Jodie Dionne-Odom
Tick-Borne Illnesses
Ticks are excellent vectors for disease transmission. More than 800 species of these obligate blood-sucking creatures inhabit the planet. They are second only to mosquitoes as vectors of human disease, both infectious and toxic. Ticks can carry and transmit a remarkable array of pathogens, such as bacteria, spirochetes, rickettsiae, protozoa, viruses, nematodes, and toxins. A single tick bite can transmit multiple pathogens, a phenomenon that has led to atypical presentations of some classic tick-borne diseases.
Many, if not most, tick-borne illnesses have a specific geographic distribution. In the United States, ticks are the most common vectors of vector-borne diseases. The incidence of tick-borne and other vector-borne illnesses is increasing worldwide, probably on the basis of global warming, international travel and trade, deforestation, and increasing population density, especially in urban areas. The encroachment of human populations into previously uninhabited wilderness where ticks and their animal hosts live has led to the increased incidence of these illnesses, challenging infectious disease and public health experts worldwide.
Lyme Disease
Definition and Epidemiology
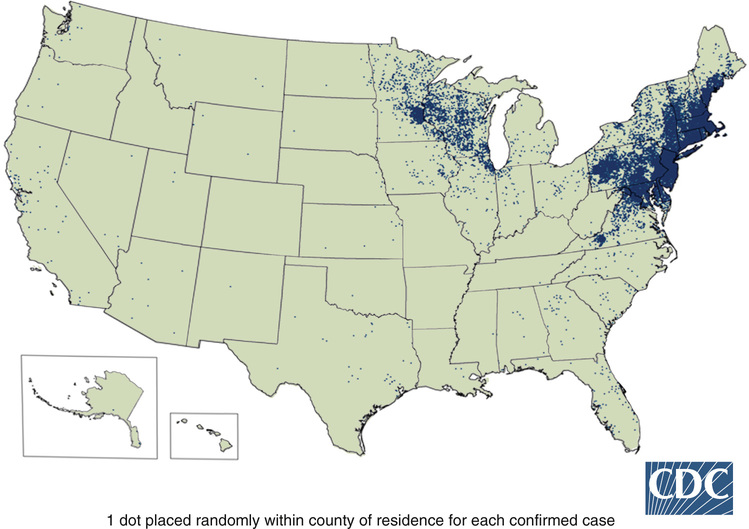
Lyme disease is caused by the bacterium Borrelia burgdorferi and is transmitted to humans by the bite of a tick. It occurs in North America, Europe, and Asia and is now the most common vector-borne disease in the United States and Europe.1 Although about 30,000 cases each year are reported to the Centers for Disease Control and Prevention (CDC; a significant increase over the past decade), an estimated 300,000 cases occur annually.2 Illness usually occurs after a tick bite during the summer months and has a characteristic expanding skin lesion known as erythema migrans that appears at the site of the bite. If the rash goes unnoticed and treatment is not given, the spirochete may disseminate in days to weeks to other sites of the body, including the nervous system and the heart. All stages are usually curable with appropriate antibiotic therapy, but the ideal phase for diagnosis and treatment is in early infection.
Pathophysiology
Lyme disease was initially recognized in 1976 as a separate entity when a cluster of children in Lyme, Connecticut, were thought to have juvenile rheumatoid arthritis and were later diagnosed with Lyme disease. Manifestations of illness had been previously reported in Europe as erythema chronicum migrans, Bannwarth syndrome, or acrodermatitis chronica atrophicans. In 1982, these syndromes were linked to the recovery of a previously unrecognized spirochete from a tick vector.1
The vector of transmission for Lyme disease is the Ixodes tick species, most commonly Ixodes scapularis in the United States. Ixodes pacificus, a less common vector, is found in the western United States, where the frequency of disease is low. The tick requires a blood meal at each stage of its life cycle (larval, nymphal, and adult stages). Horizontal transmission of B. burgdorferi occurs in the larval and nymphal stages and from certain rodents, particularly white-footed mice and chipmunks, found in the northeastern United States (from Maine to Virginia) and in the North Central states, including Wisconsin and Minnesota (Fig. 234-1). White-tailed deer are the preferred adult host but are not involved in the life cycle of the spirochete. Transmission of the spirochete to humans occurs only after an extended period of attachment (36 to 72 hours), a finding that has particular clinical importance in the diagnosis of illness associated with exposure.
Clinical Presentation
The clinical characteristics of Lyme disease can be divided into three stages: early localized infection, early disseminated infection, and late persistent infection (Box 234-1). Stage 1 (early localized infection) is characterized by a pink-red spherical rash at the site of the tick bite called erythema migrans (Fig. 234-2). It occurs in 70% to 80% of patients and usually appears within 3 to 30 days of the tick bite. It often has a homogeneous appearance with evolution to a target-like lesion with central clearing. Patients often describe this lesion as burning, itchy, or painful, although it may be minimally symptomatic and go unrecognized owing to location. Erythema at the site of a tick bite can be located anywhere on the body but is most often found on the thigh, groin, axilla, or nape of the neck, given the propensity for ticks to attach to exposed skin (often the leg) and migrate to warm, moist areas of the body.

Stage 2 (early disseminated infection) occurs within several days to weeks of infection and may be associated with multiple annular secondary skin lesions. This stage is often accompanied by constitutional symptoms, including malaise, fatigue, headaches, fevers, chills, generalized achiness, and regional lymphadenopathy. If untreated, 15% of patients may develop neurologic abnormalities during a period of weeks to months, including unilateral cranial nerve VII palsy (Bell palsy), meningitis, encephalitis, motor and sensory radiculoneuritis, mononeuritis multiplex, cerebellar ataxia, and myelitis. Five percent of untreated patients may develop cardiac involvement, most commonly atrioventricular block, which often manifests as bradycardia and sudden death from Lyme carditis; this is very rare but has been reported.3
Stage 3 (late persistent infection) occurs months after disease onset and manifests as intermittent attacks of large joint pain and swelling in the context of strong cellular and humoral immune responses to B. burgdorferi. This may persist for years, but the natural history is complete resolution of symptoms and infection, even without specific therapy.
Diagnostics
Diagnosis of Lyme disease can be complicated, but testing is commonly performed; a study showed that large commercial laboratories in the United States performed 3.4 million Lyme disease tests in 2008.4 Diagnosis of disease is predicated on three factors: presenting clinical characteristics, an epidemiologic link (possible tick exposure in an endemic area), and positive laboratory findings (an antibody response to B. burgdorferi). One exception to these rules is that early disease often occurs before the development of a detectable humoral immune response and thus requires a clinical diagnosis. For serologic testing, the CDC recommends a two-test approach of screening antibody testing followed by a more specific confirmatory test. Serum samples should be screened by enzyme-linked immunosorbent assay (ELISA), followed by confirmatory Western blot (WB) testing if results are positive or equivocal. For results to be called positive, an IgM WB must have two of the following three bands present: 23, 39, and 41 kDa. Careful interpretation of the results is essential and requires the clinician to take into account the history and clinical scenario, because the 23 and 41 kDa bands can be falsely positive. An immunoglobulin G (IgG) blot is considered positive if five of the following 10 bands are present: 18, 23, 28, 30, 39, 41, 45, 58, 66, and 93 kDa.4
Serodiagnosis is insensitive during the first few weeks of infection and only 30% of patients with erythema migrans will have detectable antibodies.5 Approximately 70% of patients will have seroreactivity 2 to 4 weeks later. Patients without signs of acute illness and a persistently positive IgM and negative IgG result months after a tick bite can be clinically assumed to have a false-positive IgM result or a persistent IgM response despite therapy. After antibiotic therapy, antibody titers decline slowly, although IgG and IgM responses may persist for years, complicating the diagnosis of subsequent reinfections with B. burgdorferi.1
One new test is the C6 ELISA, which appears to be more sensitive in early disease and performed well in patients who had been exposed to ticks in Europe, but it is somewhat less specific than the ELISA/WB testing and studies are ongoing.6 Alternative diagnostics, such as polymerase chain reaction (PCR) assay of a skin biopsy sample or borrelial culture of skin or blood, are expensive to perform and are not currently recommended outside of a research setting.7
Differential Diagnosis
The differential diagnosis for Lyme disease varies according to the stage of disease. Erythema migrans may resemble an uninfected tick bite, and if it rapidly expands (>1 cm/day) then disappears, it is more likely to be an allergic reaction to the tick saliva. Secondary erythema migrans lesions may have the appearance of erythema multiforme. Facial palsies can also be seen with herpes simplex type 1 virus or varicella-zoster virus. Arthritis may be diagnosed as reactive arthritis in adults or pauciarticular juvenile rheumatoid arthritis in children. Some patients have nonspecific complaints, including chronic fatigue and weakness that occur for months to years after a tick bite. These individuals warrant an evaluation for untreated Lyme disease as well as other possible causes of their chronic symptoms.
Management
Treatment guidelines, as recommended by the Infectious Diseases Society of America, vary by stage of disease and extent of neurologic involvement. For early localized or disseminated infection, the treatment of choice is oral doxycycline, 100 mg twice daily for 14 days. Second-line treatment is amoxicillin, which is useful for children younger than 8 years and pregnant women, for whom doxycycline is contraindicated.7 Third- and fourth-line treatments are cefuroxime and erythromycin, respectively. Duration of therapy and long-term outcomes in patients with early Lyme disease were assessed in a retrospective cohort study by Kowalski and coworkers.8 Of the 607 patients who met the study inclusion criteria, 93% were treated with doxycycline; 17% were treated for less than 10 days, 33% were treated for 11 to 15 days, and 47% were treated for more than 16 days. Patients treated for less than 10 days had long-term outcomes similar to those of patients treated with longer courses, and treatment failure was exceedingly rare.8
About 15% of patients with disseminated infection experience a Jarisch-Herxheimer–like reaction with an increase in systemic symptoms with fever, malaise, and increased size or intensity of the rash during the first 24 hours of therapy.2,7 Erythema migrans lesions usually resolve within 1 to 2 weeks after the initiation of antibiotic therapy, but systemic symptoms can take months to resolve.2,7
For patients with objective neurologic abnormalities, 2 to 4 weeks of intravenous ceftriaxone is advised.9 Lyme carditis can be treated with oral or parenteral antibiotics, although syncope, dyspnea, chest pain, or evidence of second- or third-degree heart block probably warrant hospitalization, intravenous therapy, and continuous monitoring.10 Temporary pacemakers may be required for advanced heart block but can be discontinued when the heart block resolves.10 Lyme arthritis does not necessarily warrant parenteral therapy, but if symptoms persist, re-treatment with a 4-week course of oral antibiotics or 2 to 4 weeks of parenteral ceftriaxone is advised. If symptoms improve but do not completely resolve, an additional 4-week course of oral antibiotics is favored. If patients have no resolution of symptoms despite parenteral therapy and if results of PCR testing of synovial fluid are negative, symptomatic treatment with nonsteroidal anti-inflammatory agents, intra-articular injections of corticosteroids, or disease-modifying antirheumatic drugs is recommended.9
Prevention
Prevention of Lyme disease is crucial until an effective vaccine is available and is best accomplished by avoidance of tick-infested areas. If this is not possible, protective clothing (long pants tucked into socks) and insecticides containing diethyltoluamide (DEET) or permethrin are effective at deterring ticks.11 Inspection of the entire body for ticks is invaluable and should include moist parts of the body, such as groin and axillae. Removal of a tick within 24 hours of attachment is sufficient to prevent Lyme disease. Routine use of antimicrobial prophylaxis (doxycycline, 200 mg orally once) can be considered when all four of the following conditions are met: (1) the attached tick can be reliably identified as an adult or nymphal I. scapularis tick, and it has been attached for less than 36 hours on the basis of engorgement or certainty about the time of exposure; (2) prophylaxis can be started within 72 hours of tick removal; (3) ecologic information indicates that the local rate of infection of the ticks with B. burgdorferi is greater than 20%; and (4) there is no contraindication to the use of doxycycline.11 There are no data to support the substitution of doxycycline with amoxicillin for prophylaxis.10 Patients who have removed attached ticks should be monitored closely for signs and symptoms of tick-borne disease for up to 30 days.12 This includes development or expansion of a skin lesion at the site of the tick bite or development of a viral-like illness.
The development of a Lyme disease vaccine has been challenging because B. burgdorferi spirochetes exploit tick proteins to establish an infection.13 The former vaccine against Lyme disease was based on anti-OspA (anti–outer surface protein A). Borrelia organisms upregulate OspA while entering the tick and bind to the tick receptor for OspA, which allows them to remain inside the tick between blood meals. The OspA vaccine was approved by the U.S. Food and Drug Administration (FDA) in 1998.13 It proved to be 80% protective against B. burgdorferi infection after three vaccine doses; however, high antibody titers did not persist long after vaccination, and additional boosters would have been required for immunity to be maintained. Therefore it was withdrawn from the market 4 years after it was released. Other vaccines are currently being investigated and include combining multiple Borrelia antigens and tick antigens to elicit a synergistic anti-Borrelia and anti-tick immune response. One such multivalent OspA candidate vaccine has been tested in 300 European participants in a phase I/II trial and was well tolerated with good levels of antibodies elicited.14,15
Complications
There has been much controversy over the incidence, prevalence, and pathogenesis of post–Lyme disease syndrome.16 When these patients are evaluated, it is necessary to begin with objective evidence of having had B. burgdorferi infection with positive ELISA results and IgG on WB testing. Post–Lyme disease syndrome describes a small percentage of patients with ongoing pain, neurocognitive, or fatigue symptoms lasting more than 6 months, despite resolution of objective manifestations of infection with antibiotic therapy; it is often indistinguishable from chronic fatigue syndrome or fibromyalgia. Compared with patients with active Lyme disease, these patients describe more generalized or disabling symptoms, often with an impact on their quality of life.17 There is no evidence to support the presence of an ongoing bacterial B. burgdorferi infection among patients who have completed the recommended treatment regimens for Lyme disease, although some people do continue to have ongoing symptoms, and this is an active area of investigation. One recent study showed elevated interleukin-23 (IL-23) levels and the presence of autoantibodies in a subset of these symptomatic individuals.18 Further antibiotic treatment is not indicated for patients with chronic subjective symptoms, and long-term antibiotic therapy is associated with well-known risks of side effects, selection of antibiotic-resistant bacteria, and perturbation of normal flora.19
Unfortunately, many patients who have been treated for early Lyme disease subsequently become reinfected after the first episode has resolved. Reinfection is defined as “the development of a new tick-transmitted infection with Lyme Borrelia occurring after successful antimicrobial treatment of a prior episode of Lyme disease.”12 This is distinct from relapse, which is defined as “the presence of objective clinical and/or microbiological evidence of persistent infection with Lyme Borrelia after a non-curative course of antimicrobial treatment.”12 It has been well documented that reinfection occurs only after treatment of early Lyme disease (almost always erythema migrans) and not after manifestations of late infection. Reinfection is clinically evident by a repeated episode of erythema migrans, at a skin site different from the previous episode, occurring more than 1 year after the initial episode. In addition, reinfection occurs during months when the nymphal stage of the tick vector is abundant in the environment. The rate of recurrence is actually higher than the incidence of Lyme disease in the general population.20 Proposed explanations for these findings include repeated tick bites (particularly in patients who live in endemic areas and who have low compliance with recommended preventive measures), immunologic factors (the immune response to erythema migrans is not fully protective), and microbiologic variation (evident by Borrelia strain variability as a means to circumvent host immune response). Furthermore, serologic testing is not useful in differentiating reinfection from initial infection, given the variability in IgM reactivity and potential for prolonged seroreactivity.20
Coinfection with other bacteria, specifically Babesia microti and Anaplasma phagocytophilum, may occur in patients with tick exposure in areas where these pathogens are endemic. Like B. burgdorferi, these organisms are also transmitted by the Ixodes tick species. Depending on the region, it has been reported that as many as 2% to 12% of patients with early Lyme disease may also have anaplasmosis and 2% to 40% may also have babesiosis, although the higher range of coinfection rates are limited to certain geographic locales.21 Diagnostic testing for coinfection should be considered in patients whose symptoms are more severe than typical Lyme disease or who have high-grade fevers for more than 48 hours despite appropriate antibiotic therapy; in those who have symptoms resembling a viral infection that fail to improve or worsen despite resolution of the skin lesion; and in those with leukopenia, thrombocytopenia, or anemia.7 These organisms will be further discussed in upcoming sections of the chapter.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree






