Study objective
Lumbar puncture is a commonly performed procedure, although previous studies have documented low rates of successful completion in infants. Ultrasonography can visualize the anatomic landmarks for lumbar puncture and has been shown in some studies to reduce the failure rate of lumbar puncture in adults. We seek to determine whether ultrasonography-assisted site marking increases success for infant lumbar punctures.
Methods
This was a prospective, randomized, controlled trial in an academic pediatric emergency department (ED). We enrolled a convenience sample of infants younger than 6 months between June 2014 and February 2016 and randomized them to either a traditional lumbar puncture arm or an ultrasonography-assisted lumbar puncture arm. Infants in the ultrasonography arm received bedside ultrasonography of the spine by one of 3 study sonographers before lumbar puncture, during which the conus medullaris and most appropriate intervertebral space were identified and marked. The lumbar puncture was then performed by the predetermined ED provider. Our primary outcome was successful first-attempt lumbar puncture. Subjects were considered to have a successful lumbar puncture if cerebrospinal fluid was obtained and RBC counts were less than 1,000/mm 3 . All outcomes were assessed by intention-to-treat analysis.
Results
One hundred twenty-eight patients were enrolled, with 64 in each arm. No differences between the 2 arms were found in the baseline characteristics of the study subjects and providers, except for sex and first-attempt position. The first-attempt success rate was higher for the ultrasonography arm (58%) versus the traditional arm (31%) (absolute risk difference 27% [95% CI 10% to 43%]). Success within 3 attempts was also higher for the ultrasonography arm (75%) versus the traditional arm (44%) (absolute risk difference 31% [95% CI 15% to 47%]). On average, performing bedside ultrasonography on 4 patients (95% CI 2.1 to 6.6) resulted in 1 additional successful lumbar puncture.
Conclusion
Ultrasonography-assisted site marking improved infant lumbar puncture success in a tertiary care pediatric teaching hospital. This method has the potential to reduce unnecessary hospitalizations and exposures to antibiotics in this vulnerable population.
SEE EDITORIAL, P. 620 .
Introduction
Background
What is already known on this topic
Lumbar puncture is difficult to perform on infants.
What question this study addressed
Does the use of ultrasonography-assisted site marking increase success rate for infant lumbar puncture?
What this study adds to our knowledge
In this randomized controlled trial with 128 children, the use of bedside ultrasonographic marking by 2 individuals was associated with a 27% absolute improvement in success of lumbar puncture.
How this is relevant to clinical practice
This study suggests that ultrasonography-assisted site marking improves infant lumbar puncture success, although it remains to be seen how generalizable the results are.
Bedside ultrasonography possesses the ability to visualize the anatomic landmarks of lumbar puncture, including the subarachnoid space and conus medullaris in infants. In the adult literature, the effect of ultrasonography assistance on lumbar puncture success is equivocal. In the pediatric population, ultrasonography has been used to determine optimal patient positioning for lumbar puncture, to increase confidence of the lumbar puncture insertion site, to help disclose the reason for a failed lumbar puncture, and to mark the lumbar puncture insertion site. In simulation, it has been demonstrated that physicians inexperienced with ultrasonography can easily obtain the requisite anatomic images for lumbar puncture. Few studies have investigated the effect of bedside ultrasonography on lumbar puncture success rate in pediatric patients. To our knowledge, no randomized studies have been published on the use of ultrasonography for infant lumbar puncture. In theory, through visualization of anatomic landmarks and marking of the most appropriate insertion site, ultrasonography-assisted site marking could affect lumbar puncture success.
Importance
Increasing the proportion of successful lumbar punctures with ultrasonography assistance has many implications. First, it would reduce pain and discomfort through reduction of total attempts and total procedure time. Second, it could significantly reduce the rate of unnecessary hospitalizations, additional interventional procedures, and antibiotic use. Third, it would offer a significant cost savings through improvement of the diagnostic and management process. In one recent retrospective study of low-risk infants aged 28 to 60 days, those who had unsuccessful lumbar punctures were hospitalized more frequently and had higher median hospital charges than those with successful lumbar punctures, despite similar serious bacterial infection rates.
Goals of This Investigation
The goals of this investigation were to determine the effect of bedside ultrasonography-assisted site marking on the proportion of successful infant lumbar punctures (on first attempt and within 3 attempts) compared with the traditional approach. In addition, we sought to determine whether the ultrasonography intervention decreased hospitalization length of stay. We hypothesized that ultrasonography-assisted site marking would increase the proportion of successful lumbar punctures and therefore decrease length of stay.
Materials and Methods
Study Design and Setting
We performed a prospective, nonblinded, randomized, controlled trial in an urban academic pediatric emergency department (ED) that has more than 90,000 pediatric patients per year and is staffed with medical students, nurse practitioners, trainees, and attending physicians. Trainees included residents of various specialties (pediatrics, medicine-pediatrics, emergency medicine, family medicine, and psychiatry) and pediatric emergency medicine fellows. There were no specific lumbar puncture training efforts in place, aside from standard hospital credentialing policy for procedures, during the entirety of this study. The institutional review board approved this study.
Selection of Participants
We recruited a convenience sample of infants aged zero to 6 months during a 20-month period from June 2014 to February 2016. Eligible patients were drawn from the study site ED. Inclusion criteria were infants aged 6 months or younger and receiving a lumbar puncture. Research assistants screened patients on the ED tracking board for eligibility. Exclusion criteria included known spinal cord abnormality, such as tethered cord, or parents who were non-English speaking. Sampling of patients was limited to study sonographer availability, given that the study arm was revealed only after randomization. As per institutional protocol, verbal consent for lumbar puncture was obtained by the provider, and written informed consent was subsequently obtained by a study investigator before enrollment.
Interventions
A block randomization sequence was generated with random-sized blocks before the start of the study to ensure that treatment groups were evenly distributed throughout the study duration. The sequence was kept in a password-secured spreadsheet and was not available to the study investigators. Allocation concealment occurred through storage in sealed envelopes containing premarked group assignment and study numbers. During the study period, any medical student, nurse practitioner, trainee, or attending physician was eligible to perform the lumbar puncture; however, to minimize potential bias, the clinician performing the lumbar puncture was identified before randomization. Once the subject was consented and enrolled, the next envelope in line was selected by a research assistant to assign the subject to a treatment arm. For patients randomized to the traditional lumbar puncture arm, no additional intervention was made and clinicians proceeded with lumbar puncture based on the traditional landmark approach. For patients randomized to the ultrasonography-assisted lumbar puncture arm, bedside ultrasonography was performed with a Mindray M7 (Mindray North America, Mahwah, NJ) linear high-frequency transducer before lumbar puncture to identify anatomic landmarks ( Figure 1 ) and to mark the insertion site.
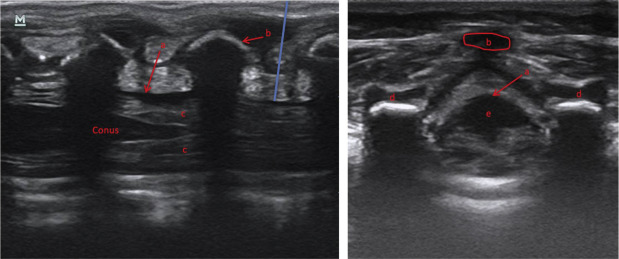
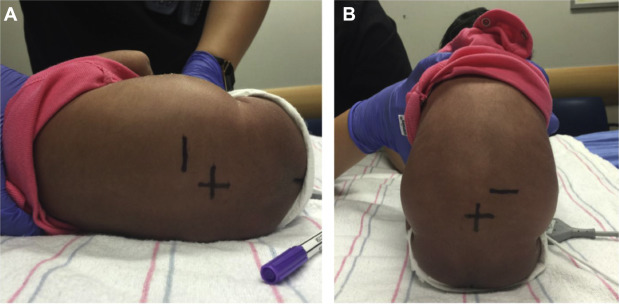
The patient was placed in the lateral decubitus or sitting position (depending on provider preference), with the spine flexed as if planning for lumbar puncture. The termination of the conus medullaris was identified and marked on the skin with a surgical marking pen with a long line perpendicular to the spine. The optimal interspinous level below the conus (widest subarachnoid space) was identified in the longitudinal plane and centered on the screen image, and another short mark was made adjacent to the center of the probe; the probe was then reoriented into the transverse plane at the level of this mark, the spinal canal was centered on the screen, and a short mark was again made at the center of the probe. With the probe removed, these 2 short marks were extended and intersected, making a target cross. The interspace level was confirmed by counting the corresponding vertebral bodies superiorly from the sacrum. The depth from the skin surface to the thecal sac at the marked interspace level was measured and recorded. The research assistant recorded the total time from initial probe placement until skin marking. If abnormal anatomy, such as a low-lying conus, was visualized, the lumbar puncture was aborted. The clinician performing the lumbar puncture was then provided a diagram with the skin markings ( Figure 2 ), as well as the depth and instructions to direct his or her first attempt at the marked interspace. There was no interrater reliability of any measurements performed because the information was provided in real time. Subsequent attempts were allowed by clinician discretion based on the ultrasonography information and clinical judgment. No change in the patient positioning was allowed unless the puncture was unsuccessful on the first attempt.
Three study sonographers performed the ultrasonography (a pediatric emergency medicine board-certified physician and director of the study site emergency ultrasonography program [A.E.C], a senior pediatrics resident [J.T.N.], and a medical student [K.D.]). The director had additional training in emergency and advanced emergency ultrasonography. The trainees completed a beginner ultrasonography technique course and successful identification of anatomic landmarks on at least 5 infant patients. The medical student sonographer had no previous experience with point-of-care ultrasonography but also completed a 2-day ultrasonography course. Each sonographer reviewed the visualization and marking procedure with the principal investigator before the first study ultrasonograph in order to standardize the technique. All images and clips were reviewed with a board-certified pediatric radiologist for feedback and quality control. To our knowledge bedside ultrasonography was not being clinically used at the study site for infant lumbar puncture in the ED.
Methods of Measurement
Baseline demographic and clinical characteristics were collected ( Table 1 ). These characteristics and additional information, including recent antibiotic therapy, history of lumbar puncture (within the previous 72 hours), and spinal cord abnormality (by history), were recorded by a research assistant on a standardized datasheet on the date of enrollment.
| Characteristic | Traditional Arm, n=64 | Ultrasonography-Assisted Arm, n=64 |
|---|---|---|
| Age, days | 29 (14, 45) | 24 (9, 34) |
| Sex, male † | 30 (46.9) | 45 (70.3) |
| Race | ||
| White | 24 (37.5) | 35 (54.7) |
| Black | 26 (40.6) | 16 (25.0) |
| Asian | 5 (7.8) | 1 (1.6) |
| Other | 9 (14.1) | 12 (18.8) |
| Weight, kg | 4.2 (3.3, 4.7) | 3.9 (3.5, 4.4) |
| Gestational age, wk ‡ | 39.0 (37.0, 40.0) | 39.2 (37.7, 40.0) |
| Maximum temperature, °C (°F) | 38.1 (100.6) (37.4, 38.6 [99.3, 101.5]) | 38.2 (100.8) (37.6, 38.8 [99.7, 101.8]) |
| Time LP performed | ||
| Day (8 am to 8 pm ) | 48 (75.0) | 47 (73.4) |
| Night (after 8 pm to before 8 am ) | 16 (25.0) | 17 (26.6) |
| Bolus received | 30 (46.9) | 30 (46.9) |
| First-attempt position † | ||
| Lateral decubitus | 54 (84.4) | 62 (96.9) |
| Sitting | 10 (15.6) | 2 (3.1) |
∗ Values represent median (IQR) and frequency (percentage).
† Statistically significant difference.
In regard to the lumbar puncture procedure, all clinicians who attempted it recorded patient positioning (sitting versus lateral decubitus), provider training level, and self-reported previous lumbar puncture experience (stratified into groups of zero, 1 to 10, 11 to 20, 21 to 50, and >50) for each attempt. It is standard practice at the study institution to use topical lidocaine for all infant lumbar punctures.
A follow-up chart review by the lead research assistant was performed on each patient after hospital discharge. Additional information was recorded, including length of hospitalization, length of receipt of antibiotics, and need for further interventional procedures such as repeated lumbar puncture and sedation. After the final patient was enrolled and data collection was complete, the data were downloaded from REDCap and thoroughly checked for missing variables. Any patients with missing variables had an additional chart review.
To calculate our sample size, we assumed a baseline neonatal lumbar puncture success rate of 60% (based on previous studies demonstrating a failure rate of up to 40%). Using calculations for the comparison of 2 proportions, we estimated a sample size of 128 (64 per group) needed to detect an absolute 20% improvement with a power of 0.8 and α of .05.
Outcome Measures
Our primary outcome was a successful first-attempt lumbar puncture, defined as cerebrospinal fluid obtained with RBC counts less than 1,000/mm 3 because this was the most commonly cited definition of traumatic tap in the literature. An unsuccessful lumbar puncture was also defined as obtaining no cerebrospinal fluid (“dry tap”) or insufficient cerebrospinal fluid for cell counts. Given the diagnostic and treatment ambiguity inherent in both situations (no cerebrospinal fluid or traumatic fluid obtained), we decided to include these together as unsuccessful lumbar punctures. If 2 tubes of cerebrospinal fluid were sent for cell counts, the tube with the fewest RBCs (regardless of order) was used for analysis.
Our secondary outcomes included lumbar puncture success within 3 attempts. The same provider or another clinician could perform additional attempts at the same level as the marking or by provider discretion, keeping in mind the marked level of the conus and the ultrasonography information provided. An attempt was defined as removal and reinsertion of a spinal needle. Redirection of the spinal needle beneath the skin did not constitute an additional attempt. A provider change was not counted as a de novo attempt, but rather as subsequent attempts after the first provider. An additional secondary outcome included lumbar puncture success, defined as RBC count less than 10,000/mm 3 , given the different provider thresholds of a “traumatic tap.”
Primary Data Analysis
Descriptive statistics were used to report baseline and demographic characteristics between the 2 study arms. For purposes of data analysis, we reviewed patient and provider characteristics for the first lumbar puncture attempt only, irrespective of the number of additional attempts, because the rates of traumatic lumbar puncture increase with subsequent attempts. All outcomes were assessed by intention-to-treat analysis.
To assess our primary and main secondary outcomes, we calculated absolute risk differences, risk ratios, and 95% confidence intervals (CIs) where indicated. We investigated for any correlation between sonographer and lumbar puncture success, as well as provider experience (dichotomized to ≤10 lumbar punctures and >10 lumbar punctures) and lumbar puncture success. All analyses were performed with Stata (version 13.0; StataCorp, College Station, TX).
Materials and Methods
Study Design and Setting
We performed a prospective, nonblinded, randomized, controlled trial in an urban academic pediatric emergency department (ED) that has more than 90,000 pediatric patients per year and is staffed with medical students, nurse practitioners, trainees, and attending physicians. Trainees included residents of various specialties (pediatrics, medicine-pediatrics, emergency medicine, family medicine, and psychiatry) and pediatric emergency medicine fellows. There were no specific lumbar puncture training efforts in place, aside from standard hospital credentialing policy for procedures, during the entirety of this study. The institutional review board approved this study.
Selection of Participants
We recruited a convenience sample of infants aged zero to 6 months during a 20-month period from June 2014 to February 2016. Eligible patients were drawn from the study site ED. Inclusion criteria were infants aged 6 months or younger and receiving a lumbar puncture. Research assistants screened patients on the ED tracking board for eligibility. Exclusion criteria included known spinal cord abnormality, such as tethered cord, or parents who were non-English speaking. Sampling of patients was limited to study sonographer availability, given that the study arm was revealed only after randomization. As per institutional protocol, verbal consent for lumbar puncture was obtained by the provider, and written informed consent was subsequently obtained by a study investigator before enrollment.
Interventions
A block randomization sequence was generated with random-sized blocks before the start of the study to ensure that treatment groups were evenly distributed throughout the study duration. The sequence was kept in a password-secured spreadsheet and was not available to the study investigators. Allocation concealment occurred through storage in sealed envelopes containing premarked group assignment and study numbers. During the study period, any medical student, nurse practitioner, trainee, or attending physician was eligible to perform the lumbar puncture; however, to minimize potential bias, the clinician performing the lumbar puncture was identified before randomization. Once the subject was consented and enrolled, the next envelope in line was selected by a research assistant to assign the subject to a treatment arm. For patients randomized to the traditional lumbar puncture arm, no additional intervention was made and clinicians proceeded with lumbar puncture based on the traditional landmark approach. For patients randomized to the ultrasonography-assisted lumbar puncture arm, bedside ultrasonography was performed with a Mindray M7 (Mindray North America, Mahwah, NJ) linear high-frequency transducer before lumbar puncture to identify anatomic landmarks ( Figure 1 ) and to mark the insertion site.









