CHAPTER 64
Suprascapular Nerve Block
INTRODUCTION
The suprascapular nerve is a branch off the brachial plexus that arises from the C5-C6 nerve roots. It has afferent, efferent, and sympathetic fibers. Seventy percent of the afferent input travels via the suprascapular nerve; specifically, it provides sensory input from the scapula, acromioclavicular joint, and posterior and superior shoulder joint. Its efferent component innervates the supraspinatus and infraspinatus muscles.
The suprascapular block was first described by Wertheim and Rovenstein in 1941 for the use of intractable shoulder pain. This initial technique was essentially “blind” in that it was solely based on landmarks and clinical information without additional modalities that may be used today such as a nerve stimulator, fluoroscopy, or ultrasound. Wertheim and Rovenstein relied on the patient’s perception of paresthesias as the marker that their needle was correctly placed in the suprascapular notch where the nerve exits. Studies have demonstrated significant benefits of the suprascapular nerve block such as pain relief and improved range of motion. With shoulder pain affecting approximately 15% to 30% of adults, the relative ease of this block along with its minimal risks emphasizes the importance of its use in clinical practice.
INDICATIONS FOR SUPRASCAPULAR BLOCK
• Shoulder pain from inflammatory diseases: rheumatoid arthritis, seronegative spondyloarthropathies, crystal arthropathies
• Postoperative pain after shoulder surgery (arthroscopy, acromioplasty)
• Adhesive capsulitis/rotator cuff disease
• Intractable pain from trauma (ie, fracture)
• Bursitis
• Acute anterior shoulder dislocation
• Diagnostic block for suprascapular nerve entrapment
RELEVANT ANATOMY
• The suprascapular nerve is arises from the C5 and C6 nerve roots of the brachial plexus.
• In 50% of instances, the nerve will also arise from the C4 nerve root.
• It runs lateral, posterior, and inferior deep to the posterior belly of the omohyoid muscle and anterior to the trapezius muscles to reach the superior border of the scapula to the superior scapular notch.
• It then runs inferior to the transverse scapular ligament and passes under the supraspinatus muscle through the floor of the supraspinous fossa, around the lateral border of the scapular spine and into the infraspinaous fossa to innervate the infraspinatus muscle.
The suprascapular nerve gives off several branches including:
• Motor nerves to the supraspinatus and infraspinatus muscle
• Sensory nerve branches to the coracoclavicular, coracohumeral ligaments, acromioclavicular joint, glenohumeral joint, and the subacromial bursa
The supraspinous fossa is an important structure to delineate as it is used for the blockade of the suprascapular nerve in several techniques. It is bounded by the following structures:
• Spine of the scapula
• Plate of the scapula
• Supraspinous fascia
Suprascapular Notch
• The suprascapular nerve is the only neural structure that exits through the supraspinous fossa via the suprascapular notch which also serves as point of injection for this nerve block.
• The anatomic variation of this notch can explain the incidence of suprascapular nerve injury as well as any difficulty in placement of this block.
• In one cadaveric study, the suprascapular notch was found to be deeper in men than in women with the average for males being 8.22 mm and for women 8.06 mm.
The suprascapular notch (Figure 64-1) can be described into 5 types.
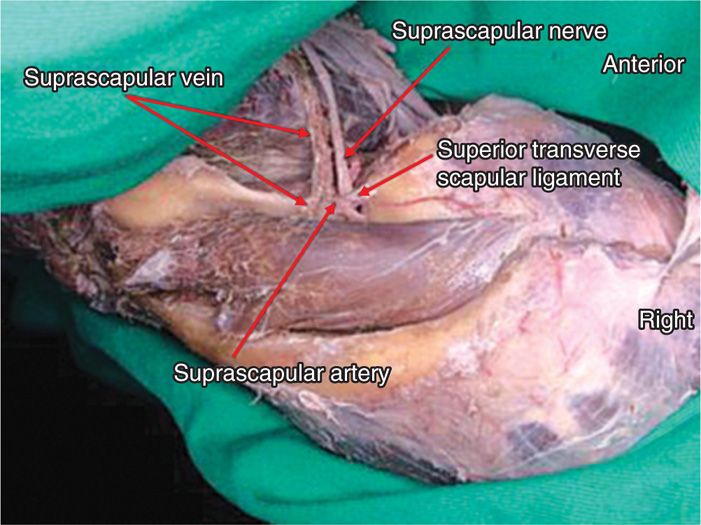
Figure 64-1. View of the suprascapular nerve in relation to the muscle attachments and suprascapular vasculature.
• Type 1: Lacks a distinct notch.
• Type 2: Notch is greater in transverse length than vertical length.
• Type 3: Notch is greater in vertical length than transverse length.
• Type 4: Bony foramen.
• Type 5: Notch and a bony foramen.
A specific vascular structure to recognize is the suprascapular artery which courses superior to the transverse scapular ligament (the nerve travels inferior to the ligament) and along the scapular spine (Figure 64-1).
Important anatomy to consider when performing this block:
• Spine of scapula
• Inferior angle of the scapula
• Coracoid process
• Trapezius muscle
• Clavicle
CONCERNS AND CONTRAINDICATIONS
Unlike other nerve blocks to the shoulder including the interscalene and supraclavicular block, the suprascapular block is less invasive and carries a decreased risk to the patient. However, this does not preclude the fact that each patient needs to be carefully examined and the risks and benefits be weighed before the procedure.
Some basic concerns/contraindications as in all nerve blocks include:
• Patient refusal
• Lack of knowledge of the practitioner
• Complicated anatomy
• Infection at the site
• Coagulopathy
PREOPERATIVE CONSIDERATIONS
The preoperative considerations may vary slightly depending on the technique chosen for this nerve block. This should therefore be taken into account.
• Proper history and physical to exclude any infectious/malignant etiology that could potentially complicate the results
• Informed consent
• Patient needs to be able to be cooperative and alert in order to give feedback such as paresthesias
• Able to sit comfortably (for ultrasound and “blind” technique) or prone (for fluoroscopic technique)
• Allergies to any medications
Equipment Needed
These will vary based on the technique used.
Equipment for direct/indirect “blind” approach:
• 21-gauge 38-mm spinal needle
• 25-gauge needle for local administration
• 10-cc syringe for local anesthetic
• 3-cc syringe for local medication
• Marking pen
Equipment for the ultrasound block will have the following added:
• Ultrasound with linear probe
• Sterile ultrasound cover
Equipment for Fluoroscopic Procedure
• 22-gauge 8- to 10-cm needle
• 25-gauge needle for local
• 3-cc syringe for local medication
• 3-cc syringe for medication
• Connector tubing
Medications
• 1% lidocaine
• Bupivacaine 0.5%
• Methylprednisolone 40 mg or triamcinolone 20 mg
• Antiseptic solution for skin preparation
Technique
There have been several different techniques illustrated for the suprascapular nerve block. These include:
• Wertheim method (“classic”) directing at suprascapular notch
• Dangoisse modified method—directing at the supraspinous fossa
• Ultrasound guided
• Fluoroscopic guided
The “Classic” Approach
• The Wertheim approach, first described in 1941, relies on surface anatomy, patient participation as the needle produces paresthesias in proximity to the nerve.
• The patient is sitting with hands at sides and head and shoulder slightly flexed.
• Landmarks are identified and drawn on the patient.
• A line is drawn along the spine of the scapula from the base of spine to the medial border of the bone.
• A second line is then drawn from the inferior angle of the scapula and this will bisect the first line drawn (Figure 64-2).
