
Thoracolumbar Spine Fractures
Amy Kaji and Robert S. Hockberger
Thoracolumbar spine (TLS) injuries are relatively uncommon in the United States; however, of all blunt trauma patients presenting to the emergency department (ED), the rate of TLS injury is up to 15% (1). Although there are only approximately 40 cases per million population in the United States, spinal cord injury (SCI) predominantly afflicts productive young adults. Between 1973 and 1979, the average age at injury was 28.7 years, but as the median age of the general population has increased, the average age of injury has also increased (2). Since 2005, the average age at injury is 41. Over 80% of SCI occur among males, and the total annual cost to society from medical expenses and lost productivity is estimated to be over $5 billion. Statistics from the National Spinal Cord Injury Database (NSCID) reveal that motor vehicle–related collisions account for 39.2% of all SCI, followed in frequency by falls, and intentional acts of violence, such as gun shot wounds (2). At its peak, violence caused 24.8% of SCI between 1990 and 1999, but since 2005, it accounts for only 14.6% of SCI. Sports-related injuries have also decreased over time.
The human spine consists of 33 bony vertebrae: 7 cervical, 12 thoracic, 5 lumbar, 5 sacral, and 4 coccygeal. In the adult, the spinal cord ends at the level of the L1 vertebrae and then continues as the cauda equina. Due to its highly exposed location above the torso and its inherent flexibility, the cervical spine is the most commonly injured part of the spinal column (see Chapter 28). In contrast, the thoracic spine is rigidly fixed. The thoracic ribs articulate with the respective transverse processes and sternum, and a great amount of force is necessary to damage the thoracic spine. The middle of the thoracic spine is a vascular watershed area; thus, a vascular insult may lead to spinal cord ischemia. The second most commonly injured spine region is the thoracolumbar junction. The transition zone from thoracic to lumbar vertebrae is vulnerable to injury because of the juxtaposition of a rigidly fixed thoracic spine against a flexible lumbar spine. The spinal column also changes from a kyphotic curve to a lordotic curve at this level, and of all TLS injuries, 90% of the fractures occur in the region between T11 and L4. Allowing for more flexion and extension, the thoracolumbar junction facet joints are oriented differently when compared to other vertebral levels, and this is thought to concentrate greater forces at this level. Since the spinal canal is relatively wide at this level, however, thoracolumbar junction injuries rarely result in complete cord lesions and more commonly result in incomplete cord lesions (3).
CLINICAL PRESENTATION
Classification
White and Panjabi first described the concept of spinal instability, which they defined as the inability of the spine to maintain the anatomical relationships between vertebrae necessary to prevent neurologic injury or compromise (4). Since then, numerous classification schemes for TLS injuries have been reported. Utilizing results from a retrospective review of over 400 TLS injuries, Denis delineated a means to assess stability of vertebral fractures in which he divided the spinal column into three columns: anterior, middle, and posterior. The anterior column includes the anterior longitudinal ligament, the annulus fibrosus, and the anterior half of the vertebral body; the middle column comprises the posterior longitudinal ligament, the posterior annulus fibrous, and the posterior half of the vertebral body; whereas the posterior column includes the supraspinous and interspinous ligaments, as well as the facet joint capsule (Fig. 29.1) (4). According to this scheme, the stability of the spine is based upon the integrity of two of the three spinal columns, although Denis stipulated that the stability of the middle column determined the integrity of the spine. Denis used his three-column theory to distinguish major and minor TLS fractures. Spinal instability can also be inferred from plain radiographs as a loss of 50% vertebral height or an angulation at the thoracolumbar junction of greater than 20 degrees (5). The spine is also considered to be unstable in the presence of a neurologic deficit, since the spinal column has failed to protect the cord. In general, a stable fracture pattern in a neurologically intact patient may be treated nonoperatively.
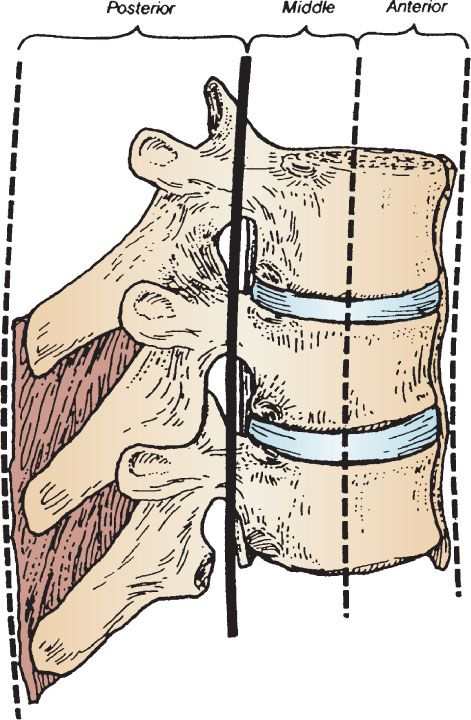
FIGURE 29.1 The three-column concept used to classify thoracic and lumbar spine fractures. (From Galli RL, Spaite DW, Simon RR. Fractures, dislocations, and major ligamentous injuries. In: Galli RL, Spaite DW, Simon RR, eds. Emergency Orthopedics: The Spine. Norwalk. Appleton and Lange; 1989, with permission.)
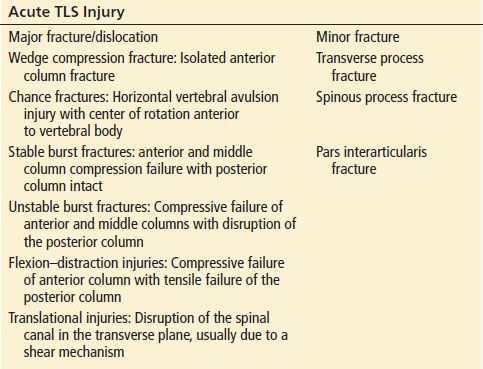
McAfee subsequently classified TLS injuries into five different patterns: wedge compression fractures, chance fractures, stable and unstable burst fractures, flexion–distraction injuries, and translational injuries. All of these fractures result from one or more of the three mechanisms of injury: axial compression, axial distraction, and translation (6). McAfee distinguished stable and unstable burst fractures based upon the integrity of the posterior ligament complex (6). A combination of Dennis’ division of major and minor fracture patterns and McAfee’s fracture–dislocation scheme is currently widely accepted and utilized (Table 29.1).
TABLE 29.1
Thoracolumbar Spine Injury Classification
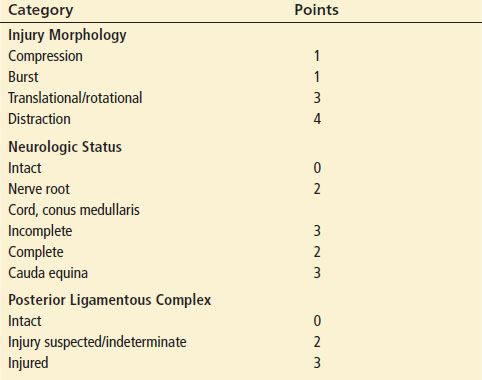
More recently, the Spine Trauma Study Group collaborated to create the Thoracolumbar Injury Classification and Severity Score (TLICS), which identifies three major injury characteristics to describe TLS injuries: injury morphology, posterior ligamentous complex integrity, and neurologic status (Table 29.2) (7). The injury morphology is categorized as one of the following four injury patterns: compression, burst, translational/rotational, or a distraction pattern (these are detailed further later in the chapter). The integrity of the posterior ligament complex, which consists of the supraspinous ligament, interspinous ligament, and facet joint capsules, can be assessed from plain radiographs, CT scans, and MRI. The neurologic status is graded in increasing order of severity as: neurologically intact, nerve root injury, complete SCI and incomplete SCI or cauda equina. Each characteristic is assigned a score and then summed to yield the TLICS. A score ≥5 suggests the need for operative treatment due to significant instability, whereas a score ≥3 suggests nonoperative treatment. A score of 4 may be treated either operatively or nonoperatively. The TLICS has yielded >90% agreement in the management of thoracolumbar trauma (8,9).
TABLE 29.2
Thoracolumbar Injury Classification and Severity Score Scale
Wedge Compression Fractures
Wedge compression fractures account for 50% to 70% of all TLS fractures and usually result from compressive failure of the anterior column after an axial load is applied in flexion. Simple wedge fractures are defined as demonstrating less than 10% compression, and there is generally no neurologic impairment since the middle column remains intact. Simple wedge fractures are stable, since pure flexion injuries do not disrupt the posterior ligament complex, and an additional rotational force is necessary to cause an unstable fracture pattern. However, if there is severe compression (>50%), kyphosis greater than 20 degrees, multilevel compression fractures, or a rotational component to the injury, then the posterior ligamentous complex may fail and progress to involve the middle column, resulting in spinal instability (6).
Wedge compression fractures generally result from falls, motor vehicle collisions, and occasionally generalized tonic–clonic seizures. Bilateral calcaneal fractures should alert the emergency physician to the possibility of a TLS fracture due to axial compression from a vertical plunge (4). Associated injuries are common, and fractures frequently coexist at other spinal levels. It is important to image patients older than 75 who complain of back pain, even after apparently minor injury, since 25% of this age group sustains osteoporotic compression fractures. In conscious patients who have no major distracting injury, there is invariably pain or tenderness at the site. While neurologic deficits are rare, wedge compression fractures are associated with a high incidence of intestinal ileus (3).
Best seen on lateral radiographs, simple wedge compression fractures demonstrate anterior compression of the vertebral body without any disruption of the posterior cortex (Fig. 29.2). The AP radiograph may demonstrate a subtle increase in the interspinous distance if there is a kyphotic deformity. Of note is that there is no vertebral subluxation, and thus, acute neurologic injury almost never occurs with a simple, single wedge compression fracture. It is important to ascertain that the posterior elements remain intact, since the integrity of the posterior cortex is the key feature that distinguishes the wedge compression fracture from an unstable burst fracture. However, standard radiographs may not be adequate to evaluate the integrity of the posterior vertebral cortex. In an analysis of 67 thoracolumbar radiographs reviewed by two radiologists and two orthopedists, 20% of the CT-confirmed burst fractures were initially misdiagnosed as wedge fractures (10). Thus, CT scan should be considered when plain radiographs demonstrate what appears to be a wedge compression fracture with any possible involvement of the posterior cortex, since plain radiographs are not accurate in determining involvement of the posterior wall of the vertebral body. Once an injury is identified, CT is better at delineating the bony structures and helps to demonstrate the integrity of the middle column, the degree of canal compromise, as well as subluxations and fractures of facets and lamina.
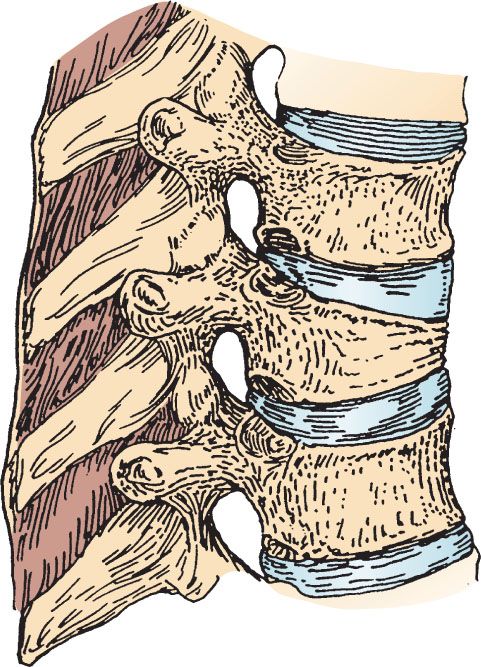
FIGURE 29.2 An anterior wedge fracture due to flexion in the thoracic region (ribs removed for visualization). (From Fractures, dislocations, and major ligamentous injuries. In: Galli RL, Spaite DW, Simon RR, eds. Emergency Orthopaedics the Spine. Appleton and Lange; 1989, with permission.)
Chance Fractures
Chance fractures account for only 5% of all TLS fractures and result primarily from a mechanism of distraction although there may be a minor component of flexion. The axis of flexion is anterior to the nucleus pulposus and the anterior longitudinal ligament. If the distraction forces are great enough, both the middle and posterior columns may be disrupted.
Chance fractures are usually seen in victims of automobile or airplane accidents who are wearing lap seat belts (3). Examination may reveal ecchymosis of the lower abdomen and tenderness at the fracture site, but the absence of these signs does not preclude the diagnosis. Although neurologic deficits occur in less than 5%, Chance fractures are commonly associated with intra-abdominal injuries, such as intestinal perforations, hematomas, and contusions.
Chance fractures are best seen on a lateral radiograph, which demonstrates a horizontal disruption through the spinous process, laminae, transverse process, pedicles, and the vertebral body (4). The height of the vertebral body is increased, and the distance between the spinous processes above and below the injury may appear to be widened (Fig. 29.3). The AP view may demonstrate an increased interspinous distance and a schism in the transverse processes. Routine axial CT scans of the spine frequently miss these fractures, since the image cuts are parallel to the level of the injury. Thus, sagittal reconstruction of CT images is recommended if a Chance fracture is suspected (4).
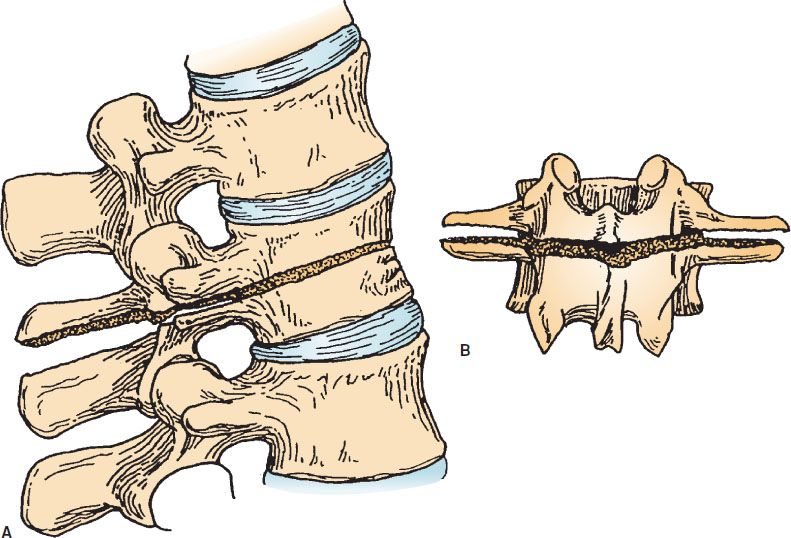
FIGURE 29.3 A “Chance” fracture created by a distraction mechanism. A: Lateral view. B: Posterior view. (From Fractures, dislocations, and major ligamentous injuries. In: Galli RL, Spaite DW, Simon RR, eds. Emergency Orthopaedics the Spine. Appleton and Lange; 1989, with permission.)









