EPIDEMIOLOGY
An estimated 450,000 individuals in the United States receive medical treatment each year for burn injuries. Although 40,000 patients require hospitalization and more than 60% of those are treated at one of 127 specialized burn centers,1 the vast majority of burn patients are treated in the acute setting by emergency physicians and discharged with outpatient follow-up.2,3
Nearly 70% of burn victims are male,1 and risk is highest between the ages of 18 and 35. Seventy-seven percent of all injuries are accounted for by fire or scalding; 43% of scald injuries occur in children less than 5 years of age.4 Although overall survival exceeds 96%, fire, burn, and smoke inhalation still account for approximately 3400 deaths each year in the United States.1 Elderly patients understandably have a disproportionately higher death rate.4,5,6 The risk of death from a major burn increases with larger burn size, older age, the presence of inhalation injury, and female sex.6
The Centers for Disease Control and Prevention lists the following groups as being at increased risk of fire-related injuries and death: children ≤4 years of age, adults ≥65 years of age, African Americans and Native Americans, persons living in rural areas, persons living in manufactured homes or substandard housing, and persons living in poverty.7
Care of the acute burn–injured patient has improved significantly over the last several decades.8,9 The rate of hospital admissions has decreased owing to improvements in both the acute care provided in the ED and outpatient care at specialized burn centers. Only approximately 4% of those treated in specialized burn treatment centers die from their injuries or associated complications.4,10
PATHOPHYSIOLOGY
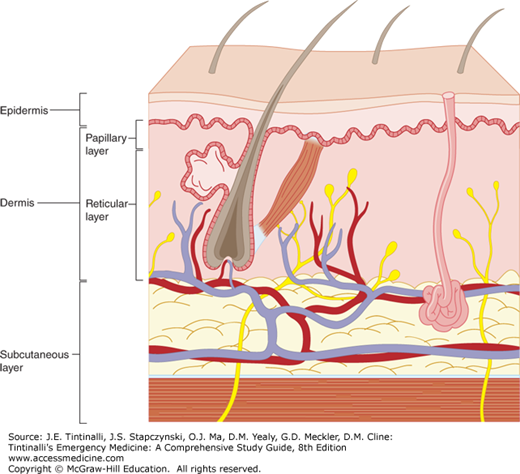
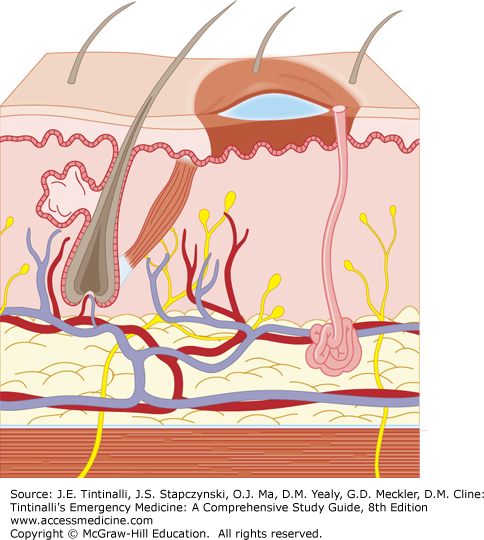
Skin consists of two layers: the epidermis and the dermis (Figure 216-1). Skin thickness varies both by age and anatomic location: it is relatively thinner at extremes of age, whereas it is thicker on the palms, soles, and upper back. Thus, the depth and severity of thermal injury varies by both the age of the victim and the anatomic location exposed.
Skin functions as a semipermeable barrier to evaporative water loss, protects against environmental assault, and aids in the control of body temperature, sensation, and excretion. Partial-thickness thermal injury disrupts these barrier functions and contributes to free water deficits. This effect may be significant with moderate to large burns.
Thermal injury results in a spectrum of local and systemic homeostatic disorders that contribute to burn shock (Table 216-1). These include disruption of normal cell membrane function, hormonal alterations, acid-base disturbance, hemodynamic changes, and hematologic derangement.
Disruption of sodium pump Intracellular influx of sodium and water Extracellular efflux of potassium Depression of myocardial contractility (>60% of body surface area burned) Increased systemic vascular resistance Metabolic acidosis Increase in hematocrit and increased blood viscosity Secondary anemia from erythrocyte extravasation and destruction Local tissue injury Release of histamines, kinins, serotonins, arachidonic acids, and free oxygen radicals |
The fluid and electrolyte abnormalities seen in burn shock are largely the result of alterations of cell membrane potential causing intracellular influx of water and sodium, and extracellular migration of potassium, secondary to dysfunction of the sodium pump. In patients with burns greater than 60% of total body surface area, depression of cardiac output results in a lack of response to aggressive volume resuscitation. Although disputed by others, Baxter and Shires11 have explained this phenomenon on the basis of circulating myocardial depressants. Systemic vascular resistance is increased. A significant metabolic acidosis may be present even in the early stages of a large burn injury. Massive thermal injury results in an increase in hematocrit with increased blood viscosity during the early phase, followed by anemia from erythrocyte extravasation and destruction. Surprisingly, however, transfusion is seldom required for patients with isolated burn injury, and aggressive transfusion has been associated with increased morbidity and mortality.12,13,14
Thermal injury is progressive. Local effects of thermal injury include the liberation of vasoactive substances, disruption of cellular function, and formation of edema. The subsequent systemic response alters the neurohormonal axis and further extends the injury. Implicated in these events are histamine, kinin, serotonin, arachidonic acid metabolites, and free oxygen radicals. These substances exert their primary effects at the local level and cause progression of the burn wound. Although many factors may influence prognosis, the severity of the burn, the presence of inhalation injury, associated injuries, the patient’s age, comorbid conditions, and acute organ system failure are most important.5,6 Cell damage occurs at temperatures of >45°C (113°F) owing to denaturation of cellular protein. The size and depth of the resulting burn are functions of the burning agent, its temperature, and the duration of exposure. Burn wounds are described as having three zones: the zone of coagulation, in which tissue is irreversibly destroyed with thrombosis of blood vessels; the zone of stasis, in which there is stagnation of the microcirculation; and the zone of hyperemia, in which there is increased blood flow. The zone of stasis can become progressively more hypoxemic and ischemic if resuscitation is not adequate. In the zone of hyperemia, there is minimal damage to the cells and spontaneous recovery is likely.
CLINICAL FEATURES
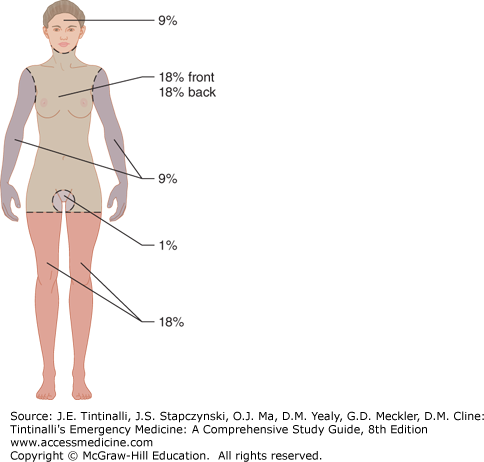
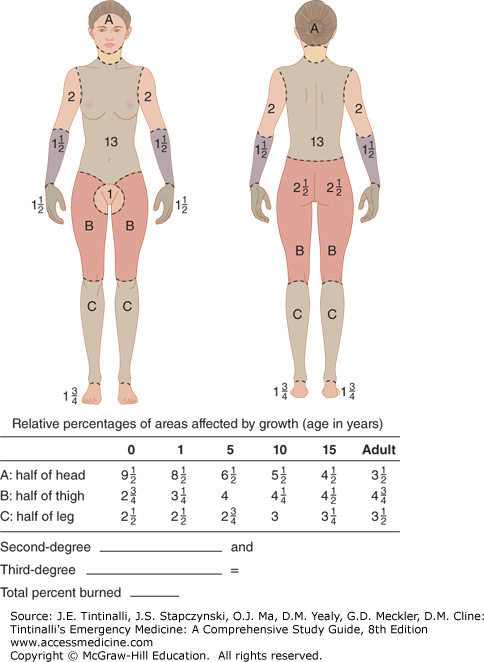
The size of a burn injury is quantified as the percentage of body surface area involved.9 The Rule of Nines is a simple and commonly used method to calculate burn size (Figure 216-2), It divides the body into segments that are approximately 9% or multiples of 9%, with the perineum forming the remaining 1%. Because of the proportionately larger heads and smaller legs of infants and children, this method must be modified in pediatric burn injury.
A second method assumes that the area of the back of the patient’s hand is approximately 1% of their total body surface area. The number of “hands” that equal the area of the burn can approximate the percentage of body surface area burned. A third and more precise method uses the Lund-Browder burn diagram (Figure 216-3). This allows an accurate age-adjusted determination of burn size for a given depth, allowing for the anatomical differences of children.15
Experienced burn care nurses and physicians can reliably estimate burn size regardless of the method used. Although it is common for inexperienced individuals to estimate burn size incorrectly when patients are first assessed in the ED, it remains a vital determinant of both fluid resuscitation and the need for ultimate transfer.
The depth of a burn has historically been described in degrees: first, second, third, and fourth (Table 216-2). However, a classification of burn depth according to the need for surgical intervention has become the accepted approach in burn treatment centers: superficial partial-thickness, deep partial-thickness, and full-thickness burns8 (Table 216-3). Determination of burn depth requires clinician judgment using commonly observed wound features. There is no objective method of measuring burn depth, and burn wound biopsy is not routine practice.
| Burn Depth | Histology/Anatomy | Example | Healing |
|---|---|---|---|
| Superficial (first degree) | Epidermis | Sunburn | 7 d |
| No blisters, painful | |||
| Superficial partial-thickness (superficial second degree) | Epidermis and superficial dermis | Hot water scald | 14–21 d, no scar |
| Blisters, very painful | |||
| Deep partial-thickness (deep second degree) | Epidermis and deep dermis, sweat glands, and hair follicles | Hot liquid, steam, grease, flame | 3–8 wk, permanent scar |
| Blisters, very painful | |||
| Full-thickness (third degree) | Entire epidermis and dermis charred, pale, leathery; no pain | Flame | Months, severe scarring, skin grafts necessary |
| Fourth degree | Entire epidermis and dermis, as well as bone, fat, and/or muscle | Flame | Months, multiple surgeries usually required |
| Burn Classification | Burn Characteristics | Disposition |
|---|---|---|
| Major burn | Partial-thickness >25% BSA, age 10–50 y | Burn center treatment |
| Partial-thickness >20% BSA, age <10 y or >50 y | ||
| Full-thickness >10% BSA in anyone | ||
| Burns involving hands, face, feet, or perineum | ||
| Burns crossing major joints | ||
| Circumferential burns of an extremity | ||
| Burns complicated by inhalation injury | ||
| Electrical burns | ||
| Burns complicated by fracture or other trauma | ||
| Burns in high-risk patients | ||
| Moderate burn | Partial-thickness 15%–25% BSA, age 10–50 y | Hospitalization |
| Partial-thickness 10%–20% BSA, age <10 y or >50 y | ||
| Full-thickness burns ≤10% BSA in anyone | ||
| No major burn characteristics present | ||
| Minor burn | Partial-thickness <15% BSA, age 10–50 y | Outpatient treatment |
| Partial-thickness <10% BSA, age <10 y or >50 y | ||
| Full-thickness <2% in anyone | ||
| No major burn characteristics present |
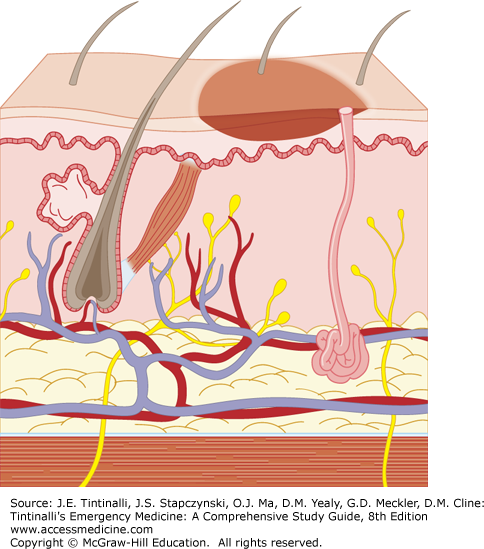
A superficial burn involves only the epidermal layer of skin. Sunburn is frequently given as an example, even though it is caused by ultraviolet light instead of thermal injury.16 The burned skin is red, painful, and tender without blister formation. Superficial burns usually heal in about 7 days without scarring and require only symptomatic treatment (Figure 216-4).
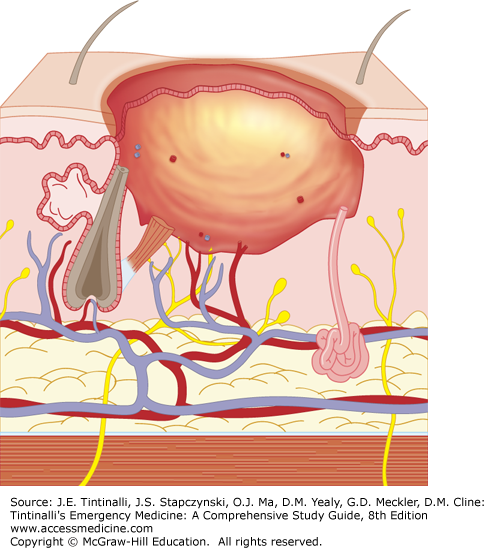
Partial-thickness burns extend into the dermis and are subdivided into superficial partial-thickness (Figure 216-5) and deep partial-thickness burns (Figure 216-6).
In superficial partial-thickness burns, the epidermis and the superficial dermis (papillary layer) are injured while the deeper layers of the dermis, hair follicles, and sweat and sebaceous glands are spared. Superficial partial-thickness burns are often caused by hot water scalding. The skin is blistered, and the exposed dermis is red and moist. These wounds are exceedingly painful to touch. The dermis is well-perfused with intact capillary refill. Healing typically occurs in 14 to 21 days, scarring is usually minimal, and there is full return of function.
Deep partial-thickness burns extend into the deep dermis (reticular layer) (Figure 216-6). Hair follicles and sweat and sebaceous glands are damaged, but their deeper portions usually survive. Hot liquids (e.g., oil or grease), steam, or flame usually cause this type of injury. The skin may be blistered, and the exposed dermis is pale white to yellow in color. The burned area does not blanch; it has absent capillary refill and absent pain sensation. Deep partial-thickness burns may be difficult to distinguish from full-thickness burns. Healing takes 3 weeks to 2 months; scarring is common and related to the depth of the dermal injury. Surgical debridement and skin grafting may be necessary to obtain maximum function.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree