INTRODUCTION AND EPIDEMIOLOGY
Hypertension affects approximately 30% of the U.S. population, and 1% to 6% of all ED patients will present with severe hypertension.1,2,3,4,5 Of the latter, between a third and one half will have end-organ damage.2,3,4,5 Risk factors for the development of hypertensive crisis include obesity, cigarette smoking, and older age.6
Chronic hypertension is categorized into three classifications: prehypertension, stage 1 hypertension, and stage 2 hypertension7 (Table 57-1).
Hypertensive emergency is an acute elevation of blood pressure (≥180/120 mm Hg) associated with end-organ damage; the targeted end organs include the brain, heart, aorta, kidneys, or eyes7 (Table 57-2). Acute hypertensive emergencies are more common in chronic hypertensive patients who fail to adhere to their antihypertensive therapy regimens and those who are unable to access outpatient health care.6
| Diagnostic Category | Signs and Symptoms | Evidence of Acute End-Organ Damage |
|---|---|---|
| Acute aortic dissection | Chest pain, back pain Unequal blood pressures (>20 mm Hg difference) in upper extremities | Abnormal CT angiogram of chest and abdomen/pelvis or transesophageal echocardiogram of the aorta |
| Acute pulmonary edema | Shortness of breath | Interstitial edema on chest radiograph |
| Acute myocardial infarction | Chest pain, nausea, vomiting, diaphoresis | Changes on ECG or elevated levels of cardiac biomarkers |
| Acute coronary syndrome | Chest pain, nausea, vomiting, diaphoresis | Clinical diagnosis, changes on ECG, or elevated levels of cardiac biomarkers |
| Acute renal failure | May have systolic or diastolic abdominal bruit | Elevated serum creatinine level, proteinuria |
| Severe pre-eclampsia, HELLP syndrome, eclampsia | Seizures | Proteinuria, hemolysis, elevated liver enzyme levels, low platelet counts |
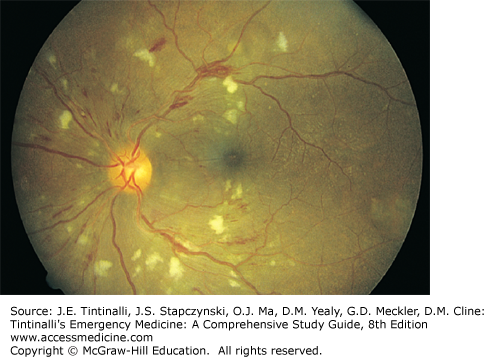
| Hypertensive retinopathy | Blurred vision | Retinal hemorrhages and cotton-wool spots (Figure 57-1), hard exudates, and sausage-shaped veins |
| Hypertensive encephalopathy | Altered mental status, nausea, vomiting, headache | May see papilledema or arteriolar hemorrhage or exudates on funduscopic examination, may note cerebral edema with a predilection for the posterior white matter of the brain on MRI |
| Subarachnoid hemorrhage | Headache, focal neurologic deficits | Abnormal CT of the brain; red blood cells on lumbar puncture |
| Intracranial hemorrhage | Headache, new neurologic deficits | Abnormal CT of the brain |
| Acute ischemic stroke | New neurologic deficits | Abnormal MRI or CT of the brain |
| Acute perioperative hypertension | Bleeding unresponsive to direct pressure | Clinical diagnosis; manifestations of other hypertensive emergencies |
| Sympathetic crisis* | Anxiety, palpitations, tachycardia, diaphoresis | Clinical diagnosis in the setting of sympathomimetic drug use (i.e., cocaine or amphetamines) or pheochromocytoma (24-h urine assay for catecholamines and metanephrine or plasma fractionated metanephrines) |
Hypertensive urgency is a term for profound elevations in blood pressure without acute target organ dysfunction.7 An arbitrary blood pressure of ≥180/120 mm Hg is often cited as an urgency and an indication for rapid pharmacologic intervention (often parenteral) to reduce blood pressure within hours; however, no clear clinical benefit of such treatment exists, and risk can occur from precipitous drops in blood pressure.8,9 Hypertensive urgency is better seen as another form of severe hypertension where prompt therapy with oral agent(s) is the best path, seeking reduction in blood pressure over days to weeks.
PATHOPHYSIOLOGY
At baseline, chronic hypertensive patients have biochemical and structural changes in the arterial walls that shift the vascular autoregulatory curve, requiring higher arterial pressures to maintain end-organ blood flow, notably in the brain.10,11,12 Eventually, the ability to adapt is passed. The resultant mechanical wall stress and endothelial injury lead to increased permeability, and excessive perfusion of the cerebral, cardiac, and renal vascular beds results. This can be followed by activation of the coagulation cascade and platelets, and deposition of fibrin results in fibrinoid necrosis of the arterioles. Clinically, this is manifested by hematuria (involvement of the renal vasculature) or arterial hemorrhages or exudates on funduscopic examination. Further contributing to the damage are prostaglandins, free radicals, cytokines, and mitogenic, chemoattractant, and proliferation factors, which result in endothelial damage, smooth muscle proliferation, and thrombosis.10,12 The renin-angiotensin system may also be activated, which leads to vasoconstriction. Pressure natriuresis occurs, leading to volume depletion, prompting additional release of vasoconstrictors from the kidney. These combined effects produce hypoperfusion, ischemia, and dysfunction of end organs. Endothelial dysfunction from such crises can persist for years after the acute event.13
CLINICAL FEATURES
Measure blood pressure in both arms quickly and consecutively, while the patient is quietly resting. Check blood pressure several times before starting antihypertensive therapy. Blood pressure differences can result from aortic dissection, coarctation, peripheral vascular disease, and some unilateral neurologic and musculoskeletal abnormalities. However, interarm blood pressure differences are also reported in “normal” individuals. The most important factor in blood pressure difference is increasing age, with the thought that loss of vascular elasticity or asymmetrical atheromatous narrowing of subclavian or brachial arteries might be causative. Although there are no guidelines or standards for determining the significance of blood pressure measurement disparities, a between-arm difference >10 to 20 mm Hg is suggested as meaningful,14,15 and each 10-mm Hg difference carries an increasing mortality hazard. When a blood pressure difference is detected, treat the higher blood pressure and make sure that subsequent measurements are made on the same arm.15 Blood pressure measurements with wrist oscillometric devices give lower readings than arm measurements, so arm measurements are preferred.16 Use the same device for repeat blood pressure measurements.
After careful blood pressure measurement, the next question in a patient with severely elevated blood pressure is whether this constitutes a hypertensive crisis. Although a modest drop (4 to 12 mm Hg) in systolic and diastolic blood pressures can be expected in patients presenting with elevated blood pressures,17,18,19 do not discount a diagnosis of hypertensive emergency simply because the patient has no prior history of hypertension. Up to 16% of patients presenting with hypertensive emergency have no known history of hypertension.4 The key is to seek acute end-organ involvement.
Table 57-3 lists the proportion of patients who present with elevated blood pressure by stroke subtypes, aortic dissection subtypes, heart failure, and acute coronary syndrome. Although elevations in blood pressure accompany the majority of these presentations, note that severe elevations of blood pressure are far less common in presentations typically labeled as hypertensive emergencies (Table 57-2).
| Disease | Threshold Value Raising Risk | % of Patients with Elevated Pressures |
|---|---|---|
| Subarachnoid hemorrhage20 | ≥140 mm Hg SBP | 100% |
| Ischemic stroke20,21 | ≥140 mm Hg SBP ≥160 mm Hg SBP | 77%–82% 47%–54% |
| Intracerebral hemorrhage20 | ≥140 mm Hg SBP ≥160 mm Hg SBP | 75% 27% |
| Type B aortic dissection22,23 | ≥140 mm Hg SBP or ≥90 mm Hg DBP | 67%–77% |
| Type A aortic dissection24 | >150 mm Hg SBP | 36%–74% |
| Acute heart failure25 | >140 mm Hg SBP | 54% |
| NSTEMI-ACS25,26 | ≥140 mm Hg SBP ≥160 mm Hg SBP | 57%–59% 31% |
Rapid diagnosis and treatment of acute aortic dissection are critical because delays increase mortality. Differentiating the relatively uncommon aortic dissection from the more common acute coronary syndromes is important because blood pressure management is different in these two disorders, and anticoagulation can prove catastrophic in a patient with acute aortic dissection.27
Acute aortic dissection presents with abrupt, sudden onset of pain, usually in the chest, often described as tearing or ripping, and radiating to the interscapular region23,28 (see chapter 59, “Aortic Dissection and Related Aortic Syndromes”). Less than a quarter of patients with acute aortic dissection have a neurologic deficit or pulse deficits based on blood pressure differentials ≥20 mm Hg, and only about a third have a diastolic murmur. Chest radiograph is abnormal in most but usually nonspecific, and only 25% of radiographs demonstrate the classic widened mediastinum,24 so CT of the chest is needed for the diagnosis. ECG changes are nonspecific, but <10% demonstrate findings consistent with a myocardial infarction.24 D-Dimer testing cannot be used in isolation to exclude the diagnosis, but elevated D-dimer and C-reactive protein levels are associated with higher in-hospital mortality.29,30
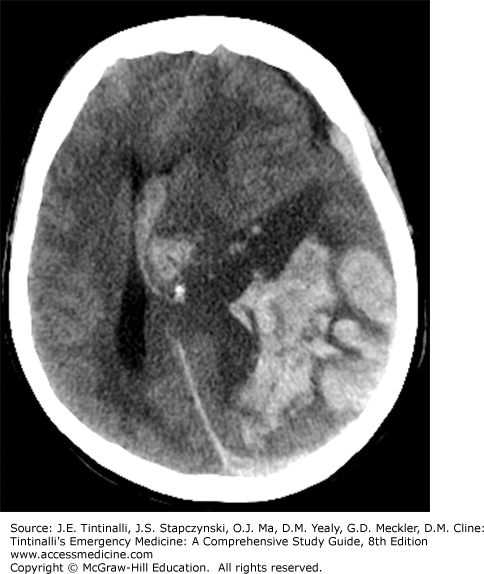
Elevated blood pressure, headache, and focal neurologic deficits are associated with either ischemic or hemorrhagic strokes. Acute ischemic strokes may be diagnosed with MRI, and cerebral hemorrhage is identified on head CT (see chapter 167, “Stroke Syndromes”) (Figure 57-2).
Hypertensive encephalopathy is a clinical diagnosis after excluding focal ischemia or bleeding. It is characterized by altered mental status, headache, vomiting, seizures, or visual disturbances, and most patients will have papilledema. When MRI findings demonstrate reversible edema that is primarily focused posteriorly (occipital vs frontal regions), this is referred to as posterior reversible encephalopathy syndrome (Figure 57-3).
FIGURE 57-3.
Axial fluid-attenuated inversion recovery MRI showing white matter hyperintensity in the occipital lobes bilaterally consistent with posterior reversible encephalopathy syndrome. The patient’s confusion improved with blood pressure control. Repeat MRI after several days of therapy demonstrated remarkable improvement. [Image used with permission of Michael Farner, MD.]
Patients with new-onset renal failure may have peripheral edema, oliguria, loss of appetite, nausea and vomiting, orthostatic changes, or confusion. However, some patients have few or no specific symptoms (see chapter 88, “Acute Kidney Injury”). Elevated serum creatinine confirms the diagnosis, and urinary sediment is also abnormal.
Pre-eclampsia is associated with hypertension, peripheral edema, and proteinuria. These patients may also develop hemolysis, elevated liver enzyme levels, and low platelet counts (HELLP syndrome) (see chapter 100, “Maternal Emergencies after 20 Weeks of Pregnancy and in the Postpartum Period”).
There are four settings in which an excess of catecholamines can result in a hypertensive emergency. An acute catecholaminergic syndrome may occur with abrupt discontinuation of oral or transdermal clonidine. The withdrawal syndrome is potentiated by concomitant β-blocker therapy due to unopposed α-mediated vasoconstriction.
Pheochromocytoma is rare, and between 5% and 20% of tumors are malignant. Patients may experience life-threatening hypertension.31 Signs of pheochromocytoma include headache, alternating periods of normal and elevated blood pressure, tachycardia, and flushed skin, punctuated by asymptomatic periods.
Sympathomimetic drugs such as cocaine, amphetamines, phencyclidine hydrochloride (PCP), and lysergic acid diethylamide (LSD), can precipitate a hypertensive emergency, with tachycardia, diaphoresis, chest pain, and, depending on the agent, mental status changes.32 Patients receiving monoamine oxidase inhibitor therapy who consume tyramine-containing foods may develop a hyperadrenergic state.33 Autonomic dysfunction due to spinal cord or severe head injury or abnormalities such as spina bifida may also present as a hypertensive emergency, with the diagnosis made clinically based on the existing injury.
Formal recommendations for the evaluation of an ED patient presenting with asymptomatic but severe hypertension do not exist.9 Commonly ordered tests include basic metabolic panel (73%), ECG (53%), chest radiograph (46%), and urinalysis (43%).3 In a prospective study of over 100 ED patients with asymptomatic severe hypertension, clinically meaningful results existed in only 6% of patients, with only 5% of patients thought to have abnormal results attributable to acute hypertensive target organ injury.34 Until more data are available, base ED evaluation on the patient complaint, history, and review of systems, and perform selected testing.
TREATMENT
Table 57-4 lists agents for the management of hypertensive emergencies categorized by diagnosis. Hypertensive emergencies in pregnancy are discussed in chapter 100. In selecting therapy, be familiar with the use of the selected agent, and establish a target range for blood pressure reduction. The goal is to minimize end-organ damage by initial blood pressure reduction while avoiding hypoperfusion of cerebral, coronary, and renovascular beds. Acute aortic dissection is the exception, because the risk of morbidity and mortality due to inadequate blood pressure and heart rate control outweighs the risk of hypoperfusion syndromes.
| Diagnosis | Therapy Goals | Agents | Risks | Comments |
|---|---|---|---|---|
| Aortic dissection | Reduce shear forces by ↓ BP and PR; lower SBP to 100–120 mm Hg35,36,37; or lower SBP to <140 mm Hg23; ↓ PR <60 beats/min | Measure BP in both arms and treat higher BP | ||
| Labetalol35,36,37 IV continuous infusion or esmolol35,36,37 IV bolus, then continuous infusion | Respiratory distress in COPD, asthma patients; test dose of esmolol recommended, switch to diltiazem if esmolol intolerant36 | |||
| Nicardipine38 IV continuous infusion (after β-blocker) | Always use β-blocker prior to vasodilators | |||
| Nitroprusside36,37 continuous infusion (after β-blocker) | Always use β-blocker prior to vasodilators; nitroprusside alone increases wall stress from reflex tachycardia; cyanide and thiocyanate toxicity in patients with reduced renal function or therapy >24–48 h | |||
| Acute hypertensive pulmonary edema | Reduce BP by 20%–30%; diuresis through vasodilation; symptomatic relief | |||
| Nitroglycerin SL, topical, or IV continuous infusion39,40 | IV nitrates dilate capacitance vessels at low doses; higher doses dilate arterioles and lower BP | |||
| Enalaprilat IV40 | ACE inhibitor, can worsen renal function | Avoid hypotension | ||
| Nicardipine IV continuous infusion | Use with caution; some patients experience a negative inotropic effect | |||
| Nitroprusside IV continuous infusion39,40 | Cyanide and thiocyanate toxicity in patients with reduced renal function or therapy >24–48 h | |||
| Nesiritide IV39,40 | Mixed outcomes (favorable and unfavorable) with nesiritide, with most recent ASCEND-HF trial showing no difference in dyspnea and mortality when compared to placebo41 | Nesiritide lowers PCWP more than nitroglycerin39 | ||
| Acute myocardial infarction | Reduce ischemia; avoid ≤25% reduction of MAP42 | BP >180/110 mm Hg is a relative contraindication for thrombolytics43,44 | ||
| Nitroglycerin SL, topical, or IV continuous infusion42,43,44 | Do not give nitrates in patients who have taken phosphodiesterase inhibitors for erectile dysfunction ≤24 h (48 h for tadalafil)43 | |||
| Metoprolol or labetalol IV bolus42,43,44 | Do not give β-blockers in CHF, low-output states, or other contraindications to β-blockers | Monitor for hypotension; consider RV infarct and volume depletion | ||
| Acute sympathetic crisis (cocaine, amphetamines, MAOI toxicity) | Reduce excessive sympathetic drive and symptomatic relief | Labetalol is controversial; if given, administer along with a nitrate42 | ||
| Benzodiazepine32,45 IV bolus | Benzodiazepines are first-line agents; observe for respiratory depression | |||
| Nitroglycerin SL, topical, or IV continuous infusion42,45 | ||||
| Phentolamine45 IV or IM | ||||
| Nicardipine IV continuous infusion42,45 | ||||
| Acute renal failure | Reduce BP by no more than 20% acutely11 | Do not give nitroprusside, as it results in cyanide and thiocyanate toxicity; avoid ACE inhibitor acutely (some authors contradict this caution)11 | ||
| Nicardipine46 IV continuous infusion | ||||
| Clevidipine IV continuous infusion | ||||
| Fenoldopam46 IV continuous infusion | ||||
| Hypertensive encephalopathy | Decrease MAP 20%–25% in the first hour of presentation47; more aggressive lowering may lead to ischemic infarction | Autoregulation of cerebral perfusion may be significantly impaired, so avoid rapid BP lowering; do not give nitroglycerin48 as it may worsen cerebral autoregulation | ||
| Nicardipine49 IV continuous infusion | ||||
| Labetalol50 IV continuous infusion | Avoid in sympathetic crisis from drugs | |||
| Fenoldopam50 IV continuous infusion | ||||
| Clevidipine IV continuous infusion51 | ||||
| Subarachnoid hemorrhage | SBP <160 mm Hg to prevent rebleeding52; avoid hypotension to preserve cerebral perfusion; BP parameters have not yet been defined52 | Nimodipine is used to decrease mortality. BP control is not its primary goal, but some decrease in BP may be seen.52 Clazosentan is used with success in lieu of nimodipine and has similar hypotensive effects.53 | ||
| Nicardipine54,55,56 IV continuous infusion | ||||
| Labetalol52,56 IV bolus, 10–20 milligrams IV, or continuous infusion | ||||
| Esmolol IV bolus, then continuous infusion | ||||
| Clevidipine52 IV continuous infusion | ||||
| Intracerebral hemorrhage | If SBP >200 or MAP >150 mm Hg, consider aggressive management, IV infusion.57 If SBP >180 or MAP >130 mm Hg and possibly elevated ICP*, use infusions or IV boluses while maintaining CPP ≥60 mm Hg.57 If SBP >180 or MAP >130 mm Hg and no elevated ICP, goal MAP is 110 mm Hg (160/90 mm Hg).57 | Drops in SBP <150 mm Hg are not associated with increased morbidity.58 Early hemorrhage growth often occurs in first 6 h. Recent data suggest that during this time, aggressive BP control (SBP 120–160 mm Hg) diminishes hematoma growth, morbidity, and mortality.58,59,60 | ||
| Labetalol56,61 IV bolus or continuous infusion | ||||
| Nicardipine56,61,62,63 IV continuous infusion | ||||
| Esmolol64 IV bolus, then continuous infusion | ||||
| Acute ischemic stroke, rtPA candidate (BP ≤185/110 mm Hg) | If fibrinolytic therapy planned, treat if BP remains >185/110 mm Hg after 3 measurements65; SBP goal is between 141 and 150 mm Hg66 | Excess BP Lowering may worsen ischemia | Elevated BP spontaneously decreases within 90 min after onset of acute stroke symptoms | |
| Labetalol65 10–20 milligrams IV bolus; may repeat one time | ||||
| Nicardipine65 IV continuous infusion 5 milligrams/h, titrate up by 2.5 milligrams/h every 5–15 min; maximum 15 milligrams/h; adjust when desired BP is reached | ||||
| Nitroprusside65 may be used if BP is not controlled with above agents or DBP >140 mm Hg | ||||
| Acute ischemic stroke, hypertension excludes rtPA (BP >185/110 mm Hg) | Treat if >220/120 mm Hg on third of 3 measurements, spaced 15 min apart65 | Do not lower SBP by >10%–15% in first 24 h.65 BP that is lower during the acute ischemic stroke than the premorbid pressure could be considered hypotension. Be careful with BP control efforts in patients taking oral β-blockers or clonidine; antihypertensive withdrawal syndrome may occur. | ||