Inhibitors
Inducers
Quinidine
Phenobarbital
Cimetidine
St. John’s wort
Ketoconazole
Phenytoin
Fluconazole
Carbamazepine
Metronidazole
Rifampin
Grapefruit juice
Cigarette smoking
Erythromycin
Pioglitazone
Paroxetine
Oxcarbazepine
Fluoxetine
Amiodarone
Simvastatin
5.2.3 Safety Warnings
In 2006, the FDA released a public safety advisory after a trend of methadone-related deaths in patients treated for nonmalignant pain [9]. A black box warning from the manufacturer was then issued. This warning identifies severe respiratory depression as the most problematic side effect of methadone. The warning also exposes the risk of fatal arrhythmia (torsades de pointes) and QT prolongation with methadone treatment. These events were reported in patients treated for pain with large, daily doses of methadone. But patients taking conventional doses for opioid detoxification and maintenance were not excluded from these risks [9, 10] (Table 5.2).
Table 5.2
Risk factors for QTc prolongation and torsades de pointes
QTc prolongation | Torsades de pointes |
|---|---|
Genetic disposition | Concurrent use of one or more QT interval prolonging drugs |
Electrolyte abnormalities | Congenital prolonged QT |
Liver disease | QTc interval greater than 500 ms |
Thyroid disease | Electrolyte abnormalities |
Advanced age | History of torsades de pointes |
Female gender | A-V node dysfunction and bradyarrhythmias |
Structural heart disease | Ischemic heart disease and congestive heart failure |
Medication induced | Advanced age |
Illicit drug use | Recent conversion from atrial fibrillation |
5.2.4 Cardiac Manifestations
Methadone can cause serious cardiac conduction effects, including QT interval prolongation and torsades de pointes [11]. A host of common cardiac and non-cardiac medications as well as electrolyte disturbances can prolong the QT interval. QT prolongation can be inherited as well as acquired. All forms cause abnormal repolarization leading to altered refractory periods in the heart. Patients with prolonged QT interval are especially prone to syncope or even sudden death during periods of stress or sympathetic stimulation because of deranged repolarization [12]. Rate-corrected QT (QTc) greater than 450 ms is considered prolonged, and >500 ms is associated with an increased risk for sudden death [13]. Generally, the QTc is slightly longer in women [14].
In a review of patients on methadone therapy, the prevalence of QTc interval prolongation ranged from 0.5 to 31% based on a threshold of >430 to 450 ms in men and >460 to 470 ms in women [10, 12, 15–18]. The proportion of patients who exceeded a QTc >500 ms ranged from 0 to 6% in six studies [10, 13, 16, 19–21]. Higher methadone doses were associated with greater prolongation of QTc interval after controlling for other confounding factors [10, 12, 18, 19, 22, 23]. Patients who took high daily doses had torsades de pointes [22, 24].
5.2.5 Torsades de Pointes
Torsade de pointes is a polymorphic ventricular tachycardia that can lead to sudden death. It is characterized by a gradual change in the amplitude and twisting of the QRS around the isoelectric line. What differentiates it from generic ventricular tachycardia is the prolonged QT interval. Quite often, the arrhythmia terminates spontaneously and comes in bursts. Because the rhythm is not usually sustained, the patient’s baseline QT prolongation may be seen on the rhythm strip. In certain cases, prolongation may evolve into ventricular fibrillation. Ventricular rates can vary from 150 to 250 bpm, and patients may be completely asymptomatic (Fig. 5.1).
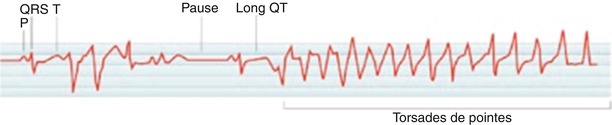
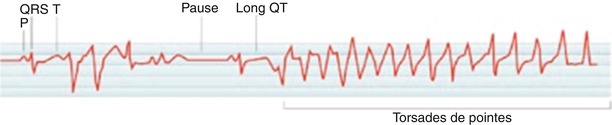
Fig. 5.1
Electrocardiogram of torsades de pointes
5.2.6 Treatment
Recognizing torsade de pointes and differentiating it from generic ventricular tachycardia is important. Certain conventional antiarrhythmic agents will be ineffective and can even exacerbate the arrhythmia. For example, group IA antiarrhythmic drugs will prolong the QT interval and thus worsen the torsades [25]. Goals of treatment are aimed at shortening the QT interval. Modalities of therapy include cardiac pacing, intravenous atropine, and isoproterenol infusion. The treatment that has gained in popularity and has proven to be extremely efficacious is intravenous magnesium sulfate. Synchronized cardioversion may be ineffective because the abnormal rhythm is polymorphic. Unsynchronized shock or defibrillation may be necessary.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree






