REASONING:
This question tests knowledge of the pathophysiology associated with burn injury and its effects on the pharmacokinetics of muscle relaxants. It is challenging because the wording used in choice D attempts to lead you down a path that is clearly wrong once the choice is examined carefully. Burned muscle tissue does not regenerate acetylcholine receptors. Rather, the sites of healthy tissue (both intra- and extrajunctional) have been correlated with increased expression of acetylcholine receptors. Choices B and C can be eliminated because they do not significantly affect the pharmacokinetics of muscle relaxants. Choice A is the best answer because the direction of association is correct (increased protein binding leading to decreased drug potency), and the pharmacokinetics involved relate directly to drug potency. It is important to note that depolarizing muscle relaxants should not be administered to burn patients after the first 24 hours (owing to proliferation of acetylcholine receptors) because they can cause severe hyperkalemia leading to cardiac arrest. This effect is thought to peak 20 to 90 days after the injury but has been reported to persist for up to 2 years.
BIBLIOGRAPHY:
Bonate PL. Clinical pharmacology of muscle relaxants in patients with burns. Clin Pharmacokinet. 1980;5(6):548-556.
Gronert GA. A possible mechanism of succinylcholine-induced hyperkalemia. Anesthesiology. 1980;53(4):356.
Gronert GA, Dotin LN, Ritchey CR, Mason AD, Jr. Succinylcholine-induced hyperkalemia in burned patients, part II. Anesth Analg. 1969;48(6):958-962.
Gronert GA, Theye RA. Pathophysiology of hyperkalemia induced by succinylcholine. Anesthesiology. 1975;43(1):89-99.
Jaede U, Sorgel F. Clinical pharmacokinetics in patients with burns. Clin Pharmacokinet. 1995;29(1):15-28.
Leibel WS, Martyn JA, Szyfelbein SK, Miller KW. Elevated plasma binding cannot account for the burn-related D-tubocurarine hyposensitivity. Anesthesiology. 1981;54(5):378-382.
Loirat P, Rohan J, Baillet A, et al. Increased glomerular filtration rate in patients with major burns and its effect on the pharmacokinetics of tobramycin. N Engl J Med. 1978;299(17):915-919.
Marathe PH, Dwersteg JF, Pavlin EG, et al. Effect of thermal injury on the pharmacokinetics and pharmacodynamics of atracurium in humans. Anesthesiology. 1989;70(5):752-755.
Martyn J, Goldhill DR, Gousouzian NG. Clinical pharmacology of muscle relaxants in patients with burns. Clin Pharmacol. 1986;26(8):680-685.
Martyn JA, Matteo RS, Greenblatt DJ, et al. Pharmacokinetics of D-tubocurarine in patients with thermal injury. Anesth Analg. 1982;61(3):241-246.
Martyn JA, Matteo RS, Szyfelbein SK, Kaplan RF. Unprecedented resistance to neuromuscular blocking effects of metocurine with persistence after complete recovery in a burned patient. Anesth Analg. 1982;61(7):614-617.
Morgan GE, Mikhail MS, Murray MJ. Clinical Anesthesiology. 3rd ed. New York, NY: McGraw-Hill; 2002:803, 190 (Table 9-7 Diseases With Altered Responses to Muscle Relaxants).
Schaner PJ, Brown RL, Kirksey TD, et al. Succinylcholine-induced hyperkalemia in burned patients, part I. Anesth Analg. 1969;48(5):764-770.
Viby-Mogensen J, Hanel HK, Hansen E, et al. Serum cholinesterase activity in burned patients. Acta Anaesthesiol Scand. 1975;9(3):159-179.
BOOK B: QUESTION 2
Answer D
QUESTION (Choose single best answer):
Which of the following parts of the infant’s airway determines the appropriate diameter of a nasotracheal tube?
Pediatrics
(A) Nares.
(B) Glottis.
(C) Vocal cords.
(D) Cricoid cartilage.
(E) Third tracheal ring.
CORRECT ANSWER: D
SUMMARY:
The infant larynx has a funnel shape and is narrowest at the level of the cricoid cartilage. The cricoid cartilage size determines the diameter of both oral and nasal endotracheal tubes with a leak pressure of 20 to 30 cmH2O being adequate. Too small a tube size with excessive leak can impede ventilation, while too large a tube can cause mucosal trauma and airway edema. New evidence shows that the adult airway is not narrowest at the level of the glottic opening, but actually at the level of the cricoid cartilage in most adults. Ultrasound imaging of the pediatric cricoid cartilage can aid in determining proper endotracheal tube size.
EXPLANATION:
(A) Incorrect. The diameter of the nares must accommodate the outer diameter of a nasal endotracheal tube, but it is not, in fact, a determinant of tube diameter.
(B) Incorrect. The glottic opening is larger than the subglottic area in infants due to the funnel shape of the infant airway. Previously, the glottic opening was thought to be the narrowest portion of the adult airway, but adult cadaveric data have shown that the cricoid cartilage is the narrowest portion of the airway in about 70% of adults.
(C) Incorrect. The distance between the vocal cords is larger than the cricoid cartilage diameter in both infants and in most adults.
(D) Correct. The infant larynx is funnel shaped and is narrowest at the level of the cricoid cartilage. Multiple formulae exist for estimating proper pediatric endotracheal tube diameter and length, including height, weight, and age. Recently, the use of preinduction ultrasound-guided imaging of the pediatric cricoid cartilage in determining proper endotracheal tube size has been validated.
(E) Incorrect. This part of the trachea is below the cricoid cartilage and is not involved in endotracheal tube selection.
REASONING:
Choice A is tempting, but the cricoid cartilage, ultimately, is the determinant of any endotracheal tube diameter, whether oral or nasal. Choices B and C can be eliminated because both the cords and glottic opening are larger than the cricoid cartilage diameter due to the funnel shape of the infant larynx. Choice D plays no role in tube selection. An excessively small endotracheal tube can contaminate the operating room with volatile anesthetic and decrease ventilation of the infants lungs, while an excessively large-tube diameter can damage airway mucosa and lead to postextubation croup or stridor.
BIBLIOGRAPHY:
Miller RD, Eriksson LI, Fleisher LA, Wiener-Kronish JP, William YL. Miller’s Anesthesia. 7th ed. Philadelphia, PA: Churchill Livingstone; 2010:2562, 2578 (Table 82-6 Recommended Sizes and Distance of Insertion of Endotracheal Tubes and Laryngoscope Blades for Use in Pediatric Patients).
Morgan GE, Mikhail MS, Murray MJ. Clinical Anesthesiology. 4th ed. New York, NY: McGraw-Hill; 2006:936.
Shibasaki M, Nakajima Y, Ishii S, et al. Prediction of pediatric endotracheal tube size by ultrasonography. Anesthesiology. 2010;113(4):819-824.
BOOK B: QUESTION 3
Answer C
QUESTION (Choose single best answer):
Administration of 200 mEq of sodium bicarbonate during cardiopulmonary resuscitation is associated with
Pharmacology
(A) Cerebrospinal fluid (CSF) alkalosis.
(B) Hypercalcemia.
(C) Hypercarbia.
(D) Hyperkalemia.
(E) Shift of the oxyhemoglobin dissociation curve to the right.
CORRECT ANSWER: C
SUMMARY:
Administration of sodium bicarbonate is associated with CO2 production owing to neutralization of H+ ion, which initially produces carbonic acid. It is immediately broken down to CO2 and water. Other effects include metabolic alkalosis, hypernatremia, hyperosmolarity, and leftward shift of the oxyhemoglobin dissociation curve.
EXPLANATION:
(A) Incorrect. CO2 produced from bicarbonate administration causes CSF acidosis from rapid passage of CO2 across cell membranes.
(B) Incorrect. Alkalosis produces hypocalcemia by altering the equilibrium of ionized and bound calcium.
(C) Correct. The neutralization of hydrogen ion produces carbonic acid that immediately dissociates to CO2 and water. CO2 is eliminated in the lungs through expiration. Inadequate alveolar ventilation can result in hypercarbia and worsening acidosis.
(D) Incorrect. Alkalosis produces hypokalemia.
(E) Incorrect. Sodium bicarbonate administration produces alkalosis, resulting in a leftward shift of oxyhemoglobin curve.
REASONING:
This question is challenging because two choices, A and C, seem like plausibly correct choices. Most readers recognize that sodium bicarbonate administration causes an elevation in serum bicarbonate, leading to alkalosis. Most readers also recognize that sodium bicarbonate administration is associated with a transient hypercarbia. The key to this question is that choice A refers to CSF, and not serum alkalosis, which makes it incorrect. C is the best answer.
BIBLIOGRAPHY:
Barash PG, Cullen BF, Stoelting RK, Cahalan M, Stock M. Clinical Anesthesia. 6th ed. Philadelphia, PA: Lippincott Williams & Wilkins; 2009:293, 1544.
Morgan GE, Mikhail MS, Murray MJ. Clinical Anesthesiology. 4th ed. New York, NY: McGraw-Hill; 2006:562-563, 682, 719.
BOOK B: QUESTION 4
Answer C
QUESTION (Choose single best answer):
When compared with diazepam, midazolam
Pharmacology
(A) Metabolites contribute more significantly to the sedative effect.
(B) Elimination is less dependent on hepatic metabolism.
(C) Has more predictable action after intramuscular administration.
(D) Produces less respiratory depression.
(E) Produces less hypotension during induction of anesthesia with opioids.
CORRECT ANSWER: C
SUMMARY:
The differences between midazolam and diazepam are tested frequently on board examinations. These drugs differ primarily in onset and duration of action, route of administration, extent of biotransformation to active metabolites, and suitability for use in the intraoperative setting. Midazolam is a highly protein-bound benzodiazepine that is suitable for intravenous, oral, and intramuscular administration. It is associated with rapid onset of action and elimination, lack of active metabolites, and significant respiratory depression at higher dosages, especially in elderly patients. Diazepam is suitable for oral and intravenous administration but not for intramuscular usage owing to pain at the site of injection and unreliability of action when given via the intramuscular route. Diazepam has active metabolites that prolong its duration of action. The duration of action of both diazepam and midazolam is dependent on hepatic clearance.
EXPLANATION:
(A) Incorrect. Diazepam metabolites contribute more significantly to the sedative effect. Midazolam has virtually no active metabolites.
(B) Incorrect. Both midazolam and diazepam are dependent on hepatic metabolism for clearance. They both undergo oxidation and conjugation reactions in the liver prior to clearance. These reactions are affected most commonly by age, cirrhosis, and coadministration of other drugs (especially those metabolized by the cytochrome P-450 enzyme system).
(C) Correct. Midazolam has a much more reliable onset and action when given intramuscularly than diazepam. Diazepam is also painful on injection.
(D) Incorrect. Midazolam is associated with greater respiratory depression because of increased potency of the drug compared with diazepam. After initial Food and Drug Administration (FDA) approval of midazolam, there were deaths related to inadvertent overdosing that led to fatal respiratory depression. A decrease in the dosing recommendations as well as unit repackaging ensued.
(E) Incorrect. Benzodiazepines and high-dose narcotics have been reported to produce hypotension during induction for coronary bypass surgery. A study by Liang and colleagues found no significant differences in hemodynamic changes associated with induction of anesthesia with fentanyl (5 μg/kg) and midazolam (0.3 mg/kg) versus fentanyl (5 μg/kg) and diazepam (0.3 mg/kg).
REASONING:
This is a somewhat challenging question that reflects the often-tested pharmacodynamic and pharmacokinetic comparisons between midazolam and diazepam. The reader should ensure that these differences are understood clearly. Choice D can be eliminated with knowledge of midazolam’s sixfold increased intrinsic potency compared with diazepam. One might also have used this knowledge to exclude choice E. Knowledge of the Liang study similarly would have excluded choice E. Similarly, choice A can be eliminated if the reader recalls that diazepam has two active metabolites, whereas midazolam does not have any. Choice B is incorrect because all benzodiazepines are dependent on hepatic clearance for elimination. This leaves choice C, which makes empirical sense because diazepam is not given intramuscularly in the clinical setting.
BIBLIOGRAPHY:
Buhrer M, Maitre PO, Crevoisier C, Stanski DR. Electroencephalographic effects of benzodiazepines: II. Pharmacodynamic modeling of the electroencephalographic effects of midazolam and diazepam. Clin Pharmacol Ther. 1990;48(5):555-567.
Liang SW. Studies of midazolam, diazepam and thiopentone on respiratory and cardiovascular function during induction anesthesia. Zhonghua Wai Ke Za Zhi. 1991;29(3):161-164, 205.
Miller RD, Miller ED, Reves JG, et al. Anesthesia. 7th ed. New York, NY: Churchill Livingstone; 2009.
Morgan GE, Mikhail MS, Murray MJ. Clinical Anesthesiology. 4th ed. New York, NY: McGraw-Hill; 2006.
Mould DR, DeFeo TM, Reele S, et al. Simultaneous modeling of the pharmacokinetics and pharmacodynamics of midazolam and diazepam. Clin Pharmacol Ther. 1995;58(1):35-43.
Tuman KJ, McCarthy RJ, el-Ganzouri AR, et al. Sufentanil-midazolam anesthesia for coronary artery surgery. J Cardiothorac Anesth. 1990;4(3):308-313.
BOOK B: QUESTION 5
Answer A
QUESTION (Choose single best answer):
Which of the following statements concerning a patient who has been receiving nitroprusside for several days is true?
Pharmacology
(A) Biotransformation of cyanide requires a sulfur donor.
(B) Formation of methemoglobin increases cyanide toxicity.
(C) Increased serum thiocyanate concentrations are innocuous.
(D) Mixed venous Po2 decreases as cyanide toxicity develops.
(E) Serum thiocyanate concentrations reflect the degree of cyanide toxicity.
CORRECT ANSWER: A
SUMMARY:
Sodium nitroprusside (SNP) is metabolized to cyanide ions, which can combine with methemoglobin, thiosulfate, or cytochrome oxidase. It is the interaction with cytochrome oxidase that interrupts cellular respiration. This leads to anerobic respiration and accumulation of lactic acid, acidosis, and increased mixed venous oxygen owing to a cellular inability to use oxygen. Untreated, this process eventually causes cell death. Toxic blood cyanide levels (> 100 mg/dL) are associated with greater than 1 mg/kg SNP infused over 2 hours or more than 0.5 mg/kg/h administered within 24 hours.
EXPLANATION:
(A) Correct. Cyanide ions are metabolized by rhodanase enzyme present in the liver and kidney to produce thiocyanate. Rhodanase requires thiosulfate ions as sulfur donors to catalyze this reaction.
(B) Incorrect. The nitroprusside moiety breaks down to yield five cyanide radicals and one NO molecule. These cyanide radicals can be cleared by one of the three mechanisms. CN can combine with methemoglobin to give cyanomethemoglobin. Therefore, formation of methemoglobin does not increase cyanide toxicity. On the contrary, it leads to safe elimination of cyanide.
(C) Incorrect. Elevated thiocyanate levels (5-10 mg/dL) can cause central nervous system (CNS) abnormalities.
(D) Incorrect. Mixed venous Po2 increases because CN– prevents use of oxygen as the final electron acceptor in the electron transport pathway involved with cellular respiration.
(E) Incorrect. Thiocyanate is cleared by the kidney. Its accumulation in renal failure produces toxicity characterized by nausea, muscle weakness, altered mental state, and thyroid dysfunction. Kidney or liver disease does not increase the likelihood of cyanide toxicity.
REASONING:
A commonly tested complication to chronic SNP infusion is the potential for toxicity related to cyanide and thiocyanate. It should be noted that toxicity is unlikely if a constant rate infusion is kept below 0.5 μg/kg/min (for chronic infusion, ie, > 3 hours). For infusions of short duration, the dose can go up to 8 to 10 μg/kg/min. Cyanide toxicity occurs by interfering with mitochondrial respiration. This produces acidosis, increased mixed venous oxygen saturation, and ultimately death. Increasing dose requirements to achieve pharmacologic effect (tachyphalaxis) may be the first clue to the onset of cyanide toxicity. Treatment consists of termination of the SNP infusion, ventilation with 100% oxygen, and infusion of thiosulfate (as a sulfur donor) and sodium nitrate (to produce methemoglobin). Administration of hydroxocobalamine instead of thiosulfate is recommended in patients with coexisting renal failure.
BIBLIOGRAPHY:
Barash PG, Cullen BF, Stoelting RK Cahalan M, Stock M. Clinical Anesthesia. 4th ed. Philadelphia, PA: Lippincott Williams & Wilkins; 2001:773-775 (Figure 28-13).
Morgan GE, Mikhail MS, Murray MJ. Clinical Anesthesiology. 4th ed. New York, NY: McGraw-Hill; 2006.
Stoelting RK. Pharmacology and Physiology in Anesthetic Practice, 3d ed. Philadelphia, Lippincott Williams & Wilkins, 1999, p. 316.
BOOK B: QUESTION 6
Answer C
QUESTION (Choose single best answer):
Which of the following increases the cephalad spread of hyperbaric intrathecal local anesthetics?
OB/Regional
(A) Cephalad-directed needle bevel.
(B) Coughing.
(C) Lithotomy position.
(D) Obesity.
(E) Rapid injection.
CORRECT ANSWER: C
SUMMARY:
Hyperbaric local anesthetic solutions are by definition denser than CSF, and their distribution therefore is governed largely by gravity. Patient position is one of the most important factors in the spread of these agents, especially the Trendelenburg, lateral, and jackknife positions. Factors that affect the spread of local anesthetics include age, height, direction of the needle opening during injection (dependent on needle type, ie, Whitacre), anatomic configuration of the spinal column, site of injection, volume and density of CSF, dosage of anesthetic, and volume of anesthetic solution. Factors that have been shown to have limited clinical importance include gender, direction of the needle bevel, turbulence, composition of CSF, CSF pressure, CSF circulation, addition of vasoconstrictors, and weight of the patient.
EXPLANATION:
(A) Incorrect. When studied, the direction of the needle bevel had no effect on the distribution of local anesthetic in the CSF. When a solution is injected through a standard beveled lumbar puncture needle, the solution exits in a straight line regardless of the needle bevel direction. Exceptions to this may be the Whitacre and Tuohy needles, which have different bevel openings, but the question does not specifically ask about these types of needles.
(B) Incorrect. Although CSF pressure increases with coughing, studies demonstrate that it does not have an effect on the spread of local anesthetic.
(C) Correct. Although other patient positions have a significant effect on spread of hyperbaric local anesthetics, lithotomy position does not. Lithotomy position may remove the pooling effect of the lumbar lordosis on local anesthetic distribution, but the thoracic kyphosis decreases cephalad spread.
(D) Incorrect. Weight does not have an effect on local anesthetic spread. This question was written prior to information generated by a 2011 paper by Carvalho et al, which showed that weight had no dependence on block height for cesarean delivery using modest doses of bupivacaine. This is no longer a valid answer.
(E) Incorrect. When studied, the level of sensory anesthesia was the same with varying injection rates up to 0.5 mL/s.
REASONING:
This question had many possible choices, including some that are intuitively correct but have been refuted when studied. Because hyperbaric solutions will follow gravity, choice A could be eliminated. Choices B and E are controversial at best and refuted in many studies. D has also been refuted in a recent study. C is the correct answer due to gravity-dependent distribution of local anesthetic.
BIBLIOGRAPHY:
Barash PG, Cullen BF, Stoelting RK, Cahalan M, Stock M. Clinical Anesthesia. 6th ed. Philadelphia, PA: Lippincott Williams & Wilkins; 2010:937-941.
Carvalho B, Collins J, Drover DR, et al. ED(50) and ED(95) of intrathecal bupivacaine in morbidly obese patients undergoing cesarean delivery. Anesthesiology. 2011;114(3):529-535.
Morgan GE, Mikhail MS, Murray MJ. Clinical Anesthesiology. 4th ed. New York, NY: McGraw-Hill; 2006:305-308, 305, (Table 16-2 Factors Affecting the Level of Spinal Anesthesia).
Singh SI, Morley-Forster PK, Shamsah M, et al. Influence of injection rate of hyperbaric bupivacaine on spinal block in parturients: a randomized trial. Can J Anaesth. 2007;54(4):290-295.
BOOK B: QUESTION 7
Answer B
QUESTION (Choose single best answer):
Compared with a patient without liver disease, a patient with cirrhosis will have
Pharmacology
(A) Greater accumulation of vecuronium with infusion.
(B) Increased unbound plasma vecuronium concentration.
(C) More frequent occurrence of phase II block after succinylcholine administration.
(D) Prolonged elimination half-life of atracurium.
(E) Unchanged volume of distribution for pancuronium.
CORRECT ANSWER: B
SUMMARY:
Vecuronium is metabolized by the liver to a limited extent. It is cleared largely by biliary excretion and to a small extent by renal excretion (25%). Muscle relaxants are water-soluble drugs with increased volume of distribution in disease states such as liver or renal failure. Multiple factors affect dose and duration of action of neuromuscular blocking agents.
EXPLANATION:
(A) Incorrect. Vecuronium is metabolized by the liver to a limited extent, but, according to Miller’s Anesthesia, “has been shown to have decreased clearance, a prolonged elimination half-life, and a prolonged neuromuscular blockade in patients with cirrhosis.” The increased volume of distribution can also contribute to a longer-elimination half-life. According to Clinical Anesthesiology, “the duration of action of vecuronium is usually not significantly prolonged in patients with cirrhosis unless doses greater than 0.15 mg/kg are given.” It seems that at usual clinical doses, accumulation of vecuronium is not clinically significant, making answer choice B a better selection.
(B) Correct. Vecuronium exhibits a moderate to high protein-binding capacity of 60% to 80%. Cirrhosis usually is accompanied by hypoalbuminemia, leading to increased plasma concentration of the unbound drug.
(C) Incorrect. Decreased levels of pseudocholinesterase that occur in liver disorders produce prolonged phase I block.
(D) Incorrect. Atracurium is degraded primarily by the Hofmann reaction and nonspecific ester hydrolysis, with less than 10% being excreted unchanged by renal and biliary routes. Thus its elimination is independent of renal or hepatic function.
(E) Incorrect. Liver failure produces increased volume of distribution for water-soluble drugs such as pancuronium. Thus there is a need for larger initial dose and less frequent maintenance doses in these patients.
REASONING:
This question is challenging because two choices, A and B, are plausibly correct. Greater drug accumulation plausibly can occur in patients with impaired hepatic elimination. However, the high protein-binding capacity of vecuronium, coupled with the knowledge that the duration of action is usually not significantly prolonged in cirrhotic patients, makes B the best answer.
BIBLIOGRAPHY:
Barash PG, Cullen BF, Stoelting RK, Cahalan M, Stock M. Clinical Anesthesia. 6th ed. Philadelphia, PA: Lippincott Williams & Wilkins; 2009:509, 1272.
Miller RD, Eriksson LI, Fleisher LA, et al. Anesthesia. 7th ed. New York, NY: Churchill Livingstone; 2010:2139-2140.
Morgan GE, Mikhail MS, Murray MJ. Clinical Anesthesiology. 4th ed. New York, NY: McGraw-Hill; 2006:220, 223-224, 795.
BOOK B: QUESTION 8
Answer E
QUESTION (Choose single best answer):
Intrathecally administered opioids exert their analgesic effects primarily in the
Pharmacology
(A) Brain stem.
(B) Fourth ventricle.
(C) Spinal nerve roots.
(D) Spinothalamic tracts.
(E) Substantia gelatinosa.
CORRECT ANSWER: E
SUMMARY:
Opioids are administered in the intrathecal or epidural space to manage acute or chronic pain. Intrathecal opioids produce analgesia by binding to opioid receptors, mostly μ-receptors, in the substantia gelatinosa (Rexed’s lamina II) located in the dorsal horn of the spinal cord. In contrast to intravenous administration of opioids, intrathecal opioids are not associated with sympathetic nervous system denervation, skeletal muscle weakness, or loss of proprioception.
EXPLANATION:
(A) Incorrect. See above.
(B) Incorrect. See above.
(C) Incorrect. See above.
(D) Incorrect. See above.
(E) Correct. Opioid receptors are nonuniformly distributed throughout the CNS. However, the primary site of action of intrathecal opioids is the substantia gelatinosa because of its high density of opioid receptors and the role of these receptors in modulating neuronal pain pathways.
REASONING:
This question tests knowledge of how intrathecal opioids produce analgesia. Opioid receptors are located throughout the CNS, including all of the above answer choices. However, the question focuses on intrathecal opioids primary site of action which is the substantia gelatinosa. Understanding the pain pathways in the CNS would help determine that receptors in the substantia gelatinosa would be the most effective in modulating the pathways and producing analgesia, making E the best answer.
BIBLIOGRAPHY:
Barash PG, Cullen BF, Stoelting RK, Cahalan MK, Stock MC. Clinical Anesthesia. 6th ed. Philadelphia, PA: Lippincott Williams & Wilkins; 2009:466-468.
Chestnut DH, Polley LS, Lawrence CT, Wong CA. Chestnut’s Obstetric Anesthesia Principles and Practice. 4th ed. Philadelphia, PA: Mosby Elsevier; 2009:263-266.
Stoelting RK, Miller RD. Basics of Anesthesia. 5th ed. Philadelphia, PA: Churchill Livingstone; 2007:113-114.
BOOK B: QUESTION 9
Answer D
QUESTION (Choose single best answer):
During laser excision of vocal cord polyps in a 5-year-old boy, dark smoke suddenly appears in the surgical field. The trachea is intubated, and anesthesia is being maintained with halothane, nitrous oxide, and oxygen. The most appropriate initial step is to
Clinical Anesthesia
(A) Change from oxygen and nitrous oxide to air.
(B) Fill the oropharnyx with water.
(C) Instill water into the endotracheal tube.
(D) Remove the endotracheal tube.
(E) Ventilate with carbon dioxide.
CORRECT ANSWER: D
SUMMARY:
Airway fire due to laser is the number one complication (and most disastrous) of laser surgery of the airway, with a cited incidence of 0.14%. The first step is to extubate the trachea. Prevention involves avoiding the use of a tracheal tube if possible (jet ventilation or a mask/apnea technique), avoiding combustible N2O, using the lowest FIO2 possible (21% if tolerated), limiting laser time by the surgeon, insufflating the cuff with methylene blue and saline, or substituting a metal-wrapped tracheal tube. Tubes made of polyvinyl chloride (PVC) are highly susceptible to fire from CO2 lasers, while Nd:YAG lasers are less prone to cause fire with PVC but can still ignite if blood or secretions coat the tube. After mask ventilation and reintubation, bronchoscopy can be used to diagnose further airway damage.
EXPLANATION:
(A) Incorrect. Changing to room air is not part of the airway-fire protocol. This would actually be a strategy to prevent airway fire. Also, changing to air does not immediately remove the combustible gases, O2 and N2O, already present in the airway.
(B) Incorrect. This maneuver is also not part of the airway-fire protocol. If the source of the fire is coming from the blow-torch phenomenon at the distal end of the tracheal tube, water into the oropharynx would not address this issue.
(C) Incorrect. Loose or charred pieces of the tracheal tube or damaged tissue could potentially be pushed into distal airways if water is instilled into the tube. After extubation and mask ventilation, the entire tube should be placed in water.
(D) Correct. Extubation and discontinuation of ventilation is the first step. This removes all three of the fire sources from the patient’s airway: the fuel (tracheal tube), combustion gases (O2 and N2O), and the ignition source (laser). Currently used volatile anesthetics are not flammable and not explosive.
(E) Incorrect. This maneuver plays no role in treating airway fire.
REASONING:
This question requires familiarity with the algorithm for airway fire. Extubating the trachea is of primary importance because the combustion gases (N2O and O2) and the flammable source (tracheal tube) are still in the surgical field where the ignition source (laser) is being used. Choice E can be eliminated easily in this case. Choice A is challenging because it does substitute the combustion agents for air, but is actually a preventive technique and not a treatment. Choice C is tempting, but false because the tube, once removed, should be entirely submerged in water. Choice B does not address the fire if the portion of the burned tube is below the level of the cords and not in direct contact with the oropharynx.
BIBLIOGRAPHY:
Miller RD, Eriksson LI, Fleisher LA, Wiener-Kronish JP, William YL. Miller’s Anesthesia. 7th ed. Philadelphia, PA: Churchill Livingstone; 2010:2412-2413.
Morgan GE, Mikhail MS, Murray MJ. Clinical Anesthesiology. 4th ed. New York, NY: McGraw-Hill; 2006:26, 28, 839-840 (Table 39-3 Airway-Fire Protocol).
BOOK B: QUESTION 10
Answer E
QUESTION (Choose single best answer):
During craniotomy in the sitting position, end-tidal carbon dioxide tension suddenly decreases. Ventilatory excursion of the chest is normal. Further evaluation is most likely to show a decrease in
Neuroanesthesia
(A) Alveolar-to-arterial oxygen tension difference.
(B) Alveolar-to-arterial carbon dioxide tension difference.
(C) Dead space ventilation.
(D) Pulmonary artery pressure.
(E) Pulmonary artery occlusion pressure (POAP).
CORRECT ANSWER: E
SUMMARY:
The incidence of air embolism is highest during sitting craniotomies (20%-40%). Because of the 10% to 25% population incidence of patent foramen ovale, there is a significant risk of paradoxical air embolus. Clinical signs of air embolism include a decrease in end-tidal carbon dioxide tension (ETco2) and a decrease in Spo2 owing to increased dead space ventilation (increased A-a gradient for O2 and CO2), as well as hypotension. A large volume of air in the right ventricle can lead to right ventricular outflow tract (RVOT) obstruction and increased pulmonary artery pressures. RVOT obstruction will lead to decreased left ventricular preload and decreased PAOP.
EXPLANATION:
(A) Incorrect. There is an increase in the A–a O2 gradient.
(B) Incorrect. There is an increase in the A–a CO2 gradient.
(C) Incorrect. Dead space ventilation increases.
(D) Incorrect. The pulmonary artery pressure is increased with air embolism.
(E) Correct. RVOT obstruction will lead to decreased left ventricular preload, resulting in a decreased PAOP.
REASONING:
This question tests knowledge of the signs of venous air embolism (VAE) in a patient undergoing craniotomy in the sitting position. VAE can occur anytime the surgical area is above the level of the heart and there are large venous sinuses or plexuses that can entrain air. Clinical signs of VAE under anesthesia depend on the amount and rate of entrainment and the preexisting cardiopulmonary derangement. Signs can range from subtle to catastrophic cardiorespiratory collapse. It is common to see a decrease in ETco2 and Spo2 in VAE. Rapid sudden rise in the end-tidal nitrogen concentration is also seen. Hypotension often can present as the first sign. Right ventricular outflow tract and pulmonary arterial obstruction leads to increased pulmonary artery pressure, right ventricular strain and failure, and cardiovascular collapse. The key is to understand that RVOT obstruction leads to decreased forward flow through the pulmonary circulation and subsequent decrease in left ventricular preload, reflected by a decreased PAOP. E is the single best answer.
BIBLIOGRAPHY:
Barash PG, Cullen BF, Stoelting RK, Cahalan M, Stock M. Clinical Anesthesia. 6th ed. Philadelphia, PA: Lippincott Williams &Wilkins; 2009:1019, 1380-1381.
Miller RD, Eriksson LI, Fleisher LA, et al. Anesthesia. 7th ed. New York, NY: Churchill Livingstone; 2010:2055-2058, 2057f.
Morgan GE, Mikhail MS, Murray MJ. Clinical Anesthesiology. 4th ed. New York, NY: McGraw-Hill; 2006:638-639.
BOOK B: QUESTION 11
Answer A
QUESTION (Choose single best answer):
Which of the following is a cardiorespiratory effect of epidural block to a T4 sensory level?
OB/Regional
(A) Decreased expiratory reserve volume.
(B) Decreased tidal volume.
(C) Increased circulating catecholamine concentrations.
(D) Increased heart rate.
(E) Unchanged vital capacity.
