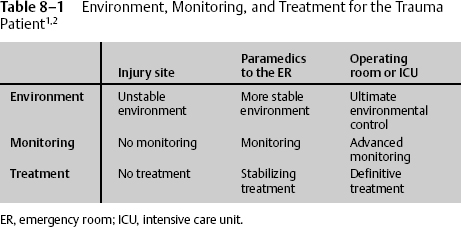
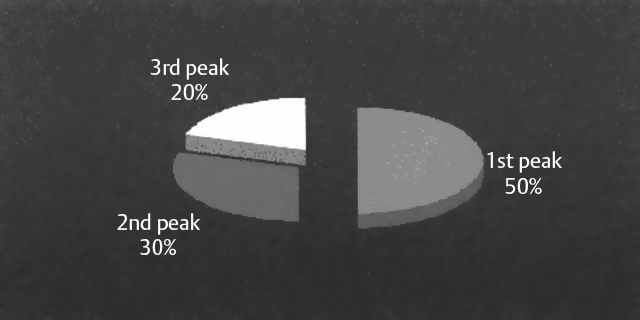
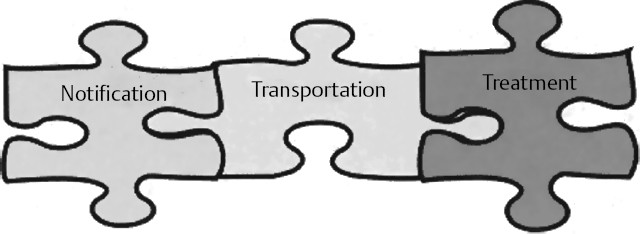
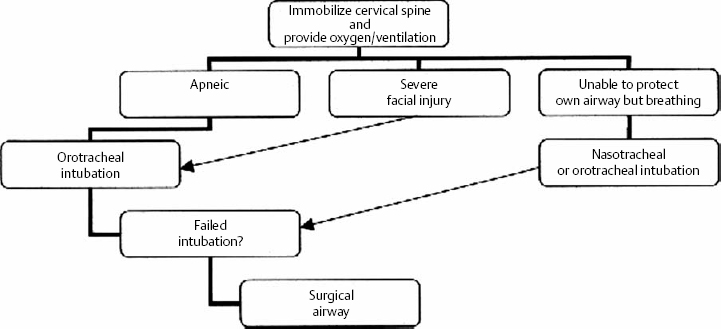
Section II David T. Wong The management of a multisystem-injured patient requires the concerted effort of organized prehospital and hospital care from multiple specialties and is best handled at a designated trauma center. In the United States, there are ~150,000 trauma deaths annually, with ~50% of preventable deaths reducible by well-organized trauma systems (Fig. 8–1). As seen in Fig. 8–1, the first trauma mortality peak (50% of cases) involves catastrophic injury and untreatable injuries; the second and third peaks (30% and 20%, respectively) can be reduced by trauma systems that include prehospital, emergency room, operative, and critical care. Most traumatic injuries are time critical. The “golden hour,” beginning from the time of injury to definitive treatment, refers to the period when a multidiscipline trauma service can have a significant impact on the survival of the patient1 (Fig. 8–2). For example, the shorter the time to operative treatment of intra-abdominal hemorrhage or operative decompression of increased intracranial pressure, the better the chances for survival. Another important concept in trauma care involves improving the environment of the multisystem-injured patient. The patient should be removed from the initial hostile and unpredictable injury site and placed in a more controllable environment. Typically, this initially involves the ambulance or helicopter, then the emergency room (ER), and ultimately the operating room or intensive care unit (ICU). Hostile factors include not only the causes of the injury but also factors such as temperature, noise, and medical resource scarcity. Even the hospital environment can be hostile if the treating physician is not able to control factors like room temperature to prevent hypothermia; noise from poor crowd control that affects communication and movement, especially in the emergency room; and rapid utilization of studies and definitive treatment—for example, decompressive craniotomy. Table 8–1 compares the three main arenas involved in trauma care—care administered at the injury site, care administered by paramedics on the way to the ER, and procedures performed in the operating room or the ICU—in terms of control of the environment, monitoring of the patient, and treatment. Figure 8–1 Trauma mortality peaks. The first trauma mortality peak is due to catastrophic injury and untreatable injuries (50% of cases); the second and third peaks (30% and 20%, respectively, of cases) in trauma mortality can be reduced by trauma systems that include prehospital, emergency room, operative, and critical care. Taking the patient to a safer place typically involves transportation to an environment such as the operating room where environmental and treatment factors are predictable and controllable. Figure 8–2 Time components of the “golden hour.” The primary assessment or the initial advanced trauma life support (ATLS) approach to an acutely injured patient requires the prioritized assessment and treatment of vital systems that is necessary for the support of all vital organs. These systems are defined by the pneumonic ABC: airway, breathing, and circulation. The efficiency of assessment and treatment involves a team of trained professionals: trauma team captain, primary assessor, airway assessor, and trauma nurses. The trauma captain overlooks the flow of the patient’s overall care, and the primary assessor does the majority of the physical examination and treatment. The airway assessor manages the airway and is usually an anesthesiologist or someone trained in airway management. Trauma nurses perform the initial vital sign tests and place monitoring devices; they also start intravenous lines and administer drugs. The loss of airway, which results in inadequate delivery of oxygenated blood to the brain and other vital organs, is one of the earliest causes of death in the injured. Included in this system is the immobilization of the cervical spine. Some of the main reasons for airway protection utilizing endotracheal intubation include decreased mentation (due to shock or brain injury), severe maxillofacial injury, aspiration risk (from bleeding or vomiting), obstruction, and inadequacy of respiratory effort (Fig. 8–3). Hypoxia is a major contributor to brain injury mortality and is still found in 60% of head-injured patients at autopsy.2 Life-threatening injuries such as tension pneumothorax, hemothorax, flailed chest, and misplaced endotracheal intubation, must be identified and treated. Inspection of the neck will help identify direct injury or tracheal deviation secondary to large hemothorax or tension pneumothorax (deviation to contralateral side). Auscultation of the chest bilaterally is important to confirm correct placement of th endotracheal tube as well as identify hemo- or pneumothorax.
Triage
8
Team Management of the Multisystem-Injured Neurosurgical Intensive Care Unit Patient
 Moving the Patient to a “Safer Place”
Moving the Patient to a “Safer Place”
 Prioritizing Care by the Trauma Team
Prioritizing Care by the Trauma Team
Primary Assessment and Treatment
Airway
Breathing
![]()
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree