Chapter 111
Telemedicine Applied to the Intensive Care Unit
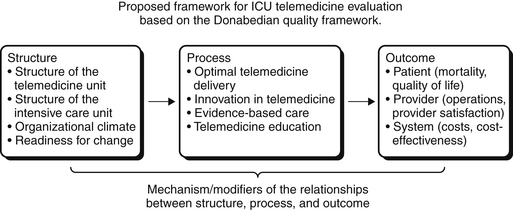
Telemedicine in the intensive care unit (ICU) allows critical care specialists to increase their reach by eliminating geographic constraints. Advances in telecommunications technology, health information systems, and new modalities for analyzing physiologic parameters derived from bedside monitors represent some of the forces that have led to the ICU-telemedicine movement. In many respects, the rapid growth in the practice of ICU telemedicine parallels that of the patient safety movement (Figure 111.1). Critical care is more frequently being delivered by teams of providers rather than by a single individual. As a result, there often exists a variety of opinions and approaches to patient care. Although much of the care is routine and amenable to standardization, not infrequently what is required involves unplanned, urgent action that necessarily is individualized. This combination of routine and emergent tasks performed by changing teams of episodic providers sets the stage for the application of electronic tools designed to identify the need for care, to standardize the delivery of that care, to enable the use of population management tools, achieve high rates of adherence to ICU best practices, to enable rapid and reliable detection of episodes of physiological instability, observe bedside provider responses, and facilitate interventions when those responses are delayed or ineffective.
The application of any new technology inevitably results in novel terminology and concepts. Understanding the definitions of these terms is critically important for both the clinical application of telemedicine tools as well as for allowing useful comparisons among ICUs and the proper interpretation of data. Definitions of ICU-telemedicine can be modeled after Medicare’s definition of tele-health services as recorded in 42 CFR 410.78, keeping in perspective that Medicare does not recognize telemedicine as a distinct billable service. Using this source, telemedicine is defined as the use of medical information exchanged from one site to another via electronic communications to improve a patient’s health. Electronic communication means the use of interactive telecommunications equipment including (but not limited to) audio and video equipment that enables real-time interactive communication between the patient and the clinician at a distant site. Telemedicine is considered an alternative to the traditional way of providing medical care (e.g., face-to-face consultations or examinations between provider and patient). The delivery of ICU telemedicine services when and where they are needed is facilitated by sophisticated notification systems that leverage available patient specific information from laboratory instruments, image interpretation, and physiological monitors. ICU-telemedicine systems vary with regard to the services that they provide and how those services are delivered.
< div class='tao-gold-member'>