CORRECT ANSWER: A
SUMMARY:
Epidural anesthesia results in blockade of sympathetic fibers two to six levels above the sensory level, resulting in decreased heart rate, cardiac output, and blood pressure. In healthy individuals, respiratory effects of neuraxial blockade are relatively minimal. Tidal volume, minute ventilation (MV), dead space, arterial blood gas tensions, and shunt fraction are minimally affected. Sensory levels affecting abdominal and intercostal musculature can have an effect on respiratory function by decreasing active exhalation and therefore decreasing expiratory reserve volume (ERV). Of note is the fact that apnea associated with neuraxial block is due to hypoperfusion of the brain stem respiratory centers rather than diaphragmatic or phrenic nerve paralysis.
EXPLANATION:
(A) Correct. Epidural blockade with a T4 sensory level is associated with abdominal and intercostal muscle relaxation, which can impair active exhalation and therefore decrease ERV.
(B) Incorrect. Tidal volume remains unchanged.
(C) Incorrect. Epidural anesthesia is associated with blockade of sensory afferent fibers associated with the stress response to surgery, and therefore levels of catecholamines are reduced.
(D) Incorrect. Because of the differential blockade of nerve fibers associated with neuraxial anesthesia, the sympathetic fibers two to six levels above the sensory level will be affected. A T4 sensory level will be associated with blockade of the cardioaccelerator fibers at T1-4 and will result in decreased heart rate.
(E) Incorrect. Vital capacity includes ERV. Because the ERV is decreased, vital capacity must decrease.
REASONING:
The key concepts for answering this question involve understanding differential blockade, the components of pulmonary volumes and capacities, and the physiologic effects of neuraxial blockade. Because ERV is a component of vital capacity, choice E can be eliminated. Knowledge of the effects of sympathetic blockade eliminates choices C and D, and understanding that unless the brain stem is hypoperfused with an unusually high block, the MV should remain unchanged eliminates choice B.
BIBLIOGRAPHY:
Barash PG, Cullen BF, Stoelting RK, Cahalan M, Stock M. Clinical Anesthesia. 6th ed. Philadelphia, PA; Lippincott Williams & Wilkins; 2010:947.
Miller RD, Eriksson LI, Fleisher LA, Wiener-Kronish JP, William YL. Miller’s Anesthesia. 7th ed. Philadelphia, PA: Churchill Livingstone; 2010:1616-1618.
Morgan GE, Mikhail MS, Murray MJ. Clinical Anesthesiology. 4th ed. New York, NY: McGraw-Hill; 2006;297, 545 (Figure 22-4).
BOOK B: QUESTION 12
Answer E
QUESTION (Choose single best answer)
Physiology
This figure describes the uptake of nitrous oxide 75% by individual tissue groups (vessel-rich group [VRG], muscle group [MG], fat group [FG]) and their sum (total uptake [TU]). Which set of labels accurately describes the curves?
CORRECT ANSWER: E
SUMMARY:
The uptake of inhaled anesthetics by tissues is influenced by blood gas solubility, blood flow, and the partial pressure difference (arterial and venous blood). The vessel-rich group (VRG) has a rapid uptake and limited capacity, so it gets saturated quickly (curve 2). The muscle group has less blood supply but greater capacity, so it can have continued uptake for hours (curve 3). The fat group has poor blood supply but enormous capacity for gases with increased lipid solubility. Because fat can have prolonged uptake (days), total uptake by the body will continue, albeit at a lower rate.
EXPLANATION:
(A) Incorrect. For all inhaled anesthetics, greatest uptake in the initial period occurs in the VRG group. The VRG organs, such as the brain, heart, kidney, liver, and endocrine system, have limited capacity and are saturated rapidly, and uptake decreases.
(B) Incorrect. The muscle group has smaller blood supply and huge capacity and continues to take up anesthetic for hours.
(C) Incorrect. The fat group has poor blood supply and the greatest capacity. It will have continued uptake for days (except for N2O).
(D) Incorrect. See above.
(E) Correct. See above.
REASONING:
This is a challenging question that tests knowledge of uptake and distribution of inhaled anesthetics. Curve 2 fits the description of the VRG, and only answer E has curve 2 in the correct order. By this reasoning, the reader can disregard all other answers. E is the best answer.
BIBLIOGRAPHY:
Barash PG, Cullen BF, Stoelting RK, Cahalan M, Stock M. Clinical Anesthesia. 6th ed. Philadelphia, PA: Lippincott Williams & Wilkins; 2009:416-417.
Morgan GE, Mikhail MS, Murray MJ. Clinical Anesthesiology. 4th ed. New York, NY: McGraw-Hill; 2006;157-159.
BOOK B: QUESTION 13
Answer B
QUESTION (Choose single best answer):
A 67-year-old man undergoes spinal anesthesia with hyperbaric tetracaine 10 mg for transurethral resection of the prostate (TURP). At the end of the 50-minute procedure, the level of anesthesia is T6, and blood pressure is 120/70 mm Hg. Within 2 minutes of transfer to a stretcher, the patient has nausea, and his blood pressure decreases to 76/42 mm Hg. Which of the following is the most likely cause of the acute hypotension?
OB/Regional
(A) Acute congestive heart failure.
(B) Decreased venous return.
(C) Dilutional hyponatremia.
(D) Progression of sympathetic block.
(E) Unrecognized bladder perforation.
CORRECT ANSWER: B
SUMMARY:
TURP can be associated with excessive fluid absorption and subsequent fluid overload. The resulting clinical signs and symptoms are due to hyponatremia and increased intravascular volume and are collectively termed TURP syndrome. This syndrome is characterized clinically by restlessness, confusion, nausea, vomiting, lethargy, hypertension, bradycardia, tachypnea, and seizures. This constellation of symptoms is difficult to assess in a patient under general anesthesia. For this reason, regional techniques, especially spinal anesthesia, are popular for this procedure. While spinal block is considered preferable to general anesthesia for TURP, the patient is still vulnerable to its cardiovascular effects. These include decreased arterial vascular sympathetic tone, decreased venous return, and decreased cardiac output, and they can be exacerbated by changes in position during the procedure. When complications occur, the astute clinician must be able to differentiate between complications attributable to the procedure and those attributable to the anesthetic technique.
EXPLANATION:
(A) Incorrect. Acute congestive heart failure (CHF), presumably due to fluid overload, is unlikely in this case because the patient did not exhibit any of the symptoms of TURP syndrome prior to his hemodynamic instability.
(B) Correct. Spinal anesthesia results in decreased venous return. The position commonly used for TURP is lithotomy with Trendelenburg position, which facilitates venous return. When the patient was transferred out of this position and his legs were placed in a dependent position, venous return was decreased. Combined with the sympathectomy from the spinal block, this change in position resulted in severe hypotension secondary to the inability to compensate by increasing vascular tone.
(C) Incorrect. Dilutional hyponatremia occurs following TURP owing to excessive fluid absorption. It causes many of the clinical symptoms associated with TURP syndrome, including lethargy, confusion, and seizures. TURP syndrome is also associated with hypertension, which is not seen in this situation, so it is unlikely.
(D) Incorrect. Progression of sympathetic block is unlikely in this situation because the patient was hemodynamically stable until movement to the stretcher. While tetracaine is a local anesthetic with a long duration of action, it is likely that the block is stable after 50 minutes.
(E) Incorrect. Bladder perforation is a complication of TURP. It manifests as abdominal pain, commonly referred to the shoulder, even in patients with adequate neuraxial blockade. This pain tends to have a temporal relationship to the perforation and typically occurs during the procedure.
REASONING:
The key to this question is the timing of this patient’s hypotension. It occurs after the procedure and is associated with moving to the stretcher. It is important to know the signs and symptoms of TURP syndrome to recognize that this patient does not appear to have this condition. Therefore, choices A and C can be eliminated. The timing of the hypotension eliminates choices C and D. Lack of abdominal pain makes choice E unlikely. The best answer is B.
BIBLIOGRAPHY:
Barash PG, Cullen BF, Stoelting RK, Cahalan M, Stock M. Clinical Anesthesia. 6th ed. Philadelphia, PA: Lippincott Williams & Wilkins; 2010:945-946.
Miller RD, Eriksson LI, Fleisher LA, Wiener-Kronish JP, William YL. Miller’s Anesthesia. 7th ed. Philadelphia, PA: Churchill Livingstone; 2010:1616-1618.
Morgan GE, Mikhail MS, Murray MJ. Clinical Anesthesiology. 4th ed. New York, NY: McGraw-Hill; 2006:759-761, 760 (Figure 33-2 Manifestations of the TURP syndrome).
BOOK B: QUESTION 14
Answer A
QUESTION (Choose single best answer):
A 26-year-old woman has persistent uterine bleeding following a normal spontaneous delivery without anesthesia. The uterus is firm on manual examination. Which of the following anesthetics is most appropriate for manual extraction of the placenta?
OB/Regional
(A) Sevolfurane.
(B) Pudendal block with lidocaine.
(C) Subarachnoid tetracaine.
(D) Thiopental.
(E) Vecuronium.
CORRECT ANSWER: A
SUMMARY:
Retained products of conception that require manual extraction are a common cause of postpartum hemorrhage and occur in up to 3.3% of deliveries. An important distinction is whether the patient requires analgesia and/or uterine relaxation. If the patient has a functioning epidural or spinal block, this may be adequate for manual extraction if the uterus is not contracted. If the uterus has contracted, it will be virtually impossible for the obstetrician to extract the placenta without relaxation. Classically, this has been done with volatile anesthetic agents (equipotent doses of halothane, sevoflurane, and desflurane cause equivalent uterine relaxation), frequently requiring induction of general anesthesia and endotracheal intubation for airway protection. More recently, nitroglycerin (intravenous or sublingual) or terbutaline has been used with great success. Hypotension with nitroglycerin has not been a clinically significant problem, and the risk of hypotension is outweighed by the advantages of not requiring an anesthetic machine, protection of airway reflexes, avoidance of general anesthesia, and the short duration of action.
EXPLANATION:
(A) Correct. The question mentions that the uterus is firm and that manual extraction of the placenta is required. This cannot be accomplished without uterine relaxation, and halothane is the only agent among the choices that will provide uterine relaxation.
(B) Incorrect. Pudendal block will anesthetize the S2-4 nerves associated with the pain of the second stage of labor but will not relax the uterus.
(C) Incorrect. Subarachnoid tetracaine will provide spinal anesthesia, which does not relax the uterus. Of note, tetracaine will have a prolonged onset and long duration of action in this patient who is bleeding and has the potential for hemodynamic instability. Thus it would not be a preferable agent for spinal anesthesia.
(D) Incorrect. Thiopental will induce general anesthesia but will not provide uterine relaxation.
(E) Incorrect. Vecuronium is an NDMR. It will not relax the uterus, and its administration to this patient would result in a paralyzed, awake patient with an unprotected airway.
REASONING:
This question is straightforward, provided that one knows that the patient and obstetrician require uterine relaxation for manual extraction of the placenta. The only agent among the list of choices that provides uterine relaxation is sevoflurane. Current practice is to use nitroglycerin for this procedure, but at the time the test question was written, it may not have been in widespread use.
BIBLIOGRAPHY:
Bucklin B, Gambling DR, Wlody DJ. A Practical Approach to Obstetric Anesthesia. Philadelphia, PA: Lippincott Williams & Wilkins; 2009:253-254.
Chestnut DH, Polley LS, Lawrence CT, Wong CA. Chestnut’s Obstetric Anesthesia Principles and Practice. 4th ed. St. Louis, MO: Mosby Elsevier; 2009:368, 823.
BOOK B: QUESTION 15 (OPTIONAL)
Answer B
QUESTION (Choose single best answer):
Compared with intermittent positive-pressure ventilation (IPPV), intermittent mandatory ventilation (IMV)
Physiology
(A) Better maintains cardiac output.
(B) Provides less than full mechanical ventilatory support.
(C) Requires a greater level of sedation.
(D) Requires a higher FIO2.
(E) Requires a lower inspiratory flow rate.
CORRECT ANSWER: B
SUMMARY:
Controlled mechanical ventilation (CMV), that is, using positive pressure to ventilate the lungs, is commonly used in the operating rooms and on intensive care units (ICUs). Intermittent positive-pressure ventilation (IPPV), continuous positive-pressure ventilation (CPPV) (IPPV + PEEP), and intermittent mandatory ventilation (IMV) are among the common modes of mechanical ventilation. IPPV is best suited for paralyzed patients without spontaneous breathing. Respiratory rate (RR) is set and minute ventilation (MV) is depending on the tidal volume, which is constant if ventilation is volume controlled. Patient is unable to breathe between the mechanical breaths. In contrast, IMV allows the patient to breathe between the breaths if needed. The RR in IMV guarantees a minimum of backup ventilation. Hence, the MV can be variable depending on the patient’s own RR.
EXPLANATION:
(A) Uncertain. The effects of positive-pressure ventilation on the cardiovascular system are too complex and depend on the specific situation of the patient such as hypovolemia, compromised myocardial function, pulmonary disease, etc. In general, an increase in the intrathoracic pressure caused by positive-pressure ventilation may reduce the venous return to the right atrium and cause a decrease in cardiac output. This effect is more prominent when the patient is hypovolemic. To compare the effects of the two ventilation modes, the exact settings must be known. IMV in a heavily sedated patient does not differ from IPPV when the settings are comparable. In patients with compromised cardiac pump function, positive-pressure ventilation may improve the cardiac output.
(B) Correct. This answer is correct if the patient has some amount of spontaneous ventilation, because in that case the patient can breathe between the mandatory mechanical breaths. In a paralyzed or heavily sedated patient, IMV can be similar to IPPV and provide full ventilatory support.
(C) Incorrect. Because IPPV does not allow the patient to breathe spontaneously between the mechanical breaths, it is suitable for a paralyzed or heavily sedated patient. In contrast, IMV does not require heavy sedation. IMV is advantageous when weaning the patient from the ventilator is the goal.
(D) Incorrect. Any level of FIO2 can be used with either ventilation modes.
(E) Incorrect. The flow rate can be set according to the ventilatory parameters. Lower flow rate is not a specification of IMV.
REASONING:
A basic knowledge of mechanical ventilation is key to answering this question. The simplest mode of mechanical ventilation is IPPV that is broadly used in the operating room. With this mode the ventilator delivers the preset breaths regardless of what the patient is doing. The patient would encounter a closed valve if he/she attempted a spontaneous breath. As an improvement and as a step forward toward weaning a patient from the ventilator, the IMV was created. For this type of ventilation, patients can attempt spontaneous breathing between the mechanical breaths, even though some breaths may collide with the mandatory mechanical breaths. By varying the rate and tidal volume of the mandatory breaths in IMV, the ventilatory support can be tailored to the patient’s needs.
BIBLIOGRAPHY:
Hall JB, Schmidt GA, Wood LDH. Principles of Critical Care. 3rd ed. 2005, Chapter 44, pp 625-637.
Morgan GE, Mikhail MS, Murray MJ. Clinical Anesthesiology. 4th ed. New York, NY: McGraw-Hill; 2006:77-79.
Shekerdemian L, Bohn D. Cardiovascular effects of mechanical ventilation. Arch Dis Child. 1999;80:475-480.
BOOK B: QUESTION 16
Answer D
QUESTION (Choose single best answer):
Which of the following findings would be considered normal in the electroencephalogram (EEG) of an adult?
Neuroanesthesia
(A) Decreased frequency during induction with halogenated anesthetics.
(B) Decreased frequency in frontal areas with administration of nitrous oxide 50%.
(C) Dominance of beta rhythm at 20 to 30 Hz during the awake relaxed state.
(D) Electrical silence with administration of isoflurane 2.5 minimum alveolar concentration (MAC).
(E) The presence of burst suppression during natural sleep.
CORRECT ANSWER: D
SUMMARY:
EEG is a commonly used monitor during anesthetics in which cerebral perfusion is of concern. Isoflurane is unique in that it produces an isoelectric EEG pattern at clinically used doses of 1 to 2 MAC, which would persist at levels of 2.5 MAC. However, desflurane and sevoflurane will not produce an isoelectric EEG pattern at clinically used doses but can produce burst suppression. Nitrous oxide is unique in producing a high-frequency high-amplitude activation pattern on the EEG.
EXPLANATION:
(A) Incorrect. The biphasic EEG pattern seen with many anesthetics begins with EEG activation during induction (high-frequency, low-voltage waves) and progresses to depression (low-frequency, high-voltage) as the dose escalates.
(B) Incorrect. Nitrous oxide is unique in that it produces a high-amplitude activation of the EEG (high-frequency, high-amplitude) and at levels of 50% produces this pattern predominantly in the anterior EEG leads.
(C) Incorrect. Beta rhythms (> 12 Hz) are high-frequency low-amplitude waves and are the most common pattern during the awake arousal state, while alpha rhythms (8-12 Hz) are the dominant pattern of the awake relaxed state.
(D) Correct. Isoflurane is unique among the volatile anesthetics in that it produces an isoelectric EEG pattern (ie, it is abolished) at clinically used doses of 1 to 2 MAC, with adequate preservation of hemodynamic parameters. The isoelectric EEG would be expected to persist at isoflurane levels as high as 2.5 MAC.
(E) Incorrect. Burst suppression does not occur during sleep but can occur with many intravenous and inhalational anesthetics.
REASONING:
This question requires familiarity with both basic EEG wave types and those produced by inhalational anesthetics. Because burst suppression does not occur during sleep and beta patterns are the primary wave during arousal, choices E and C can be eliminated, respectively. Knowing that nitrous oxide increases EEG frequencies eliminates choice B, while remembering that the biphasic EEG pattern results first in activation during induction leaves choice D as the only possible correct answer.
BIBLIOGRAPHY:
Barash PG, Cullen BF, Stoelting RK, Cahalan M, Stock M. Clinical Anesthesia. 6th ed. Philadelphia, PA: Lippincott Williams & Wilkins; 2010:424-426, 1009-1010.
Morgan GE, Mikhail MS, Murray MJ. Clinical Anesthesiology. 4th ed. New York, NY: McGraw-Hill; 2006:chap 25, 624-625 (Table 25-2 Electroencephalographic Changes During Anesthesia).
BOOK B: QUESTION 17
Answer B
QUESTION (Choose single best answer):
Proper zeroing of an arterial pressure transducer attached to a supine anesthetized patient is best accomplished by
Equipment/Physics
(A) Continuous flow of fluid through the intravascular catheter.
(B) Opening the system to air at heart level.
(C) Placement of the transducer diaphragm at heart level.
(D) Proper damping of the transducer system.
(E) Zeroing the transducer during the expiration phase of mechanical ventilation.
CORRECT ANSWER: B
SUMMARY:
Accuracy of invasive arterial blood pressure monitoring depends on correct zeroing and leveling procedures. Zeroing is accomplished by exposing the transducer to atmospheric pressure by opening the stopcock to air and pressing the zero-pressure button on the monitor. Leveling assigns the zero reference point to a specific position on the patient’s body, which is the level of the heart found at the midchest midaxillary line in the supine position.
EXPLANATION:
(A) Incorrect. Zero reference point is defined as atmospheric pressure, not a continuous flow of fluid through the catheter.
(B) Correct. Opening the system to air at heart level will accomplish both zeroing and level of the transducer to allow for accurate measurements.
(C) Incorrect. Placement of the transducer diaphragm at heart level levels the transducer but fails to set a zero reference point.
(D) Incorrect. The damping coefficient is a measure of how long it takes an oscillating system to come to rest, which is important for accurate measurements but is not involved in the zeroing procedure.
(E) Incorrect. Zeroing is used to measure atmospheric pressure and thus ventilation has no effect on zeroing.
REASONING:
This question tests knowledge of proper zeroing and leveling of a catheter-fluid arterial pressure transducer system. Answers A and D can be eliminated because they are not involved in the zeroing process. Ventilation has no effect on zeroing; thus answer E can be eliminated. Answer C is tempting, but it describes only leveling and not zeroing the system. Answer B describes proper zeroing and is the correct answer.
BIBLIOGRAPHY:
Miller RD, Eriksson LI, Fleisher LA, Weiner-Kronish JP, Young WL. Miller’s Anesthesia. 7th ed. Philadelphia, PA: Churchill Livingstone; 2010:1277-1281.
Morgan GE, Mikhail MS, Murray MJ. Clinical Anesthesiology. 4th ed. New York, NY: McGraw-Hill; 2006:126-130.
BOOK B: QUESTION 18
Answer B
QUESTION (Choose single best answer):
A 1-month-old infant becomes hypoxemic faster during apnea than an adult. Which of the following is the primary cause of this difference?
Pediatrics
(A) Functional residual capacity in an infant is half that of an adult.
(B) Metabolic rate in an infant is twice that of an adult.
(C) Resting PaO2 in an infant is lower than that in an adult.
(D) The number of alveoli in an infant is 12% the number in an adult.
(E) The hemoglobin dissociation curve in an infant is shifted to the right.
CORRECT ANSWER: B
SUMMARY:
Infant hemoglobin desaturates faster than that of an adult during periods of apnea primarily due to an elevated metabolic rate and rate of oxygen consumption (7-9 mL/kg/min infant, 3 mL/kg/min adult). Although tidal volumes are similar between infants and adults (6-7 mL/kg), RR and MV are both higher in infants. Infant functional residual capacity (FRC) is slightly less than that of an adult, but a higher MV/FRC ratio leaves less oxygen available in the FRC during apnea. Also, infants have a higher work of breathing due to their compliant chest wall and less fatigue-resistant type I muscle fibers in the diaphragm.
EXPLANATION:
(A) Incorrect. Infant FRC (27-30 mL/kg) is slightly less than that of an adult, but not half. This can contribute to faster desaturation during apnea, but it is not the primary reason.
(B) Correct. Infants have a higher rate of oxygen consumption (two to three times higher) compared to adults, which is the primary reason for faster hypoxemia during apnea. The higher MV/FRC ratio leaves less available oxygen in the FRC component during apnea.
(C) Incorrect. Normal resting PaO2 is 85 to 90 mm Hg between the ages of 1 and 10 months, with adult values slightly higher at 100 mm Hg. This small difference does not contribute to rapid desaturation.
(D) Incorrect. Infant alveoli are fewer in number and smaller in size than those of an adult, approaching adult values by age 8. While this can contribute to a reduced surface area for oxygen exchange, it is not the primary reason for hemoglobin desaturation during infant apnea.
(E) Incorrect. Hemoglobin F (HbF) constitutes 70% to 80% of total hemoglobin at birth and decreases markedly by the age of 3 to 6 months. HbF causes a left shift, not a right shift, in the oxyhemoglobin dissociation curve and does not contribute to the faster desaturation during infant apnea.
REASONING:
This question is challenging because choices B and C are both true statements regarding infant respiratory physiology, but only choice B is the primary reason for desaturation during apnea. Choice A significantly overestimates the FRC difference and choice D overestimates the alveolar anatomical difference. Choice E is clearly wrong because HbF causes a left shift in the curve.
BIBLIOGRAPHY:
Barash PG, Cullen BF, Stoelting RK, Cahalan M, Stock M. Clinical Anesthesia. 6th ed. Philadelphia, PA: Lippincott Williams & Wilkins; 2010:1174.
Morgan GE, Mikhail MS, Murray MJ. Clinical Anesthesiology. 4th ed. New York, NY: McGraw-Hill; 2006:chap 44, 923-924 (Table 44-1 Characteristics of Neonates and Infants That Differentiate Them From Adult Patients).
Stoelting RK, Miller RD. Basics of Anesthesia. 5th ed. Philadelphia, PA: Churchill Livingstone; 2007:507-509.
BOOK B: QUESTION 19
Answer B
QUESTION (Choose single best answer):
During extracorporeal shock wave lithotripsy, the shock wave should be synchronized with
Clinical Anesthesia
(A) The P wave of the ECG (electrocardiogram).
(B) The R wave of the ECG.
(C) The T wave of the ECG.
(D) Peak inspiration.
(E) End expiration.
CORRECT ANSWER: B
SUMMARY:
Extracorporeal shock wave lithotripsy (ESWL) is used to treat kidney stones in the upper two-thirds of ureters or kidneys. Repetitive high-energy shock waves are generated and focused on the stone, which cause it to fragment by shear and tear forces. Dissipation of shock wave energy can cause tissue injury, including mechanical stress on the cardiac conduction system leading to arrhythmias. Synchronization of shock waves to the R wave of the ECG decreases the incidence of arrhythmias.
EXPLANATION:
(A) Incorrect. The shock waves are timed to be 20 milliseconds after the R wave of the ECG to correspond with the ventricular refractory period. Synchronizing with the P or T wave will induce arrhythmias.
(B) Correct. The shock waves are timed to be 20 milliseconds after the R wave of the ECG to correspond with the ventricular refractory period.
(C) Incorrect. See answer A.
(D) Incorrect. Lung tissue is susceptible to injury by the shock waves because its airtissue interface can cause dissipation of energy. However, the lungs are typically not in the path of the shock wave in ESWL, and shocks do not need to be synchronized with the ventilatory cycle. This procedure is often performed in patients under regional anesthesia where they are maintaining spontaneous ventilation.
(E) Incorrect. See answer D.
REASONING:
This question tests knowledge of ESWL and its complication of causing cardiac arrhythmias. Answers D and E can be eliminated as ESWL can be performed under regional anesthesia with the patient spontaneously breathing. To decrease the incidence of arrhythmias, the shock wave during ESWL should coincide with the refractory period of the ventricle, making answer B the best choice.
BIBLIOGRAPHY:
Miller RD, Eriksson LI, Fleisher LA, Weiner-Kronish JP, Young WL. Miller’s Anesthesia. 7th ed. Philadelphia, PA: Churchill Livingstone; 2010:2124-2126.
Morgan GE, Mikhail MS, Murray MJ. Clinical Anesthesiology. 4th ed. New York, NY: McGraw-Hill; 2006:762-764.
BOOK B: QUESTION 20
Answer E
QUESTION (Choose single best answer)
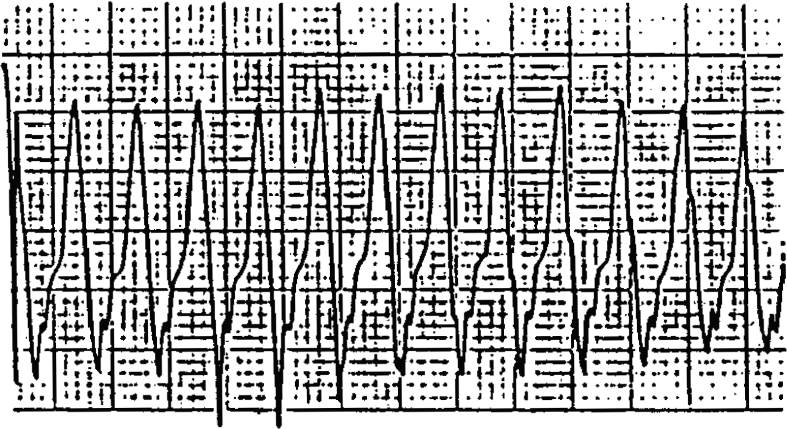
The cardiac rhythm shown here appeared suddenly in an anesthetized patient. The most appropriate management is
Cardiovascular
(A) Administration of adenosine.
(B) Administration of digoxin.
(C) Administration of epinephrine.
(D) Overdrive pacing.
(E) Synchronous cardioversion.
CORRECT ANSWER: E
SUMMARY:
Stable monomorphic VT is treated with synchronized cardioversion (E) or antiarrhythmic drugs such as amiodarone, sotalol, procainamide, or lidocaine. PEA or VT/VF should be treated with immediate defibrillation and CPR.
EXPLANATION:
(A) Incorrect. Adenosine is incorrect. Adenosine is used in the treatment of SVT and narrow and wide complex tachycardia of supraventricular origin. Adenosine also helps differentiate between wide complex tachycardia of supraventricular and nonsupraventricular origin.
(B) Incorrect. Digoxin is incorrect. It is not used in the acute management of ventricular tachycardia.
(C) Incorrect. Epinephrine is incorrect. Epinephrine is first-line therapy in the current ACLS (advanced cardiovascular life support) guidelines for PEA and VT/VF.
(D) Incorrect. Overdrive pacing is incorrect. Overdrive pacing may be useful in polymorphic ventricular tachycardia with a prolonged QT.
(E) Correct. The correct treatment is synchronized cardioversion (initial recommended dose monophasic 100-200 J; biphasic 50-100 J).
REASONING:
Synchronous cardioversion is correct. Given the information in the question stem, assume monomorphic VT with a pulse and unknown cardiac function. The treatment is synchronized cardioversion (initial recommended dose monophasic 100-200 J; biphasic 50-100 J). In stable patients with wide-QRS tachycardia and preserved LV function, you may consider an antiarrhythmic infusion of procainamide, amiodarone, or sotalol.
BIBLIOGRAPHY:
American Heart Association. 2010. Guidelines for CPR and Emergency Cardiovascular Care.
Miller RD, Eriksson LI, Fleisher LA, Wiener-Kronish JP, William YL. Miller’s Anesthesia. 7th ed. Philadelphia, PA: Churchill Livingstone; 2009:Chap 97.
BOOK B: QUESTION 21
Answer B
QUESTION (Choose single best answer):
Which of the following statements concerning hyperkalemia after succinylcholine administration to a patient with a spinal cord injury is true?
Clinical Anesthesia
(A) It is unlikely to occur if the lesion is located below T6.
(B) It is unlikely to occur within 24 hours of the injury.
(C) It is unlikely to occur more than 60 days after the initial injury.
(D) It is prevented by pretreatment with small doses of a nondepolarizing agent.
(E) It is decreased in magnitude by pretreatment with calcium chloride.
CORRECT ANSWER: B
SUMMARY:
Succinylcholine normally raises serum potassium levels by 0.5 mEq/L. In skeletal muscle injuries or atrophy caused by spinal cord injury, there is upregulation of acetylcholine receptors outside the NMJ. Widespread depolarization of these receptors can result in life-threatening potassium levels (up to 14 mEq/L), causing irreversible cardiac arrest and dysrhythmias, a process that peaks between 7 days and 5 months after injury. Administration of succinylcholine is unlikely to cause hyperkalemia during the first 24 hours after an injury, but it should be avoided after that time. Although the risk of hyperkalemia probably decreases 6 months after the injury, the use of NDMRs is preferred.
EXPLANATION:
(A) Incorrect. Injuries below T1 and above L4 result in paraplegia, which places patients at risk for succinylcholine-induced hyperkalemia.
(B) Correct. Succinylcholine-induced hyperkalemia is unlikely to occur within 24 hours of a spinal cord injury.
(C) Incorrect. While most sources report that the risk of hyperkalemia after a spinal cord injury probably decreases after 6 months, the true duration is unknown. An NDMR must be used 60 days after a spinal cord injury when there is still significant risk of hyperkalemia.
(D) Incorrect. Life-threatening hyperkalemia after succinylcholine administration is not reliably prevented by pretreatment with an NDMR.
(E) Incorrect. Hyperkalemia is not decreased in magnitude by pretreatment with calcium chloride. The cardiac arrest that can occur with succinylcholine-induced hyperkalemia after a spinal cord injury may be refractory to normal cardiopulmonary resuscitation including treatment with calcium chloride.
REASONING:
Choice B is clearly correct. The risk of a hyperkalemic response peaks at 7 to 10 days after an injury, yet it is considered safe to administer succinylcholine to a normokalemic patient within 24 hours after a spinal cord injury. Choices A, D, and E are clearly incorrect. Choice C is likely, but because succinylcholine administration is not recommended 24 hours after a spinal cord injury. Choice A is the best answer.
BIBLIOGRAPHY:
Barash, PG, Cullen BF, Stoetling RK, Cahalan M, Stock M. Clinical Anesthesia. 6th ed. Philadelphia, PA: Lippincott-Raven Publishers; 2009;1377.
Morgan GE, Mikhail MS, Murray MJ. Clinical Anesthesiology. 4th ed. New York, NY: McGraw-Hill; 2006:210,1654-1655.
BOOK B: QUESTION 22
Answer E
QUESTION (Choose single best answer):
The severity of chronic bronchitis is best assessed by measuring
Physiology
(A) Tidal volume.
(B) Carbon dioxide diffusing capacity.
(C) Sputum production over 24 hours.
(D) Forced vital capacity.
(E) Arterial blood gases.
CORRECT ANSWER: E
SUMMARY:
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree






