Figure 5.1. Components of oxygen delivery. CaO2, arterial oxygen content; PaO2, partial pressure of oxygen; SaO2, oxygen saturation; Hgb, hemoglobin.
Endpoints of resuscitation
- Endpoints of resuscitation (EOR) are vital to avoid under or over-resuscitation.
- Identify your endpoints early and assess them often.
- It is best to target multiple endpoints as no single endpoint is superior to the others.
- Pulse and blood pressure (BP) are inaccurate predictors of outcome or fluid responsiveness.
- BP is a product of cardiac output (CO) and systemic vascular resistance (SVR). Patients free of cardiopulmonary disease can compensate for impaired CO and display normal vital signs.
- Identify your endpoints early and assess them often.
- Lactate is a good indicator of hypoperfusion (<2.0 mmol/dL = normal; 2.0–3.9 = mild elevation; >4.0 = severe elevation).
- Lactate elevation may be due to a number of factors including hypoperfusion (i.e., shock), cellular metabolic dysfunction (i.e., toxins affecting either the tricarboxylic acid cycle or the electron transport chain), increased production (i.e., seizures), or decreased clearance (i.e., liver dysfunction).
- Even patients with mild lactate elevation have poorer outcomes.
- Rule of 2s: after 2 hours or 2 L of intravenous fluids (IVF), get a second lactate.
- The half-life of lactate is 15 minutes so it should be checked often.
- Any decrease >10% is good, but normalization is best.
- The half-life of lactate is 15 minutes so it should be checked often.
- Lactate elevation may be due to a number of factors including hypoperfusion (i.e., shock), cellular metabolic dysfunction (i.e., toxins affecting either the tricarboxylic acid cycle or the electron transport chain), increased production (i.e., seizures), or decreased clearance (i.e., liver dysfunction).
- Estimates of preload:
- A perfect predictor of volume responsiveness does not exist.
- Central venous pressure (CVP) is the most widely available endpoint and is most accurate in patients without cardiopulmonary disease.
- A low CVP in a patient with shock is a good indicator of fluid responsiveness.
- When the initial CVP is elevated, however, it does not mean that the patient is adequately fluid resuscitated. It may be that the patient has cardiopulmonary disease and a baseline elevated CVP. Therefore, an alternative EOR should be selected.
- When a patient is intubated, the target CVP is 12–15 mmHg due to increased intrathoracic pressures related to mechanical ventilation.
- A low CVP in a patient with shock is a good indicator of fluid responsiveness.
- A perfect predictor of volume responsiveness does not exist.
- Additional measures can be obtained from noninvasive monitoring devices such as pulse pressure variation (PPV), stroke volume variation (SVV), or thoracic fluid content (TFC).
- These also provide imperfect measures, with reported sensitivities of 80–90%.
- Estimates of afterload:
- In patients presenting with shock, noninvasive blood pressure monitoring can underestimate a patient’s central pressure. An intra-arterial catheter should be placed to minimize the amount of vasopressors administered.
Ongoing assessment of the ICU boarder
- Frequent reassessment of ICU boarders is essential. Since mortality starts to increase at about 6 hours, it is reasonable to completely reassess an ICU boarder every 2–4 hours.
- Assessments should focus on fundamentals of care and disease-specific goals.
- Use the mnemonic: Have MAD LoVE for your ICU boarders.
- Medications often need to be re-dosed during extended ED stays or titrated down (i.e., vasoactive medications).
- Ancillary rounds: round with the nurse(s) and keep them updated on the plan of care.
- Diagnostic reevaluation can prevent misdiagnosis. The “picture” is often clearer once all the data has been obtained and can be assessed in its entirety.
- Laboratory evaluation: oversights in addressing laboratory deficiencies or rechecking abnormalities are extremely common.
- Volume status is a critical component of resuscitation and management. Accurate “Ins and Outs” are frequently poorly recorded in ICU boarders. This can be remedied by asking the nurses to never take down an empty IV bag, and to number each IV bag with a permanent marker prior to administration.
- EOR review: review and/or repeat your EOR to optimize care.
- Medications often need to be re-dosed during extended ED stays or titrated down (i.e., vasoactive medications).
Septic patients
- Many hospitals have a multidisciplinary sepsis team including an ED champion.
- Sepsis order sets help streamline care.
- Completion of the Surviving Sepsis Resuscitation Bundle improves outcomes and reduces resource utilization.
- Sepsis order sets help streamline care.
- The EORs of early goal-directed therapy (indicated for septic patients with a systolic BP <90 mmHg despite 30 mL/kg of IVF, or a lactate >4.0 mmol/dL) are
- CVP goal of 8–12 mmHg (spontaneously breathing patients)
 Preload
Preload
- MAP goal of
 65 mmHg
65 mmHg
- Can add norepinephrine as first-line pressor
 Afterload
Afterload
- Can add norepinephrine as first-line pressor
- CVP goal of 8–12 mmHg (spontaneously breathing patients)
- ScvO2 goal of >70%
- If not, transfuse to achieve a Hct
 30%
30%  Arterial O2 content
Arterial O2 content
- If not, transfuse to achieve a Hct
- If CVP, MAP and Hct are at goal and ScvO2 is still <70%, dobutamine is recommended to augment contractility (the only component of DO2 not optimized) (Figure 5.1).
 Contractility
Contractility
- Aim to complete the above EOR within 6 hours from patient presentation.
Intubated patients
Mechanically ventilated patients in the ED are vulnerable to suboptimal care.
- Auto-PEEP caused by breath stacking and hyperinflation is dangerous (Auto-PEEP = intrinsic PEEP = dynamic hyperinflation).
- It is usually due to bronchospasm resulting in retained air. This in turn causes an increase in intrathoracic pressure leading to decreased CO.
- It also diminishes the efficiency of respiratory muscles, increases the work of breathing, and causes barotrauma and hypotension.
- The goal is to allow for full expiration and to minimize its occurrence.
- Reduce the respiratory rate to 10–12 breaths per minute.
- Set the tidal volume at 6 mL/kg.
- Increase the flow rate.
- Add extrinsic PEEP (50–80% of measured intrinsic PEEP).
- Reduce the respiratory rate to 10–12 breaths per minute.
- It is usually due to bronchospasm resulting in retained air. This in turn causes an increase in intrathoracic pressure leading to decreased CO.
- Patients often require deep sedation and paralysis to tolerate these settings.
- These measures may result in retained CO2 (i.e., permissive hypercapnia; keep PaCO2 <85 mmHg and pH >7.20).
- Proximal airway pressures (PAP) should be regarded as a vital sign in intubated patients and monitored regularly (normal <30 cmH2O).
- Troubleshooting an intubated patient in distress requires an assessment of PAP (Figure 5.2).
- The peak inspiratory pressure (PIP) represents resistance to flow inside the airways. If elevated (with a normal plateau pressure), it suggests bronchospasm or secretions resulting in airway plugging, and should be managed with suction and bronchodilators.
- Plateau airway pressure (Pplat) represents the compliance of the system. If elevated, the underlying cause should be identified and treated.
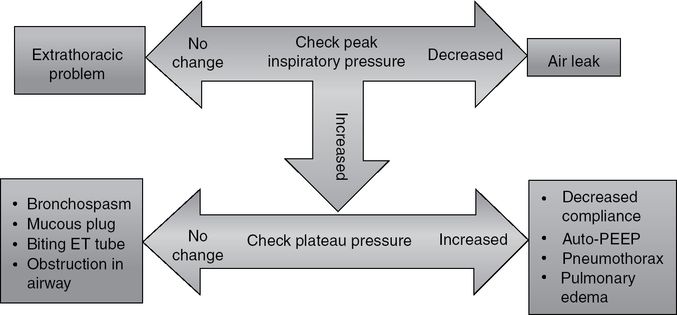
Figure 5.2. Suggested algorithm to assess PAP in troubleshooting a deteriorating intubated patient.
Stay updated, free articles. Join our Telegram channel
- Troubleshooting an intubated patient in distress requires an assessment of PAP (Figure 5.2).

Full access? Get Clinical Tree




