20 Thrombocytopenia
Thrombocytopenia is the most common coagulation disorder in the intensive care unit (ICU). Classically defined as a platelet count less than 150 × 109/L, thrombocytopenia is frequently classified according to whether platelets are consumed, sequestered, or underproduced in the bone marrow. However, a more practical classification takes into account the clinical setting (Table 20-1). In the ICU, thrombocytopenia occurs in up to 20% of all medical and 35% of all surgical admissions.1,2 It has many causes and results from the underlying disease plus the effects of medications that can impair platelet production and/or increase platelet consumption and destruction. The two most important causes of thrombocytopenia are sepsis and heparin-induced thrombocytopenia (HIT). Sepsis is associated with thrombocytopenia in 35% to 59% of cases, whereas HIT is the cause in approximately 25% of ICU patients.1–5 The highest incidence of HIT is among patients on high doses of unfractionated heparin.6 It is estimated that 2% of cardiac medical patients, 15% of orthopedic patients, and up to half of patients who undergo cardiac bypass surgery develop HIT antibodies against platelet factor 4 (heparin/PF4) following exposure to unfractionated heparin. However, most patients with heparin/PF4 antibodies do not develop thrombocytopenia, an important consideration when interpreting commonly available diagnostic tests that detect such antibodies.7 The most important complication observed in patients with HIT is not bleeding but thrombosis, which occurs 30 times more frequently in patients with HIT than in the general population.6
TABLE 20-1 Differential Diagnosis of Thrombocytopenia
| Outpatients |
| Non-ICU and MICU Inpatients |
| Coronary Care Unit Inpatients |
| Emergency Room Patients |
 Pathophysiology
Pathophysiology
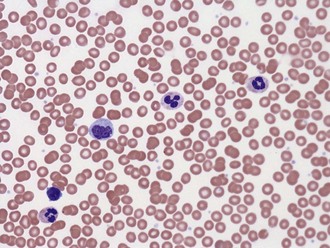
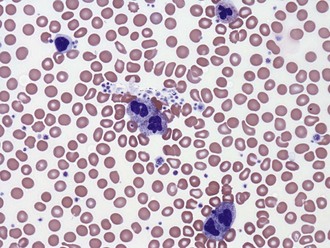
A common cause of low platelet count is test tube clumping of platelets due to ethylenediamine-tetraacetic acid (EDTA)-dependent antibodies or insufficient anticoagulant.8 When such “pseudothrombocytopenia” is considered as a possibility, the platelet count should be repeated in blood drawn into heparin- or citrate-containing tubes. Peripheral blood smears may help identify clumping platelets (Figures 20-1 and 20-2).
Immune mechanisms rarely contribute to sepsis-induced thrombocytopenia.8 Nonspecific platelet-associated antibodies can be detected in up to 30% of ICU patients. In these cases, nonpathogenic immunoglobulin G (IgG) presumably binds to bacterial products on the surface of platelets, to an altered platelet surface, or as immune complexes. A subset of patients with platelet-associated antibodies has autoantibodies directed against the integrin glycoprotein IIb/IIIa. These antibodies have been implicated in the pathogenesis of immune thrombocytopenic purpura and, although not proved, may also play a role in mediating sepsis-induced thrombocytopenia. Besides sepsis, many drugs also have been implicated in the production of nonspecific platelet antibodies, which is relevant, considering that the thrombocytopenia may be reversed by stopping the offending medication.9,10
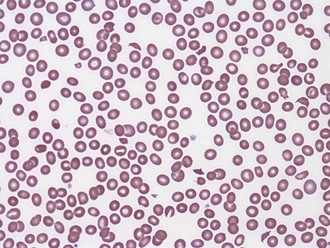
Nonimmune platelet destruction and/or consumption along with impaired production are the most important causes of thrombocytopenia in severe sepsis. There is increased binding of platelets to the activated endothelium, resulting in their sequestration, activation, and destruction. The inflammatory response to sepsis has been implicated directly in both impaired production and increased platelet destruction.4,5 Bone marrow specimens from patients with sepsis and thrombocytopenia often demonstrate hematophagocytosis.4,5 The degree to which this pathologic process is a cause or simply a marker of sepsis-related thrombocytopenia is unclear. Less commonly, thrombocytopenia is associated with underlying disseminated intravascular coagulation (DIC) and thrombotic microangiopathic disorders such as thrombotic thrombocytopenic purpura (TTP) and hemolysis-elevated liver enzymes and low platelet (HELLP) syndrome (Figure 20-3).11
< div class='tao-gold-member'>
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree