Chapter 114 Thoracic Injuries in Children
Thoracic injuries in children are relatively uncommon, but result in disproportionate morbidity and mortality compared with other traumatic injuries, mainly because thoracic injuries often are associated with other life-threatening conditions and injuries. Children, unlike adults, undergo constant growth and change. Any consideration of the injured child must take into account several factors including age-related limitations in their ability to communicate and to understand their injuries, a limited ability to cooperate with care, and their potential for recovery, growth, and life-long productivity.1 Children with significant thoracic injuries require intensive monitoring and hemodynamic and respiratory support. It is important to establish an accurate diagnosis. High-resolution imaging techniques such as helical computed tomography (CT) are indicated to detect intrathoracic lesions. This chapter discusses the epidemiology, diagnosis, and immediate approach to children with thoracic injuries and the current management of specific injuries to the thorax.
Epidemiology
The National Pediatric Trauma Registry (NPTR) was created in 1994 and has collected information from 94 trauma centers in the United States. From 1994 to 2001, 3721 patients with thoracic injuries were reported, which corresponds to 7.7% of all pediatric trauma.2 Interestingly, isolated thoracic injuries accounted for only 0.7% of all pediatric trauma patients. Thoracic trauma occurs more frequently in males, with a male/female ratio of approximately 2:1. No differences in age distribution are noted. Blunt trauma is the most frequent cause of injury (92%). The incidence of penetrating chest injury in urban areas is increasing with the escalating use of firearms in society. However, penetrating injuries (gunshot wounds and stab wounds) currently account for only 8% of all thoracic injuries in the pediatric patient.2
An analysis of consecutive pediatric patients treated at a Level 1 trauma center found that the most common thoracic injuries were pulmonary contusion (48%), pneumothorax/hemothorax (39%), and rib fractures (32%).3 Thoracic injuries most commonly present concomitantly with other injuries.2–4 From 60% to 85% of children with thoracic injuries have significant injury to at least one other organ system, most notably the central nervous system (CNS), the abdominal cavity, or the musculoskeletal system.3,4 The most common mechanisms of injury are motor vehicle-related accidents (40.7%), children as pedestrians struck by a motor vehicle (19.2%), bicycle accidents (6.6%), and falls (5.8%). Additionally, abuse accounts for 7% to 8% of blunt trauma in children.5 The pediatric traumatologist must also be aware of other modes of blunt injury including skateboarding, skiing, snowboarding, sports injuries, fights, and suicide. The advent of “extreme sports” in geographically risky areas must also be kept in mind. Finally, the role of alcohol and drugs in injury must be addressed.1
The clinical importance of thoracic injuries is reflected in the greater severity of injury observed in children with thoracic injuries (Trauma Score [TS] 11, Injury Severity Scale [ISS] 27) compared with that seen in children without thoracic injuries (TS 15; ISS 7).4 According to the NPTR, the overall mortality for trauma in the pediatric population is 3%. Thoracic injuries are present in 33% of fatal cases. The mortality rate for thoracic trauma is 12.2%. In patients with thoracic trauma, CNS injuries are the major cause of death (63.1%), followed by uncontrollable hemorrhage (13.5%).2 The number and severity of associated injuries are important determining factors in the eventual outcome and survivability of the injury.3–6 Stratification of mortality rates according to the number and type of associated injuries illustrates this point. In isolation, thoracic trauma in children carries a 5% mortality rate. Children with abdominal and thoracic injuries have a 20% mortality rate; children with chest and head injuries have a 35% mortality rate; and children with all three injuries have a 39% mortality rate.4 Fortunately, immediately life-threatening chest injuries are infrequent; consequently, emergency thoracotomies in the operating room are required in only 3% to 6% of all pediatric thoracic trauma.7 Indications for emergency thoracotomy include victims of penetrating thoracic trauma who had signs of life at some point during the resuscitative efforts.8 The indication for emergency thoracotomy in blunt trauma (witnessed cardiac arrest in the emergency department) is controversial.
Anatomic and Physiologic Considerations with Chest Injuries
The injured child is not a small injured adult. The thoracic organs in a child exhibit different physiologic characteristics than in an adult. Increased cartilage content and incomplete ossification of the ribs make the thoracic cage more compliant than that of an adult, permitting the anterior ribs to be compressed against the posterior ribs.9 This compliance results in more kinetic energy being transmitted to intrathoracic organs without bony injury. Therefore pulmonary contusions without concomitant rib fractures are more common than in adults. Rib fractures and flail segments become more common as ossification occurs. The flail segment responds to changes in intrathoracic pressure rather than to the pull of respiratory muscles, resulting in retraction with inspiration and bulging with expiration. This paradoxical movement results in inefficient thoracic expansion and increased energy expenditure. Hypoventilation and subsequent atelectasis result from the associated pain.
The trachea is more compressible and narrower (narrowest at the level of the cricoid cartilage) early in life. Therefore children are susceptible to profound respiratory embarrassment from seemingly inconsequential insults (foreign body aspiration, etc.). A decreased functional residual capacity coupled with higher oxygen consumption per unit body mass leads to rapid development of hypoxemia in the traumatized child. This equalizes to adult values by age 8 to 10 years. Cardiac output in children is determined by heart rate and stroke volume. Contractility is largely fixed in early life. Children may compensate hemodynamically and maintain a normal blood pressure with up to a 40% blood loss. Additionally, the less complete fixation of the mediastinum in children allows more visceral shift, greater compromise of preload, and profound hypotension.1
Diagnosis and Immediate Management of Chest Injuries
The initial evaluation of the child with known or suspected thoracic trauma conforms to standard trauma protocols.10 Life-threatening diagnoses should be sought in the unstable child at each step of the evaluation during the primary survey (Box 114-1). First, the patency of the airway is established. The inability to maintain an airway because of anatomical obstruction or depressed level of consciousness (Glasgow Coma Scale [GCS] ≤8) warrants endotracheal intubation. All patients with suspected cervical injuries should have manual in-line cervical stabilization maintained during intubation. If endotracheal intubation is not possible, an age-appropriate surgical cricothyroidotomy should be performed.
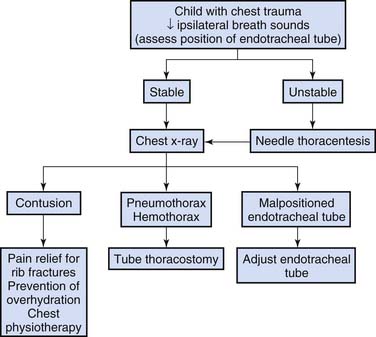
After the airway is secured, breathing is assessed. Both hemithoraces are observed for symmetrical motion and auscultation is performed to evaluate breath sounds. In the intubated patient the position of the endotracheal tube should be checked, looking for asymmetric chest expansion or decreased breath sounds, before any invasive procedures are performed. Arterial PaO2 analysis and pulse oximetry are useful for assessing oxygenation whereas PaCO2 level and capnography, where available, are extremely helpful for assessing ventilation. Capnography is being used increasingly in the emergency care of critically ill infants and children. It not only documents the correct intratracheal position of the endotracheal tube, but may also help to guide ventilation during transport. The stable child with decreased breath sounds on one side should undergo immediate chest radiography. A chest tube should be placed if either a pneumothorax or hemothorax is demonstrated. In an unstable child, needle thoracentesis should be performed immediately on the side with decreased breath sounds (Figure 114-1).
Additional clues to the nature of injuries are obtained by observation and palpation. Specifically, looking at the patterns of abrasions and contusions may suggest the mechanism of injury and allow prediction of potential intrathoracic injuries. One example is the child with a sternal contusion, who should be assessed for a cardiac contusion. The thoracic cage should be palpated from under the arms to the abdomen in a sequential fashion, looking for rib tenderness and/or flail segments. Chest radiography completes the initial evaluation. The physician checks the x-ray film for evidence of pneumothorax, hemothorax, pulmonary contusion, and rib fractures. First and second rib fractures do not seem to be reliable indicators of aortic injury in children, but may be related to other significant vascular injuries (subclavian artery).11–13 In general, approximately 60% of patients with a thoracic trauma diagnosis are admitted to the pediatric intensive care unit for further monitoring and management.3,14
Rib Fractures
Fractures of the bony thorax, specifically rib fractures, are more common than previously suspected.3,6,15 In one large study, rib fractures were noted in 32% of all children with thoracic injuries.4 However, in the context of all injured children admitted, rib fractures were infrequent and were observed in only 1.6% of injured children. Again, the pediatric experience stands in sharp contrast to the adult experience, in which rib fractures are frequently seen and are present in 33% of injured adult patients.6 The importance of rib fractures as a marker of injury severity has been emphasized.11 In one study, rib fractures were noted in only 1.6% of children admitted. However, the mortality rate of children with rib fractures was 42%, compared with a 2.1% mortality rate in children without rib fractures. When a head injury is associated, children with rib fractures have a disproportionately higher mortality rate of 71%. In addition, head injury and the number of ribs fractured correlate with risk of mortality in children.14
The mechanisms of injury resulting in rib fractures parallel those seen in other pediatric thoracic injuries, with the notable exception of the high incidence of intentional injury in younger children. Traffic injuries accounted for nearly 70% of all rib fractures, whereas child abuse accounted for 21%. The mean age of children with rib fractures is 4.7 years, and nearly 60% of children with rib fractures are 4 years or younger. It is noteworthy that child abuse accounts for nearly two thirds of rib fractures in children younger than 3 years.14 The number of fractured ribs in both injured adults and children correlates directly with the severity of injury (assessed by the Revised Trauma Score [RTS] and the ISS), the likelihood of multisystem and intrathoracic injury, and higher mortality rates.14,16 Presence of three or more rib fractures in a child reliably identifies him or her as having a significant likelihood of intrathoracic, as well as other organ involvement, and a significantly higher probability of dying.6
First and second rib fractures in children do not correlate with the presence of concomitant injury to the mediastinal great vessels and, in isolation, do not warrant aortography.3,14,17 Additionally, neither posterior rib fractures nor scapular rib fractures were indicative of great vessel injury. However, first and second rib fractures are associated with pulmonary contusions, cervical spine injuries, and injuries to intrathoracic vessels and nerves.13–19 Moreover, evidence suggests that the presence of thoracic spine fractures should heighten the suspicion of great vessel injury.20 Lower rib fractures may be associated with liver and spleen injuries.21
The key to successful management of chest wall injuries is adequate pain control to promote effective air exchange and to facilitate pulmonary toilet.6,22,23 The goal is to prevent atelectasis and pneumonia. Regional anesthetic techniques, such as epidural and intercostal nerve blockade, play an expanding role in pain control and are increasingly viewed as effective and safe adjuncts to traditional analgesia techniques.22,23
Flail segments result from multiple contiguous ribs with more than two points of fracture, fracture of the sternum and multiple costochondral junctions, or midaxillary fracture with fracture or dislocation of rib heads.1,24 A 17-year review of 225 children treated for chest trauma revealed no incidences of flail chest.24 These injuires are quite rare in children. For flail chest injury patients, an ISS greater than 23, the need for blood transfusions within the first 24 hours, and the presence or development of shock on admission are suggested as factors that predict the need for ventilatory assistance.22 These assertions stem from an analysis of adult patients. Their validity in the treatment of children awaits further evaluation. Fortunately, the majority of children with fractured ribs do not require ventilatory assistance and have a good overall prognosis.14
Clavicle, Sternal, and Scapular Fractures
The medial physis of the clavicle does not typically close until 23 to 25 years of age.25 Because of this, falls on the shoulder may lead to posterior sternoclavicular physeal fracture-dislocations in children. These injuries can be associated with dysphagia, dyspnea, and brachiocephalic compression.26 The clinician must evaluate for esophageal and great vessel injuries in this population. Sternal fractures in children can occur from motor vehicle collisions, direct blows, or flexion-compression of the spine.27–29 Although rare, these types of fractures may be associated with blunt cardiac injury.30,31 All patients with sternal fractures or sternal bruising should be assessed for a cardiac contusion.
Scapular fractures are uncommon in children.32 A significant amount of force is required to fracture the scapula. Scapular fractures are associated with rib fractures, pulmonary contusion, and head injury. Axillary artery or brachial plexus injury may also occur.33
Children with symptomatic chest wall injuries should have imaging performed to identify the fractures and associated intrathoracic injuries. Children with suspected posterior sternoclavicular fractures/dislocations, first rib fractures, and sternal fractures should be evaluated with CT imaging to evaluate the great vessels and intrathoracic organs.34 Additionally, an electrocardiograph should be obtained in children with sternal fractures.35 Any abnormal rhythm should lead to an echocardiogram and cardiac enzyme analysis to exclude blunt cardiac injury.31
Pulmonary Contusion
Pulmonary contusion rivals pneumothorax/hemothorax as the most common childhood thoracic injury. It is present in as many as 48% of children with thoracic injuries.3,4 Pulmonary contusion is defined as nonanatomical areas of consolidation on chest radiograph or CT. Evidence suggestive of pulmonary contusion, such as external chest wall abrasions, tachypnea, and abnormal breath sounds, is frequently absent in children. Automobile crashes represent the most common mechanism of injury. Pulmonary contusion is usually associated with other potentially more life-threatening conditions such as pneumothorax/hemothorax or other systemic injuries.4,14,36–38
Rib fractures are present in up to 32% of children with intrathoracic injuries.4,14,36–38 Up to 40% of cases of pulmonary contusion and other intrathoracic lesions were not radiographically evident until 48 hours after injury.36 Thus rib fractures are important markers of internal injuries because the radiographic manifestations of other intrathoracic injuries are often delayed. When pulmonary contusion is accompanied by rib fractures, serial chest radiographs should be performed during the initial 48 hours after injury to promptly identify other intrathoracic injuries.36 Although most patients with pulmonary contusion are identified by sequentially obtained chest radiographs, CT imaging may be of greater value in demonstrating posttraumatic intrathoracic pathology in patients requiring endotracheal intubation and mechanical ventilation. For patients with an oxygenation index (PaO2/FiO2) less than 300, a CT scan may be helpful in defining the extent of pulmonary contusion and identifying those patients at higher risk for acute respiratory failure or those with unsuspected or incompletely treated hemothoraces or pneumothoraces.39
Management of pulmonary contusion centers on oxygen supplementation, judicious fluid management, pain control, adequate pulmonary toilet, and respiratory support. Many children with thoracic trauma exhibit wet lung, a syndrome characterized by a combination of pulmonary contusion, pneumonia, and atelectasis.24,40 However, concern for wet lung should not compromise appropriate volume resuscitation during the initial evaluation. Corticosteroids are ineffective and probably harmful.36 Prognosis for most children with pulmonary contusion is excellent, because the majority of these injuries are mild to moderate in severity, and children recover without the need for ventilatory support. For severe pulmonary contusions, differential lung ventilation may be valuable.41–43 Early success of synchronized independent lung ventilation using a double-lumen endobronchial tube connected to two ventilators indicates a potentially lifesaving treatment option for the child with a significant pulmonary contusion.37 Early institution of synchronized independent lung ventilation may increase survival in the severely injured patient with pulmonary contusion.3,4,37,38,44 Extracorporeal life support measures may increase the risk of posttraumatic bleeding complications.1 Approximately 20% of children with pulmonary contusion develop pneumonia, a risk factor for developing respiratory failure. Half of the children who develop respiratory insufficiency do so in the first few hours after injury.40 Few develop true adult respiratory distress syndrome (PaO2/FiO2 <200), and death primarily related to the pulmonary contusion is rare in children.40,45
Traumatic Asphyxia
Traumatic asphyxia results from direct compression of the chest from crushing injury in conjunction with a deep inspiration and closed glottis. This results in a marked increased in intrathoracic pressure that is transmitted from the right atrium directly through the valveless superior and inferior vena cava, causing rupture of venules and capillaries of the face and head. A rapid increase in intracranial pressure may also occur.44 Clinical manifestations include conjunctival hemorrhage, facial edema and cyanosis, ecchymotic or petechial hemorrhages of the chest and face, hemoptysis, epistaxis, hemotympanum, and exophthalmos.46 Retina, vitreous body, or optic nerve hemorrhage may result in loss of vision. Associated neurologic symptoms include altered mental status, brachial plexus injuries, quadriplegia (without evidence of spinal cord injury), and coma.47 Interestingly, while clinical manifestations of traumatic asphyxia can be quite dramatic, morbidity and mortality are generally due to associated injuries. For those children that survive the initial traumatic insult, the dramatic clinical manifestations usually resolve with no neurologic sequelae.
Pneumothorax/Hemothorax
Pneumothorax and hemothorax collectively represent the second most common intrathoracic injuries seen in children.3,4,36 Together, they account for 39% to 50% of childhood intrathoracic injuries. Among all children who sustain thoracic trauma, approximately one third will develop a pneumothorax.3,4 One third of the pneumothoraces occur in isolation.3 The remainder will have associated intrathoracic and extrathoracic injuries. The majority (76%) of chest injuries resulting in pneumothorax or hemothorax require only a tube thoracostomy for successful management.3,4,48 One of the most common mistakes in managing a significant hemothorax is placing a chest tube that is not large enough to adequately evacuate the blood (Table 114-1). Tube thoracostomy is best performed with the upper extremity fully abducted. This position elevates the ribs and widens the intercostal space, facilitating the placement of the chest tube, which may be both diagnostic and therapeutic. The chest tube is inserted more caudally and more posteriorly for a suspected hemothorax than for a pneumothorax. Ideally, the fifth intercostal space is used along the midaxillary line. At this level, there is little danger to the long thoracic nerve, and relatively little risk to the liver or spleen. More posterior placement of the tube can result in obstruction of the tube when the child lies in the supine position.
Table 114–1 Chest Tube Sizes by Patient Weight
| Age | Weight | Chest Tube Size |
|---|---|---|
| Newborn to 1 year | 3–5 kg | 10–12 Fr |
| ≥1 year to 2 years | 6–9 kg | 12–16 Fr |
| 3 years to 4 years | 10–11 kg | 16–20 Fr |
| 12–14 kg | 20–22 Fr | |
| 5 years to 7 years | 15–18 kg | 22–24 Fr |
| 19–22 kg | 24–28 Fr | |
| 8 years to 11 years | 23–30 kg | 28–32 Fr |
| ≥12 years | >30 kg | 32–42 Fr |
Data from Bliss D, Silen M: Pediatric thoracic trauma, Critic Care Med 30(11):S409-S415, 2002.
Because of the low arterial pressure in the pulmonary circulation, bleeding from tears in the lung parenchyma is slow and hemostasis occurs early after the lung is reexpanded. Prompt drainage of blood in the thorax is necessary for several reasons, including prevention of lung entrapment secondary to hemothorax organization, prevention of infection (empyema), and accurate quantification of the amount of hemorrhage.1 Exsanguinating hemorrhage usually involves intercostal, hilar, or mediastinal vessels. Thoracotomy is indicated when the initial thoracostomy tube output is greater than or equal to 20% to 30% of the blood volume, when the output is greater than 2 to 3 mL/kg/hr over the following 6 hours, or when significant rebleeding occurs.49
It is widely accepted that the erect chest radiograph with posteroanterior and lateral projections is highly accurate in demonstrating major intrathoracic pathology. However, with the overriding concern for possible cervical spine injury, chest radiographs during trauma resuscitation usually are taken with the child in the supine position. In that position, small and even modest collections of air may not be readily demonstrated. Although the portable chest x-ray film has a well-defined role during assessment of thoracic injuries, its limitations must be borne in mind.48
Whenever possible, standing anteroposterior and lateral chest x-ray images should be obtained as soon as the clinical condition allows. Some authorities, noting the lower sensitivity of chest radiographs, recommend that emergent chest CT scans be performed in stable patients with blunt high-energy torso trauma, cross-body injury patterns, or mechanisms of injury suggestive of chest trauma.16,38,50 The focused assessment sonography for trauma (FAST) in the setting of thoracic trauma is useful for detecting fluid in the pleural cavity and has 95% sensitivity in detecting pneumothoraces compared with chest radiographs.51 However, a recent meta-analysis evaluating FAST for abdominal injuries in children noted a sensitivity of 80% and specificity of 96%. When only the most methodologically stringent articles were used (six studies), the combined sensitivity of the FAST exam for identifying children with hemoperitoneum was 66%. Sensitivity for detection of all children with intra-abdominal injuries (including those without hemoperitoneum) was even lower at 50%.52,53 The continued role of FAST in evaluating the child with thoracic injuries remains to be seen.
The increased mobility of the child’s mediastinum places the pediatric patient at increased risk for the physiologic consequences of a tension pneumothorax, which may occur in 25% of children presenting with a pneumothorax.3 However, as the mediastinum becomes more fixed, shifting is less likely. In older children and adolescents, tension physiology may be due to progressively less effective ventilation and oxygenation caused by increased intrathoracic pressure.54 The traumatologist must also keep in mind other causes of hypoxemia and hypotension including cardiac tamponade, right mainstem position of the endotracheal tube (ETT), ETT obstruction, and gastric distension.1 Fortunately, in the majority of cases, pneumothorax results from small disruptions of the lung parenchyma. These disruptions are associated with small to modest air leaks and are effectively treated with a tube thoracostomy.4,11,55,56