbow and guide the proximal forearm bones around the humeral condyles. Bring the elbow into flexion once the olecranon/radius is felt to re-seat, and apply posterior splint with elbow at 90° flexion. Ligamentous injury is common (Clin Orthop 1987:221), but conservative treatment is usually adequate (Clin Orthop 1987:165).
Hip: Done with Ortho, posterior dislocations are more common.
Knee: A true Ortho emergency, the popliteal artery as at large risk with a knee dislocation. Reduction should be done with ortho involved, splint in position of comfort. Consider arteriogram—perhaps half the patients with vascular injury will require emergent surgery, others with self-resolving spasm or intimal flap, for example, and may be able to advocate for watchful waiting.
N.B. The ballotable patella or other indications of effusion may not be present (as seen with isolated ligamentous injuries)
because the synovial membrane may be torn, and thus traumatic effusion is into the thigh and leg.
Patella: Lateral more common than medial. Completely extend knee which may reduce patella. If not, keep the knee extended while attempting the following. Put thumbs at medial edge if medial dislocation and lateral edge if lateral dislocation, and gently push toward anatomic alignment, may need to lift leading edge with fingers just a little.
Shoulder (Med Sci Sports Exerc 1984;16:444; Am J Emerg Med 1999;17:288): May dislocate anterior, inferior, or posterior. Associated compression fracture of the humeral head is called a Hill-Sachs deformity. Some general reduction principles:
The pt needs to be relaxed;
Distract the humerus so that the humeral head can slip past the glenoid rim;
Sometimes guiding the humeral head directly is needed as distraction is being applied;
Twenty milliliters of 1% lidocaine in the affected shoulder joint can bring about significant relief (sterile prep and injection) and decreases the need for intravenous sedation (J Bone Joint Surg [Am] 2002;84-A:2135);
Bring the arm to the pt’s side, elbow 90° of flexion, and immobilize in this position once reduction completed.
Anterior dislocation (Am J Emerg Med 1991;9:180): Methods include:
Weight (aka Stimson or Wait)—pt prone with 10 lbs. of weight wrapped to freely hanging arm, reduction accomplished over time—this is a good wilderness rescue technique. One variation is with pt sitting in chair with arm draped over backrest and hanging straight down (Injury 1992;23:479).
Hippocratic variation: patient supine and anchored with one sheet wrapped around affected axilla for countertraction and reducer grasps elbow, which is flexed to 90° with
forearm pointing to ceiling. Distract the humerus—original method was with physician’s heel in pt’s axilla as countertraction, but can either put other sheet around you and tie off to pt’s elbow and lean back, or just hold elbow in antecubital fossa firmly. Walk the humerus into abduction, and gently externally and internally rotate.
Scapular rotation (Ann EM 1992;21:1349): Pt prone (supine if necessary) (Ann EM 1996;27:92), weights in hand, rotate the inferior scapular pole medially and superiorly until reduced.
External rotation (Jacep 1979;8:528): Pt is supine, humerus is completely adducted, elbow at 90° with forearm pointing to ceiling, slowly and gently externally rotate the shoulder.
Walk (Milch) (J Trauma 1992;32:801): Pt supine, bring the arm from adduction with 90° elbow flexion to full abduction with external rotation, while gently walking it to this position.
The backstroke: Begin with pt supine, arm in adduction with elbow at 0°, gently walk the arm to 180° of forward flexion, as if doing a swimming backstroke.
Inferior dislocation (Instr Course Lect 1985;34:232): Significant trauma. Pt is supine; place the sheet over the shoulder for countertraction; the arm vector for reduction is approximately 180° abduction. May be truly irreducible with closed technique.
Posterior dislocation: Pt supine; vector for reduction is the long axis of humerus with arm adducted.
16.3 Fracture Management
Cause: Usually traumatic, possibly due to child abuse in children, or osteogenesis imperfecta (OI) as underlying cause in children with
multiple fractures and low intensity trauma, pathologic fractures in people with either neoplastic or other chronic diseases, such as TB in which the bone is abnormal, and more common in the elderly or in those with impaired mobility due to osteoporosis; a difficult diagnosis is that of stress fractures where repetitive forces may cause x-ray negative fractures. Be sure to screen the whole patient in the setting of multisytem trauma, and look for syncope or other co-morbid illnesses in the elderly or those with chronic diseases.
multiple fractures and low intensity trauma, pathologic fractures in people with either neoplastic or other chronic diseases, such as TB in which the bone is abnormal, and more common in the elderly or in those with impaired mobility due to osteoporosis; a difficult diagnosis is that of stress fractures where repetitive forces may cause x-ray negative fractures. Be sure to screen the whole patient in the setting of multisytem trauma, and look for syncope or other co-morbid illnesses in the elderly or those with chronic diseases.
Epidem: Common; perhaps increased osteoporosis risk in women with increased vitamin A intake based on hip fracture study (Nejm 2003;348:287, Jama 2002;287:47)
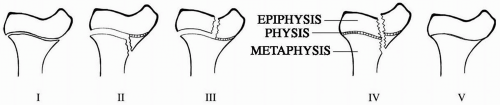
Pathophys: Bony anatomy core knowledge includes bony landmarks (the trochanteric area in the hip is the basis for our hip fracture descriptions, eg) and remembering that pediatric bones will a have growth plate (physis)—with regards to the physis, the segment at the end of the bone with the joint cartilage is called the epiphysis, and the segment toward the major portion of the bone mass is called the metaphysis. Transverse or oblique fractures usually due to uniform load without rotation, whereas spiral fractures associated with a rotational force to the bone. Children may have fractures involving the physis that are called Salter-Harris (SH) fractures (Am Fam Phys 1992;46:1180):
(Slip) SH I is a fracture through the complete physis and may not show on initial x-ray or may show as a slipping of the epiphysis relative to the metaphysis
(Aground) SH II is the physis with a portion of the metaphysis, in our picture is the bone on the bottom (aground) relative to the physis
(Lesser) SH III is a portion of the epiphysis and physis, in our picture is the bone with the lesser mass (epiphysis compared to metaphysis)
(Two) SH IV is an oblique fracture through the physis so that the fracture segment has both metaphysis and epiphysis—two (both) are involved
(Ram) SH V is a compression injury of the physis and may not show on initial x-ray, or may appear as the epiphysis rammed into the metaphysis.
When describing fractures, we need to be specific in the following areas:
Bone(s) involved
Displacement of bones from their usual anatomic location
Angulation from their normal anatomic angle
Secondary dislocation
Amount of skin tension or breach in skin overlying the fracture
Status of distal peripheral vascular and neurologic function
Specific Considerations:
Ottawa ankle rules (Jama 1993;269:1127)
Pts aged 16 years or older (Ped Emerg Care 2003;19:73; Acad Emerg Med 1999;6:1005) may have ankle or foot radiographs based on some basic triage criteria (100% sensitive for significant fracture), which are the following:
Injury < 10 d
Not a reassessment
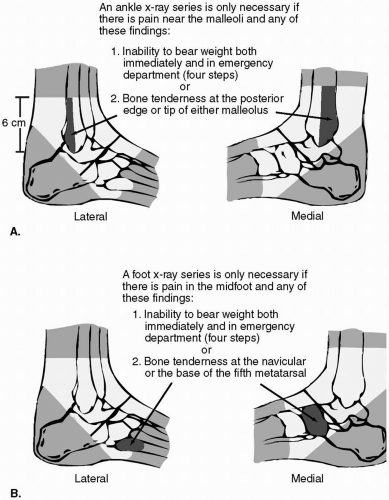 Figure 16.2 Ottawa Ankle Rules: A. Refined clinical decision rule for ankle radiographic series in ankle injury patients. B. Refined clinical decision rule for foot radiographic series in ankle injury patients. (Reproduced with permission from Stiell IG, et al., Decision rules for the use of radiography in acute ankle injuries. Jama 1993;269:1130.) |
Ottawa knee rule (Ann EM 1995;26:405; 2001;38:364)
Pts > 5 yr of age should have plain x-rays of the knee for acute knee injury for any of the following indications—in comparing these two rules (knee and ankle), knee injuries are unlike ankle injuries in that ligament injury and avulsion fractures may necessitate surgical intervention and thus, x-rays will usually be needed—and provides 95% sensitivity and specificity for detecting clinically significant fractures in adults (Jama 1996;275:611) and 100% sensitivity and approximately 43% specificity in children 5-16 yr of age (Ann EM 2003;42:48):
Age ≥ 55 yr old
Tenderness at head of fibula
Isolated patella tenderness
Inability to flex knee to 90°
Inability to bear weight for 4 steps immediately and in the ER.
Sx: H/o trauma; pain, usually with pinpoint location to affected bone; obvious deformity.
Referred pain—knee pain in hip fractures is common (Ann EM 1997;29:418).
Si: Tenderness; edema; ecchymoses; angulation; crepitus; tendon or ligamentous instability about specific joint; perhaps auscultatory percussion in hip fractures (Clin Orthop 1977:9)—place stethescope over the pubic symphysis, percuss over the patella one at a time, and an ipsilateral fracture should have decreased sound conduction.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree