Fig. 26.1
Coronal SSFP image showing facial nerve anatomy: root exit point (RExP), attached segment (AS), root detachment point (RDP), transition zone (TZ), and cisternal portion (CP)
Imaging in HFS
Imaging of patients with HFS who are considered for MVD is intended to delineate the facial nerve and adjacent vessels. Studies should include thin-section multiplanar steady-state free precession (SSFP) MRI sequences, which are heavily T2 weighted and provide excellent contrast between CSF and adjacent tissue [25]. The role of SSFP imaging in the evaluation of vascular compression syndromes has been described [26–29] and recently optimized for HFS by our group [22, 23]. Studies are performed on either 1.5 or 3 T MRI scanners (Optima and Discovery; GE Healthcare, Milwaukee, WI) and include whole-brain sagittal T1, axial fluid-attenuated inversion recovery (FLAIR) , and diffusion weighted imaging (DWI) sequences. Thin-section axial, coronal, and sagittal SSFP images through the brainstem are obtained. It is important to note that the role of imaging in HFS is supportive and not diagnostic. As reported by our group, imaging has a sensitivity of 75–92.9 % and a specificity of 28.6–75 % [30]. The high sensitivity warrants appropriate counseling in patients deemed clinically favorable for surgery but have no vascular compression on thin-slice T2-weighted MRI . Furthermore, the low specificity does not warrant justification of surgery for positive imaging findings in clinically unfavorable surgical candidates.
Operative Technique of Microvascular Decompression of the Facial Nerve
Medications have been shown to be largely ineffective in treatment of HFS [31–34]. Serial botulinum toxin injections of the facial musculature may provide a temporary respite but are not curative. In addition, prolonged use of botulinum toxin may result in persistent facial nerve paresis or palsy. For this reason, MVD, the only etiological therapy for HFS, is the preferred treatment [33, 35].
Microvascular decompression is performed under general anesthesia with the patient in the contralateral decubitus position (Fig. 26.2, utilizing auditory brainstem-evoked potentials [ABRs]), facial EMG, and monitoring of the AMR in a previously described manner [35]. A retromastoid incision is made behind the hairline, and a small craniectomy below the asterion is performed. The edge of the sigmoid sinus is identified, and the dura mater is opened. After appropriate brain relaxation is achieved with cerebrospinal fluid (CSF) drainage, the facial nerve is exposed from the root exit point to the transition zone and examined for vascular contact. In concert with our neuromonitoring team, arteries are decompressed from the facial nerve using shredded Teflon® implants. Occasionally, our surgeon (RS) transposes or “slings” the artery away from the facial nerve. ABRs and facial EMG are used to monitor the patients in all cases. Direct monopolar facial nerve stimulation is used in selected cases (Videos 26.1 and 26.2).
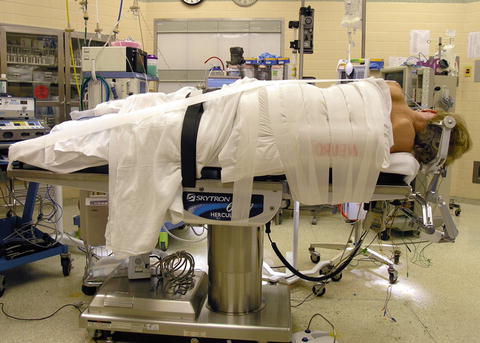
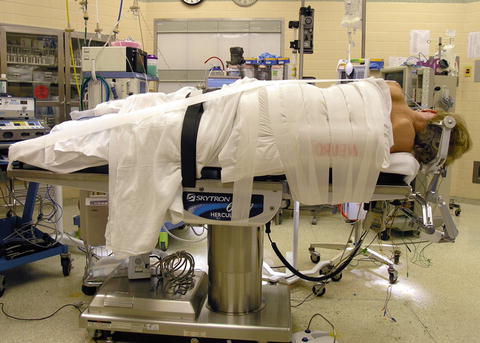
Fig. 26.2
Photograph of patient in the lateral decubitus position. Patient’s head is placed at the foot of the operating table to allow more leg room for the surgeon during the microsurgical portion of the procedure. The head is secured with three-point fixation and the patient is turned in the lateral decubitus position. The head is rotated slightly away from the affected side and flexed to allow approximately two fingerbreadths from the sternum
Anesthetic Considerations During MVD for HFS
Induction of general anesthesia may begin with propofol or etomidate. A depolarizing muscle relaxant is often used for the intubation. It has been our experience that even a small defasciculating dose of nondepolarizing muscle relaxant used during the intubation period is enough to obscure the detection of the AMR at the beginning of the case. Maintenance of general anesthesia can be achieved with a variety of techniques as long as the patient remains motionless without the use of muscle relaxants. Some patients may require only an inhalational agent while others may require inhalation as well as an infusion of either propofol or narcotic such as remifentanil. Meticulous attention to proper positioning takes into consideration avoidance of extreme head and neck flexion or rotation, proper placement of an axillary roll, as well as proper padding of both upper and lower extremities to prevent peripheral nerve injury. There should always be a final confirmation of bilateral breath sounds to confirm the absence of endotracheal tube migration.
Principles of Intraoperative Neuromonitoring for HFS
The AMR can be elicited in nearly every patient with HFS. Nondepolarizing muscle relaxants can obscure results. Bipolar subdermal needle recording electrodes are placed in the orbicularis oculi and mentalis muscles. Paired electrodes are placed approximately 0.5–1 cm apart. Bipolar stimulating electrodes were inserted subdermally over the zygomatic branch of the facial nerve midway between the outer canthus and tragus. Monophasic pulses were delivered at an intensity of 1–20 mA, a frequency of 4.0 Hz, and a pulse width of 0.2 ms. Final positioning of the stimulating electrodes is based on the location that maximizes the orbicularis oculi response and the AMR recorded from the mentalis muscle group. Once identified, suprathreshold stimulation intensity is utilized throughout the procedure. Electrodes are then affixed to the skin in their optimal position with tape.
To avoid nerve fatigue, the AMR is evoked at approximately 5-min intervals until dural opening. Once the dura is opened, the AMR should be recorded continuously throughout the dissection and decompression and then again periodically during closure to detect the potential reappearance of the AMR. Occasionally, the AMR disappears as CSF is drained, ostensibly as a result of relaxation of vascular compression of the facial nerve. Of note, our group has not used brain retraction in the past 5 years [36]. An attempt is made to restore the AMR by increasing the current intensity (up to 20 mA), increasing the stimulation frequency, and finally by increasing pulse widths in increments of 50 μs. After decompression of suspected arteries and veins from the facial nerve and disappearance of the AMR, a further attempt is made to “drive” or stimulate the AMR by increasing the frequency to 30 Hz. If the AMR cannot be elicited, we consider the AMR to have completely resolved.
Monitoring for Complications
Cranial nerve injuries during MVD may result in facial weakness, hearing impairment, vestibular dysfunction, and dysphagia and/or hoarseness, which can affect satisfaction with MVD despite the absence of HFS postoperatively. ABRs are used to monitor cochlear nerve function throughout the procedure. In addition, continuous monitoring of the AMR (Fig. 26.3) and occasional monopolar facial EMG are performed during the procedure. Indeed, neuromonitoring in MVD surgery has been shown not only to improve patient outcome in terms of symptom resolution, but also to decrease the occurrence of hearing loss and facial nerve weakness after surgery [37–39]. Monitoring of somatosensory evoked potentials (SSEPs) used to detect brainstem stroke secondary to vascular manipulation may be considered but is not routinely performed by our group. Monitoring of the ninth and tenth cranial nerves is not performed.
Fig. 26.3
Tracings of the AMR showing changes during MVD for HFS
In the following examples, we review cases from our experience over the past 30+ years of MVD for HFS.
Case Illustrations
Case 1: Understanding the AMR During MVD of the Facial Nerve
A 42-year-old woman with right-sided HFS underwent an MVD after serial botulinum toxin injections resulted in unsatisfactory results. During the operation, the AICA and PICA were noted to be tightly compressing the right facial nerve. During decompression of the PICA, the AMR resolved and could not be elicited (Fig. 26.4). The patient awoke from the operation with much reduced spasms, which gradually decreased and resolved entirely 4 months after the operation.
Fig. 26.4
Disappearance of the AMR with successful microvascular decompression of the facial nerve (Y-axis represents time in seconds following MVD of facial nerve). The compound action potential is being recorded at the mentalis muscle while the facial nerve branch to the orbicularis oculi is stimulated
Team notes: Even after appropriate decompression of the facial nerve, as many as half of the patients have persistent spasms, which resolve over the course of a few weeks to 23 months [35]. Since the AMR often disappears when the offending vessel is lifted off of the facial nerve in a microvascular decompression procedure, its use has been suggested as an intraoperative guide to success [18, 40–43]. Because HFS disappears or gradually resolves over time in many patients in whom the AMR persists intraoperatively, many authors have questioned the utility of intraoperative EMG [44–47]. In a large study evaluating 300 patients, Kong et al. [43] found a statistical difference at 1-year follow-up in the outcomes between two groups based on whether the AMR resolved or persisted [43]. Their report is the only one to show a statistically different outcome in cases where the AMR did not resolve. A meta-analysis by Sekula et al. [35] of the data concerning the relationship between resolution or persistence of the AMR after MVD and the resolution or persistence of HFS showed that the chance of a cure if the AMR was abolished after MVD was 4.2 times greater than when the AMR persisted. Thirumala et al. [48], reporting on 259 patients undergoing MVD with intraoperative monitoring of the lateral spread response (LSR), found that abolishment of the LSR during surgery was associated with statistically significant rates of spasm relief immediately postoperatively and at discharge. This increased rate of spasm relief was not observed at later follow-up between the two groups [48]. Furthermore, reoperation for persistent symptoms and botulinum toxin treatments prior to surgery does not affect rates of intraoperative abolishment of the LSR [49, 50]. Based on these results, we support that AMR should be monitored routinely in the operating room, and surgical decision-making in the operating room should be guided by the absence or presence of the AMR.
Case 2: “Frozen Shoulder” or Adhesive Capsulitis of the Glenohumeral Joint after MVD in the Contralateral Decubitus Position
A 52-year-old woman with right-sided HFS underwent an MVD after serial botulinum toxin injections resulted in unsatisfactory results. During the operation, the PICA was noted to be tightly compressing the right facial nerve. During decompression of the PICA, the AMR resolved and could not be elicited. No change in SSEPs was noted. The patient awoke without spasms but complained of pain, stiffness, and limited range of movement of her left shoulder.
The surgeon recommended observation and increasing use of the left shoulder for the first 6 weeks following the operation. During those 6 weeks, the patient’s shoulder pain increased to the point that she did not use the left shoulder and upper extremity and required assistance with dressing. The surgeon referred the patient for physical therapy, which was ineffective. The patient was then referred to an orthopedic surgeon who diagnosed her with a “frozen shoulder ” or adhesive capsulitis of the glenohumeral joint. MRI of the left shoulder confirmed adhesive capsulitis. The surgeon performed “manipulation” of the left shoulder under a general anesthetic in the operating room, and the patient awoke with reduced pain and improved range of motion. Over the next few weeks, the pain resolved entirely and range of motion was restored.
Team notes: The pathophysiology of adhesive capsulitis is elusive. Although this complication is rare with the contralateral decubitus position, it should be considered in the differential diagnosis of those patients complaining of pain and reduced range of motion of either shoulder. Additionally, extreme care should be taken when retracting the nondependent shoulder inferiorly due to the potential for stretching of the brachial plexus. This is true when shoulders are taped and pulled away from the operative field (see Fig. 26.2) whether in the supine (such as in an anterior cervical discectomy and fusion), prone (such as in a suboccipital decompression), or in lateral position, as in this case, a retromastoid approach for microvascular decompression .
Case 3: Inability to Access Brainstem Due to Intravenous Fluid Overload
A 35-year-old man with right-sided HFS was taken to the operating room for an MVD . After a retromastoid craniectomy was achieved, the dura was opened. The surgeon noted that the brain immediately “herniated through the dural opening.” After a dose of mannitol and 20 min of head elevation, the brain relaxed to the point that the dura could be closed. MVD was aborted, and the operation was rescheduled.
Team notes: Accessing the brainstem and cranial nerves requires communication between the surgeon and the anesthesia providers. Particularly in younger patients, the brain can be “full,” making the brainstem difficult to access. When possible, intravenous fluids should be limited prior to dural opening. In general, most patients receive a total of about 1 L of crystalloid or less for the entire perioperative period.
Case 4: Technical Difficulties with the Inserted Earpiece for Acquiring ABRs
A 57-year-old woman with left-sided HFS underwent an MVD after serial botulinum toxin injections resulted in unsatisfactory results. During drilling of the retromastoid craniectomy, the neuromonitoring technician became concerned because of reduced amplitude and prolonged latency of the left ABR . After confirmation that the patient was hemodynamically stable, the neuromonitoring technician checked the left earpiece and noted that the earpiece had become dislodged. The earpiece was adjusted and the ABR returned to baseline.
Team notes: Kinking of the ear insert tubing occurs infrequently and can be minimized by making sure the tubing is run away from the operative field. When the ABRs change without good reason, the insert and tubing should always be checked for proper delivery of the click stimulus (Fig. 26.5).
Fig. 26.5
Tracings of the ABRs depict dislodged insert earpiece
Case 5: Hearing Loss as a Result of MVD for HFS
A 67-year-old woman with right-sided HFS underwent an MVD after serial botulinum toxin injections resulted in permanent facial weakness (House-Brackmann grade II/VI) [51]. After dural opening, a brain retractor was used to elevate the cerebellum away from the brainstem for exposure of the facial nerve. During this maneuver, the neuromonitoring technician advised the surgeon that waves III and V of the right ABRs had increased in latency by 0.8 ms. Within a few minutes, the neuromonitoring technician advised that the amplitude of the ABRs had decreased by 50 %.
After notification of a reduction in amplitude of the ABRs, the surgeon removed the retractor and stopped dissection. The anesthesiologist increased the mean arterial blood pressure 10 mmHg to a MAP of 80 mmHg. Within 2 min, the latency improved and the amplitude increased. Within 5 min, the ABRs had returned to baseline, and the surgeon resumed exposure of the facial nerve.
Team notes: Hearing loss remains a significant risk with MVD of the facial nerve for HFS, with partial hearing loss ranging from 0.5 to 9.5 % and complete hearing loss ranging from 0.7 to 7.6 % [2, 33, 52, 53]. Polo et al. [53] have provided data concerning a stepwise reduction in hearing with progressive latency increases of Peak V of the ABR during microvascular decompression. In their study of 84 consecutive patients undergoing MVD for HFS, they report that in the group with more than a 20-dB loss in pure tone audiogram, delays in the latency of Peak V were on average 1 ms. To this end, a recent study by our group showed that intraoperative loss of wave V resulted in significantly increased odds of hearing loss [38]. Recently, our group attempted to address this with avoidance of a fixed, self-retained cerebellar retractor in favor of dynamic retraction and subsequently demonstrated a reduction in ipsilateral high-frequency hearing loss (HFHL) from 50 to 7.4 % [36].
Case 6: Anesthesia and the AMR
A 54-year-old woman with a 10-year history of right-sided HFS is brought to the operating room for MVD of the facial nerve. After positioning the patient in the contralateral decubitus position, the neuromonitoring technician reports an inability to obtain an AMR of the right facial nerve.
After confirming that the AMR was documented in the Cranial Nerve and Brainstem Disorders Clinic, discussion among the team revealed that a nondepolarizing muscle relaxant had been given during induction for intubation. The team waited 30 min before beginning the procedure, allowing the agent to wear off.
Team notes: Although the evidence is anecdotal, we believe that there is no role for the use of nondepolarizing muscle relaxants in cases involving microvascular decompression for HFS. It has been our experience that a small defasciculating dose of a nondepolarizing muscle relaxant used during the intubation period is enough to obscure the detection of the abnormal spread at the start of the case. The return of the AMR after the use of a nondepolarizing agent becomes unpredictable.
Case 7: Stroke During MVD for HFS
A 35-year-old woman with right-sided HFS underwent MVD of the right facial nerve. After exposing the facial nerve, the anterior inferior cerebellar arteries as well as multiple perforators of that vessel were noted to be tightly compressing the facial nerve. A preoperative MRI had revealed right-sided dolichoectasia of the vertebrobasilar system with clear compression of the right facial nerve. During the operation, the AICA with perforators and the vertebral artery were decompressed without incident. The AMR was abolished. SSEPs were not measured during the procedure.
Upon awakening, the patient was free of spasms, but, within an hour, she noted contralateral trunk and extremity hypalgesia and thermoanesthesia, ipsilateral Horner syndrome, ipsilateral hypohidrosis, and gait ataxia consistent with a Wallenberg syndrome [54, 55]. Stroke involving the PICA, vertebral artery, or their respective perforators was suspected [56], and a postoperative MRI of the brain confirmed a small infarct involving the lower lateral medulla and posterior cervical spinal cord. Because intraoperative videos did not indicate an avulsion of a perforator or major vessel during decompression of the vertebral and posterior inferior cerebellar arteries (including a complicated tangle of arterioles compressing the facial nerve likely representing PICA medullary perforators), occult compression or vasospasm of perforators was suspected. Although some authors have suggested the use of papaverine to prevent vasospasm-related ischemia [44], we do not routinely use papaverine during MVD due to concerns of vestibulocochlear toxicity [57]. The patient was discharged from acute rehabilitation on postoperative day 13 with improved and independent ambulation. At 10.3-month follow-up, ipsilateral hypohidrosis and gait ataxia had improved significantly with moderate improvement of contralateral extremity thermoanesthesia. The patient notes some incoordination with jogging and persistent difficulty with high humidity due to hypohidrosis.
Team notes: Because of the low incidence of stroke with MVD of the facial nerve (i.e., <0.2 %), we have not utilized SSEPs for MVD for any cranial neuralgia in recent years. It is likely, however, that a change in the SSEPs would be noted, at least in a delayed fashion, in the event of an ischemic event involving the brainstem. If so, application of papaverine to the affected blood arterial vessels (see above explanation), repositioning of Teflon pledgets, and increasing the mean arterial blood pressure (particularly with hypertonic saline) may have been valuable in this patient.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree