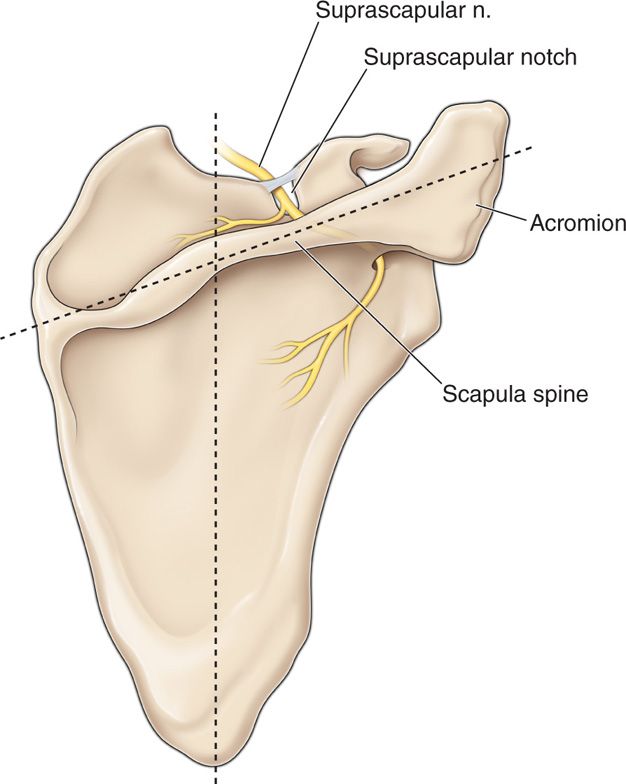
Figure 64-2. Technique for suprascapular nerve block. One line drawn from inferior angle of scapular. A second line along scapular spine. The Wertheim method adds a third line bisecting in the upper outer quadrant.
• A third line is then drawn that bisects the upper outer triangle formed from the 2 lines (Figure 64-3).
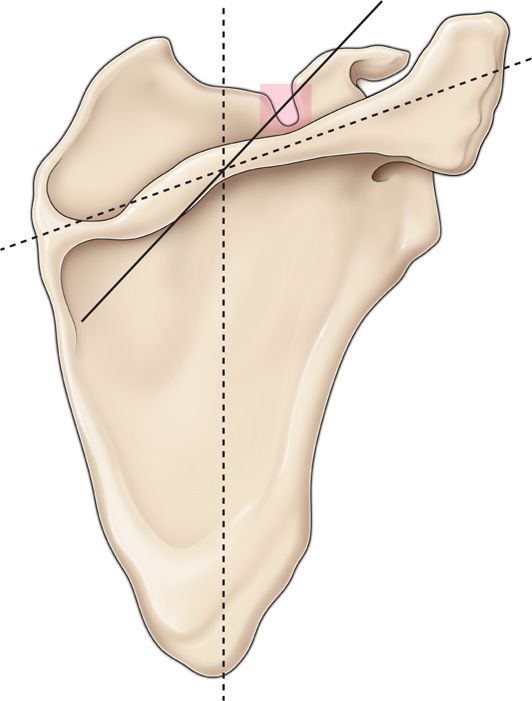
Figure 64-3. The Wertheim method adds a third line bisecting the outer quadrant.
• After sterile preparation and local anesthesia, a point 1.5 cm along this third line is the point of introduction for the needle.
• This is directed caudally and medially until it enters the notch.
• The patient should experience paresthesias to the apex of the shoulder.
• There is a greater risk of pneumothorax with this technique rather than directing at the supraspinous fossa, although the risk is still minimal.
The Dangoisse-Modified Method
Our preferred method is an alternative approach (still using landmarks only) that indirectly affects the nerve and carries a reduced risk of pneumothorax.
• Patient is sitting with arms at sides and head and shoulder slightly flexed.
• Using a marking pen, a line is drawn along the scapular spine.
• A second line is drawn from the inferior angle of the spine perpendicular cephalad to bisect the first line.
• The area is prepped in a sterile fashion.
• A 3-cc syringe attached to a 25-gauge needle is filled with 1% lidocaine which is used to infiltrate the skin approximately 2.5 cm laterally from the bisected line along the spine.
• The 21-gauge spinal needle is inserted at the previously anesthetized area and walked off the superior portion of the spine and advanced until the needle makes contact with the bony floor of the supraspinous fossa.
• A 10-cc syringe with the medication is attached, aspirated, then given slowly.* This will “fill” supraspinous fossa and thus bathe the suprascapular nerve (Figure 64-4).
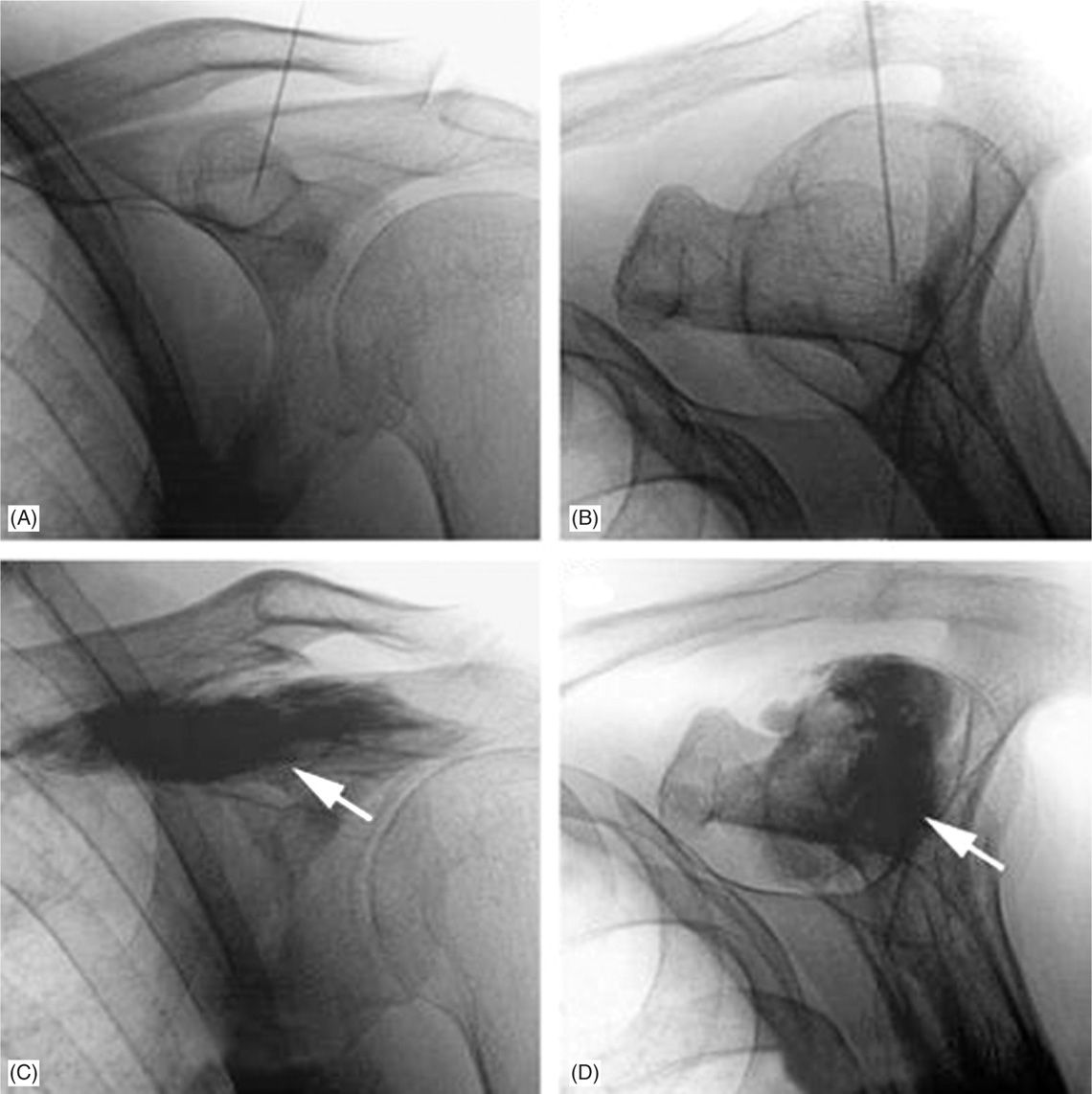
Figure 64-4. Fluoroscopic image of the suprascapular nerve block under fluoroscopy (taken with patient sitting). Contrast was given to delineate the suprascapular fossa. A, AP view; B, Neers view; C, AP view with visualization of suprascapular fossa; D, Neers view.
Ultrasound-Guided Technique
• The ultrasound technique utilizes the indirect method with the added convenience of enhanced visualization.
• The ultrasound is placed parallel to the scapular spine and moved cephalad to identify the suprascapular fossa.
• It is then moved laterally to identify the suprascapular notch where the nerve will exit.
• The nerve is seen as a round hyperechoic structure inferior to the transverse scapular ligament. The needle should be continually visualized while the medication is injected.
• To note, having the patient flex his/her elbow and placing it on the opposite shoulder theoretically decrease the pneumothorax risk additionally by moving the scapular away from the posterior chest wall.
Fluoroscopy-Guided Technique
• The fluoroscopic-guided block is mainly described in the literature when performing a radiofrequency or pulse radiofrequency lesioning of the nerve for intractable and refractory shoulder pain.
• This is reasonable and logical method for this procedure considering the need for increased accuracy for this technique.
• It also provides the benefit of having to use less local anesthetic due to its higher accuracy.
• The patient is placed prone on the table.
• The area is prepped and draped in a sterile manner.
• The suprascapular notch is identified by placing the C-arm in cephalocaudad and an angle slightly oblique approximately 15 to 20 degrees (Figure 64-5).
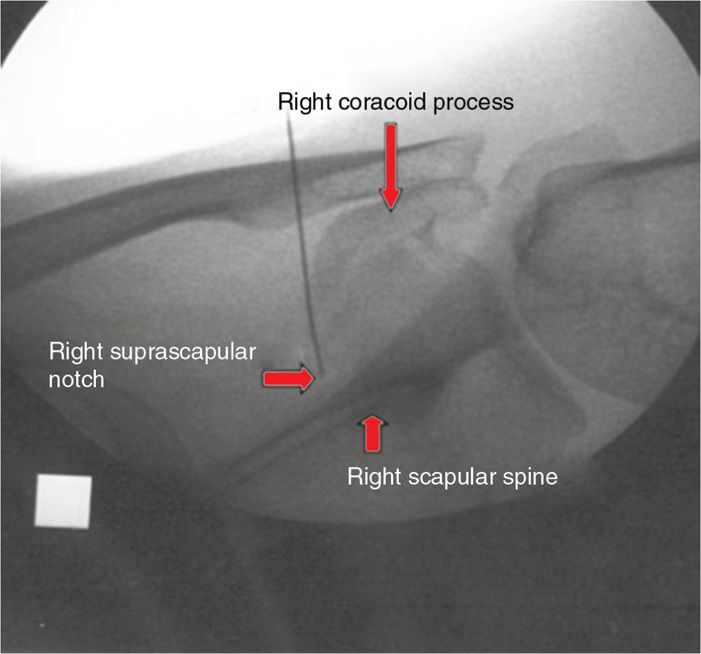
Figure 64-5. View of RF needle placement with fluoroscopy in a suprascapular block.
• Local anesthetic is given after locating the notch and the needle is inserted carefully with subsequent administration of the medication.
• If an RF procedure is performed, sensory and motor information is important to ascertain from the patient before proceeding with the lesioning of the nerve.
POSTPROCEDURE FOLLOW-UP
Adequate pain relief and possible complications need to be addressed by contacting the patient the following day.
The patient should be monitored for:
• Any chest pain or difficulty breathing possibly from a pneumothorax
• Bleeding
• Fever or other signs of infection
COMPLICATIONS
Unlike other blocks for the shoulder including the interscalene and supraclavicular blocks that have higher risks such as inadvertent epidural or spinal anesthesia and vertebral artery injection, one of the benefits of the suprascapular block is its minimal risks with the most cited being that of a pneumothorax. The commonly reported complications with this procedure are:
• Pneumothorax (<1%)
• Inadvertent vascular injection and injury
• Infection
• Neuritis
CLINICAL PEARLS
• The suprascapular nerve provides 70% of sensory to the shoulder and provides motor to both the supraspinatus and infraspinatus muscle.
• The suprascapular block is a relatively safe and easy block to perform and can be diagnostic and/or therapeutic.
• The most cited risk is a pneumothorax which still carries only <1% chance.
• It is not sufficient to cover surgery but is helpful in the postoperative state.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree







