The innervation of the elbow by all six peripheral nerve originating from the brachial plexus.
The literature dealing with pain associated with total elbow arthroplasty (TEA) mainly supports two different techniques used for postoperative pain control.
Cervical paravertebral block
All paravertebral blocks (cervical, thoracic, lumbar, and sacral) are performed at the root level where the roots are, to varying degrees, surrounded by dura mater; therefore these should be regarded as para-neuraxial epidural injections [3]. For an elbow procedure, C7 is targeted. A triceps motor response upon needle and catheter placement provides excellent postoperative pain control, while to a large extent preserving motor function and proprioception. For this procedure, more recently done with ultrasound (US) guidance, a 17 to 18G insulated Tuohy needle is used to minimize the possibility of penetrating the dura surrounding the nerve roots.
Continuous infraclavicular nerve block (CICB)
Another technique to treat pain associated with TEA is the CICB [4], which produces good pain control and satisfaction in ambulatory patients.
Traditional infraclavicular techniques used stimulating catheters [2], a bolus of 20 ml of 0.5% ropivacaine, and a postoperative infusion of 0.25% ropivacaine at 7 ml/h basal rate with a patient-controlled bolus of 3 ml every hour [4]. The CICBs can be inserted in-plane with the goal of needle tip placement posterior to the subclavian artery [5].
Ultrasound guidance has been used to aid needle placement in recent years. To manage the common problem of secondary block failure that may occur with any catheter, some have advocated dual catheter placement; leaving perineural catheters at the medial cord at the infraclavicular level and the superior trunk at the interscalene level [6].
Early documented perineural catheters were placed by performing a cut-down on the brachial artery in the axilla and threading a catheter cephalad until stopped where the artery crossed the first rib under the clavicle [7]. This was successful and clinicians have mimicked and modernized this technique by inserting infraclavicular catheter from a distal and lateral approach through the use of US [8]. After identifying the lateral, medial, and posterior cords as they cross the first rib, a catheter may be placed between the three cords (Figure 21.2).
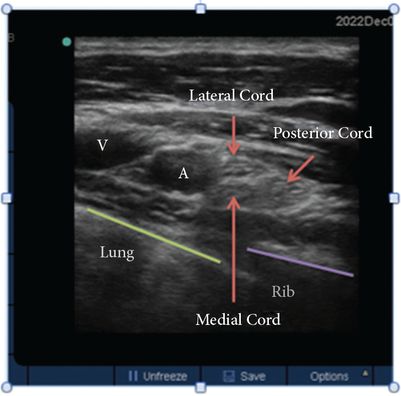
Ultrasound image of the proximal infraclavicular area. (A) is axillary artery, and (V) axillary vein. All three cords (medial, lateral, and posterior) are adjacent to the artery and in close proximity to each other, and, similar to the femoral nerve in the lower extremity, lateral to the artery and vein. The position of the rib and lung can also be seen.
For this technique, a US probe is placed parallel and inferior to the clavicle to obtain the image of all three cords in one view as they cross the first rib. An insulated Tuohy needle is inserted out of plane to the probe, just caudad to the coracoid process, such that the tip of the needle ends up between these three cords. The goal is to have the local anesthetic bathe all of them (Figure 21.3). The use of nerve stimulation in addition to US can assist in needle and catheter placement [9].
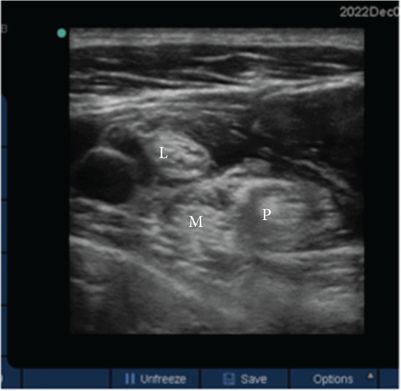
Ultrasound image of the proximal infraclavicular area after a local anesthetic bolus had been injected with all three cords: lateral cord (L), posterior cord (P), and medial cord (M) covered by the local anesthetic.
2. Describe the typical postoperative recovery
Over the past three decades, orthopedic surgeons have seen great advancement in the technology available to them for TEA [10]. Earlier cases were primarily for rheumatoid arthritis, but recent improvements in arthroplasty equipment has paved the way for surgeons to use TEAs for other indications, such as in patients who have suffered trauma [10]. When compared with other joint replacement surgeries, TEA carries relatively high complication and reoperation rates. In their report, Park et al. show a complication rate of 44% over a 13-year follow-up period, but rates vary based on the various indications for surgery [11]. Furthermore, as surgeons expand the use of TEA for trauma, the average age of the patients decreases and the expected life span of the implants will need to increase.
The majority of patients who undergo TEA do so for pain or decreased mobility of the joint resulting in disability. Most surgeons view this surgery as a last resort when other treatment modalities have failed. In the long term, most patients report improvement in pain and functional status [10]; although, satisfaction has been reported as less than 70% in patients following fractures [12]. Another study retrospectively reviewed 21 TEAs over 55 months and showed improvements in patients’ Mayo Elbow Performance Score, from a mean of 40 to 89 [13]. This score provides an excellent metric because it measures pain, motion, stability, and function.
In the immediate postoperative phase, however, the main concerns are wound breakdown, infection, and pain. The risk of wound dehiscence is so great that physical therapy is often delayed postoperatively for two to three weeks because the patients remain with their arm in a splint during this time. Patients’ arms are splinted not only for comfort but also for protection, while a continuous brachial plexus block is in place. The Brigham and Women’s Hospital TEA protocol, often followed by surgeons and physical therapists, encourages the patient to do exercises of the neck plus surrounding joints of the shoulder and wrist, but not the elbow [14].
After the acute postoperative period, physical therapy revolves around passive range of motion. This is done with attention to the wound as there is the risk of dehiscence and infection with motion at the joint. After six to eight weeks, patients begin more comprehensive physical and occupational therapy programs with emphasis on activities of daily living. Weight lifting is often limited to 5 to 15 lb (2.3 to 6.8 kg) and attention to the wound remains critical. After 12 weeks, the aim for range of motion is 120 degrees of flexion and full extension. Weight lifting is still limited to less than 15 lb (6.8 kg), and the emphasis on therapy is on functionality of daily living.
3. Debate if regional or general anesthesia alters postoperative recovery
Traditionally, patients undergoing TEA remained in the hospital for several days. Length of stay now varies greatly based on pre-existing comorbidities. The main reason for hospitalization for the first 24 hours postoperatively is for pain control and intravenous opioids may be required for up to one week in some patients.
In 2006, Ilfeld et al. reported some success in having carefully selected patients be discharged home from the post-anesthesia care unit (PACU) [14]. In this series the patients had to meet stringent discharge criteria and their pain was managed by a preoperatively placed infraclavicular catheter dosed with 40 ml of mepivacaine with epinephrine. All patients then underwent general anesthesia and postoperatively had ambulatory infusion pumps with 0.25% ropivacaine that were set to infuse at 7 ml/h with patient-controlled boluses of 3 ml limited to one bolus per hour. Although only one patient was actually discharged to home from the PACU, this study set the tone for further use of perineural brachial plexus catheters as a means to provide pain control with the possibility of shorter hospital stays. Similarly, many institutions now hospitalize patients overnight and ensure their pain control is adequate with multimodal analgesics and a peripheral nerve block catheter.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree




