Protocol for preoperative antiplatelet therapy with bare-metal stents (BMS).
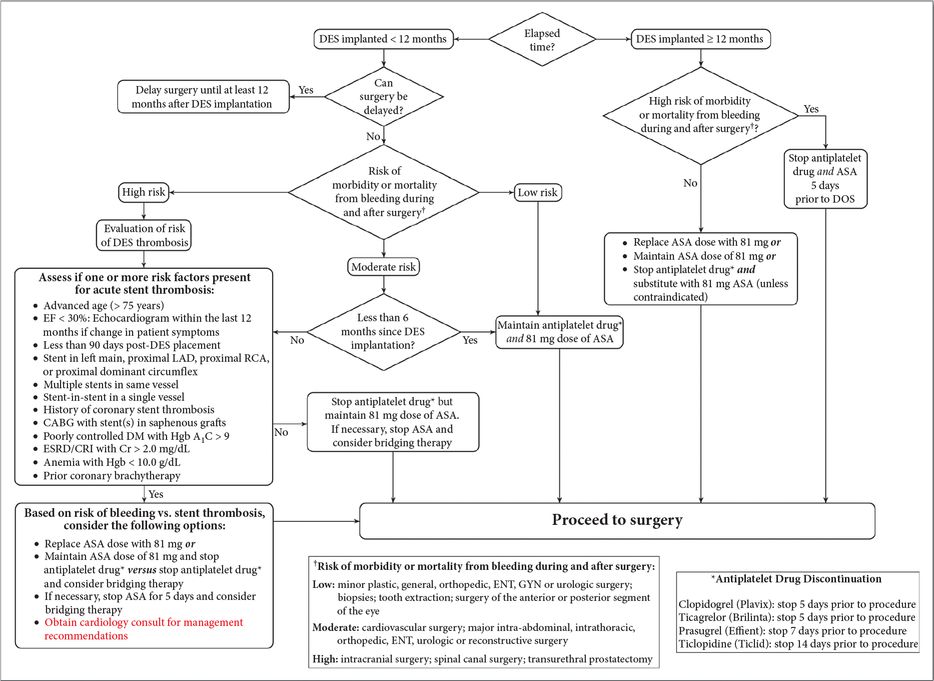
Protocol for preoperative antiplatelet therapy with drug-eluting stents (DES).
Antithrombotic or antiplatelet medications have direct impacts on regional anesthesia utilization. This information will be discussed in detail in another chapter.
3. Discuss potential anesthetic techniques for this patient
General or regional anesthesia may be utilized for shoulder surgery. Either an endotracheal tube (ETT) or laryngeal mask airway (LMA) may be used for airway management. The choice of ETT vs. LMA may be impacted by practitioner comfort, patient airway and habitus, operative time, and surgeon experience. Interscalene brachial plexus blockade may also be used as the sole anesthetic for shoulder surgery [27]. This is particularly successful when combined with propofol or dexmedetomidine [28].
4. Present the evidence for advantages and disadvantages of the use of an interscalene catheter for postoperative analgesia and recovery
When compared to opioid-based analgesia, interscalene brachial plexus blockade provides superior analgesia, opioid sparing, decreased nausea and vomiting, and improved patient satisfaction in patients undergoing shoulder surgery [29–31]. The advent of perineural continuous infusions has further improved postoperative outcomes. Patients receiving interscalene catheters meet hospital discharge criteria faster than patients who do not [32]. Continuous interscalene blockade may allow same-day discharge following total shoulder arthroplasty [33].
Risks and complications are associated with interscalene blocks. Anticipated side effects include ipsilateral phrenic nerve paralysis, Horner’s syndrome, and recurrent laryngeal nerve block. Neurologic, infectious, and systemic complications are also possible.
Neurologic complications
Current evidence suggests that the risk of clinically apparent nerve injury after total shoulder arthroplasty ranges from 0.8% to 4.3% [34]. Subclinical nerve injury, as characterized by changes in electromyographic activity, may be as high as 16.7 to 24% after shoulder arthroplasty, with an even higher risk in those patients who have preoperative neuropathy [35–36]. The use of an interscalene block does not appear to significantly increase the risk of brachial plexus injury. Brull and colleagues reported an incidence of neuropathic injury for all peripheral nerve blocks ranging from 0.02% to 2.8%; this incidence was highest after interscalene blockade [37]. Another report showed a neuropathy incidence of 2.3% after nerve stimulator-guided interscalene blockade, with complete resolution in 10 of 11 patients by six months [27]. One study found an incidence of sensory deficit of 7.9%, 3.9%, and 0.2% at one month, three months, and nine months after interscalene nerve blockade, respectively [38]. At three months, fewer than half of the affected patients had an identifiable etiology, ranging from carpal tunnel syndrome to brachial plexopathy and actual brachial plexus damage. An increased risk was not associated with an indwelling perineural catheter. Notably, the majority of all of these studies looked at nerve stimulator- guided techniques. Perhaps the largest prospective study to date addressing safety in ultrasound-guided interscalene blockade reported a 0.9% rate of neurologic complications, including three cases of postoperative brachial plexitis [31].
Patients with pre-existing neuropathy should be informed of the possible higher risk of nerve block-associated neuropathy and the benefits of the use of a peripheral nerve block should be weighed against the risk of exacerbated nerve injury. Some evidence suggests that patients with multiple sclerosis may have an increased risk [31, 39]. While potential mechanisms of injury are not well described, pathologic processes such as peripheral demyelination may play a role [40].
Infectious complications
Perineural catheter infections are rare, with an incidence of colonization and infection at 10.4% and 0.13%, respectively [41]. However, interscalene, femoral, and axillary catheters have been suggested as most likely to develop this complication [42]. Additionally, infection and abscess formation in the interscalene space can be catastrophic given the multiple neurovascular structures in close proximity. Like any indwelling perineural catheter, strict sterile technique should be used during placement. Additionally, vascular puncture and hematoma formation may increase this risk; neck cellulitis with subsequent septic shock has been described in this setting [43].
Systemic complications
Assuming use of an interscalene brachial plexus block and the sitting position, a hypotensive bradycardic response may occur. Severe hypotension and bradycardia was reported in 17% of patients undergoing shoulder surgery in the seated position [30]. The Bezold–Jarisch reflex is thought to be the mechanism for such a response. In this pathway, lower extremity venous pooling, exacerbated by the sitting position, decreases pressure on carotid sinus receptors, leading to a reflexive increase in cardiac contractility. A paradoxical parasympathetic discharge occurs, resulting in bradycardia. The presence of exogenous epinephrine, such as an additive in peripheral nerve blockade, may increase the incidence of this response [44], while beta blockade does not alter the incidence [45]. Exact mechanisms are not entirely clear.
References
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree




