CHAPTER 61
Substance Abuse
Stephen Paul Holzemer, PhD, RN • Joanne K. Singleton, PhD, RN, FNP-BC, FNAP, FNYAM
The use of alcohol and other legal as well as illegal chemical substances is a growing problem in many societies. Approximately 10% to 20% of a primary care provider’s caseload involves patients with substance-use disorders. Problems exist in data collection as it relates to multisubstance abuse. Often, only a subset of substances are identified, unless a thorough assessment is completed (Substance Abuse and Mental Health Services Administration [SAMHSA], 2011, 2012, a, b). Substance abuse has a profound effect on the mortality and morbidity of many patients, their families, and their communities. The social cost related to accidental death, violence, loss of productivity in the workforce, and unemployment can only be estimated. A definition of substance abuse must include the behavior of the patient and the effect of the abuse on the family unit and the community at large.
This chapter is a general overview of substance abuse problems and challenges for the provider. A review of these issues should be made on a patient-by-patient basis because of the many complexities of substance abuse. Providers must construct an interprofessional approach based on the demographics of their practice. The term substance abuse is used in this chapter to include concepts of heavy and frequent use and misuse. Patient-centered care would rely on assessing and intervening into patterns of substance use as soon as possible.
 GENERAL PRINCIPLES FOR PLANNING CARE
GENERAL PRINCIPLES FOR PLANNING CARE
Substance abuse is complicated because the drugs involved may be prescribed, purchased over the counter, or sold in illegal transactions. The addictive nature of these substances makes changing the using behavior difficult. Some patients may become physically or emotionally abusive if the pattern of their drug use changes, and including if or when they experience drug withdrawal. Identifying, engaging, and managing the active substance user includes cooperation between primary care providers and an emerging cadre of specialists in substance abuse.
Primary care providers must first examine their own attitudes about substance abuse. Providers must define what is acceptable and unacceptable use, with the patient, and how to motivate or encourage patients to change their behavior as necessary. Exploring these issues with the patient allows care to be provided from a supportive but well-pl anned perspective. The plan of care involves family members and other support persons willing or able to participate in recovery.
Providers are encouraged to incorporate principles of drug addiction treatment into their daily interaction with patients. Table 61.1 provides essential principles for consideration. Patients are expected to participate in their recovery, when the primary care provider approaches the topics of substance abuse with honesty and understanding.
 ANATOMY, PHYSIOLOGY, AND PATHOLOGY
ANATOMY, PHYSIOLOGY, AND PATHOLOGY
The effect of substance abuse on body systems ranges from temporary impairment to multisystem failure. Long-term drug use can cause diseases of the lungs (cancer), liver (cirrhosis), heart (cardiac myopathy, ischemia, and hypertension), and gastrointestinal tract (gastritis, hemorrhage, and malnutrition). Alcohol use has been associated with breast cancer in women, as well as demineralization of the bone. Cocaine has induced wide complex dysrhythmia in some patients and myocardial infarction. Another level of disease contracted from risk behavior (HIV/HCV) while under the influence of drugs is a growing concern (National Institute on Drug Abuse, 2012). Substance abuse is linked to many other mental or behavioral disorders (American Psychiatric Association [APA], 2013). Patients may present to the primary care provider only after serious physical or mental health problems surface.
Changes in pleasure pathways occur in the brain and the number and receptivity of dopamine and serotonin receptors increase with substance use. These changes add to the physiologic challenge in substance use, which is sometimes overshadowed by the psychosocial aspects. Finding a chromosomal link to a biologic cause or predisposition to addiction would help predict who would be at risk for these health-related problems, so proper intervention can be attempted.
Principles of Drug Addiction Treatment |
1. Addiction is a complex but treatable disease that affects brain function and behavior. Drugs alter the brain’s structure and how it functions, resulting in changes that persist long after drug use has ceased. This may help explain why abusers are at risk for relapse even after long periods of abstinence.
2. No single treatment is appropriate for everyone. Matching treatment settings, interventions, and services to an individual’s particular problems and needs is critical to his or her ultimate success.
3. Treatment needs to be readily available. Because drug-addicted individuals may be uncertain about entering treatment, taking advantage of available services the moment people are ready for treatment is critical. Potential patients can be lost if treatment is not immediately available or readily accessible.
4. Effective treatment attends to multiple needs of the individual, not just his or her drug abuse. To be effective, treatment must address the individual’s drug abuse and any associated medical, psychological, social, vocational, and legal problems.
5. Remaining in treatment for an adequate period of time is critical. The appropriate duration for an individual depends on the type and degree of his or her problems and needs. Research indicates that most addicted individuals need at least 3 months in treatment to significantly reduce or stop their drug use and that the best outcomes occur with longer durations of treatment.
6. Counseling—individual and/or group—and other behavioral therapies are the most commonly used forms of drug abuse treatment. Behavioral therapies vary in their focus and may involve addressing a patient’s motivations to change, building skills to resist drug use, replacing drug-using activities with constructive and rewarding activities, improving problem-solving skills, and facilitating better interpersonal relationships.
7. Medications are an important element of treatment for many patients, especially when combined with counseling and other behavioral therapies. For example, methadone and buprenorphine are effective in helping individuals addicted to heroin or other opioids stabilize their lives and reduce their illicit drug use. Also, for persons addicted to nicotine, a nicotine replacement product (nicotine patches or gum) or an oral medication (buproprion or varenicline) can be an effective component of treatment when part of a comprehensive behavioral treatment program.
8. An individual’s treatment and services plan must be assessed continually and modified as necessary to ensure it meets his or her changing needs. A patient may require varying combinations of services and treatment components during the course of treatment and recovery. In addition to counseling or psychotherapy, a patient may require medication, medical services, family therapy, parenting instruction, vocational rehabilitation and/or social and legal services. For many patients, a continuing care approach provides the best results, with treatment intensity varying according to a person’s changing needs.
9. Many drug-addicted individuals also have other mental disorders. Because drug abuse and addiction—both of which are mental disorders—often co-occur with other mental illnesses, patients presenting with one condition should be assessed for the other(s). And when these problems co-occur, treatment should address both (or all), including the use of medications as appropriate.
10. Medically assisted detoxification is only the first stage of addiction treatment and by itself does little to change long-term drug abuse. Although medically assisted detoxification can safely manage the acute physical symptoms of withdrawal, detoxification alone is rarely sufficient to help addicted individuals achieve long-term abstinence. Thus, patients should be encouraged to continue drug treatment following detoxification.
11. Treatment does not need to be voluntary to be effective. Sanctions or enticements from family, employment settings, and/or the criminal justice system can significantly increase treatment entry, retention rates, and the ultimate success of drug treatment interventions.
12. Drug use during treatment must be monitored continuously, as lapses during treatment do occur. Knowing their drug use is being monitored can be a powerful incentive for patients and can help them withstand urges to use drugs. Monitoring also provides an early indication of a return to drug use, signaling a possible need to adjust an individual’s treatment plan to better meet his or her needs.
13. Treatment programs should assess patients for the presence of HIV/AIDS, hepatitis B and C, tuberculosis, and other infectious diseases, as well as provide targeted risk-reduction counseling to help patients modify or change behaviors that place them at risk of contracting or spreading infectious diseases. Targeted counseling specifically focused on reducing infectious disease risk can help patients further reduce or avoid substance-related and other high-risk behaviors. Treatment providers should encourage and support HIV screening and inform patients that highly active antiretroviral therapy (HAART) has proven effective in combating HIV, including among drug-abusing populations.
HAART, highly active antiretroviral therapy.
Source: Adapted from National Institute on Drug Abuse (2012).
 EPIDEMIOLOGY
EPIDEMIOLOGY
Substance abuse accounts for at least half of the deaths attributed to unsafe or unhealthy lifestyle behaviors. The morbidity often extends to include relatives and friends of the substance user. For example, children may have asthma attacks triggered by tobacco use (second-hand smoke). Family members may experience physical, emotional, and economic harm because of the behavior of the substance abuser. Family members and others may be the victims of crime when substance abusers seek money for drugs or are under the influence of drugs. The wide variation in the physical, occupational, and economic attributes of drug users suggests that all patients should be screened for substance use and potential abuse. No clear profile of a typical substance user has emerged.
Alcohol Use
Up to 75% of the population have consumed alcohol. Approximately 80,000 deaths are attributed to excessive use (Centers for Disease Control and Prevention [CDC], 2013a), but alcohol impairment, adding to other intentional or unintentional accidents or acts, resulting in death or injury, cannot be calculated.
About 20% of men and slightly fewer women smoke. One in five deaths is related to cigarette smoking, with almost 50,000 deaths related to second-hand smoke exposure. Smoking in general is on the decline in the United States, but it remains the primary unhealthy type of behavior. For every death from tobacco use, approximately 20 other people suffer serious medical problems from smoking (CDC, 2013b). The impact of electronic cigarette smoking on health is being studied with little information available on how it relates to standard tobacco products.
Other Drug Misuse
Improper use of prescription and or illegal drugs is a critical health concern. The total scope of the problem will probably never be understood because of underreporting of problems related to the illegal nature of the problem. Opioid abuse costs, for example, are approximately $60 billion with 45% related to workplace costs (loss of productivity), 45% related to health care costs (treatment), and 10% related to criminal justice costs (CDC, 2013c). These costs do not estimate the loss of human potential as it impacts the health of individuals, families, and communities.
Un- and Under-Regulated Pain Management Services
Drug addiction for many has its roots in un- and under-regulated pain management services and practices. Poorly controlled pain, or pain management by under- or unqualified personnel, adds to the availability of pain relief drugs that are easily part of the addiction equation. The role of all primary care providers in the treatment of pain, and monitoring the response and efficacy of treatments for pain is needed (National Institute on Drug Abuse, 2012; Oliver et al., 2012).
Commonly Abused Nonprescribed and Prescribed Drugs
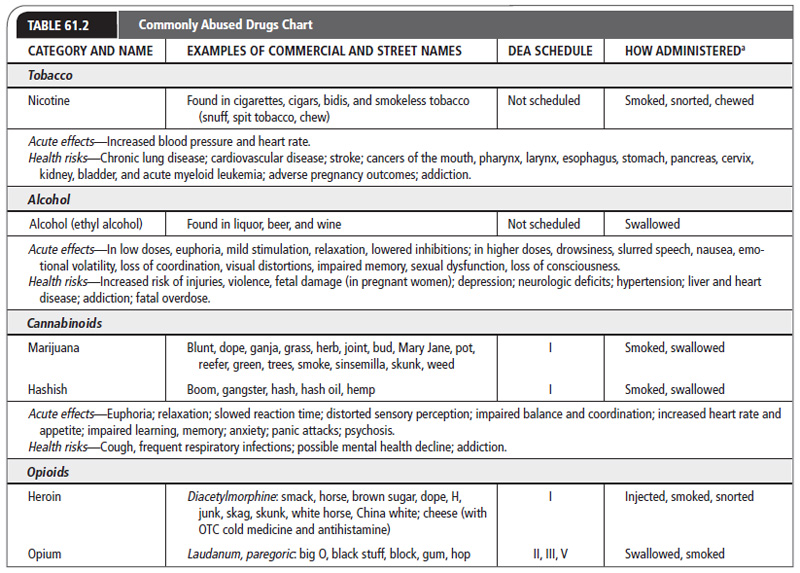
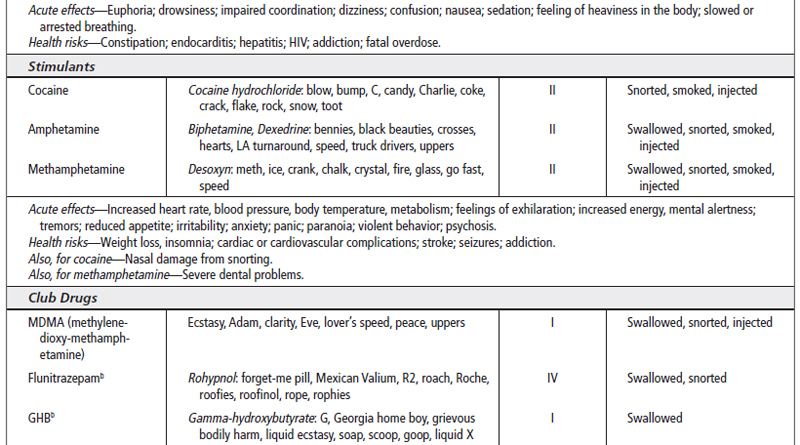
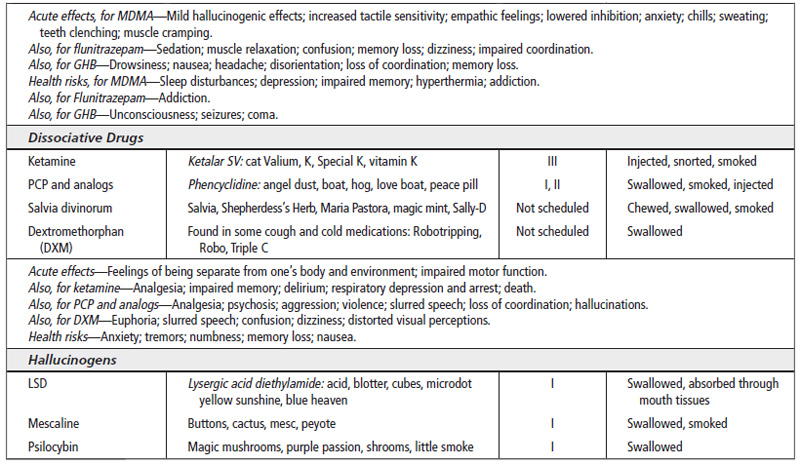
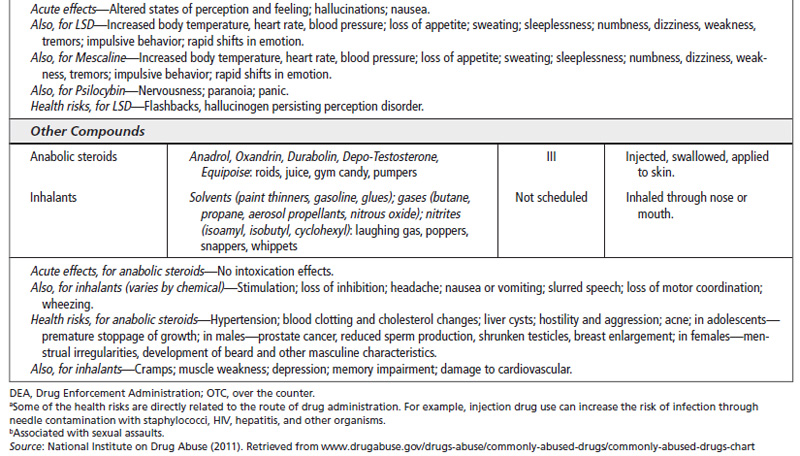
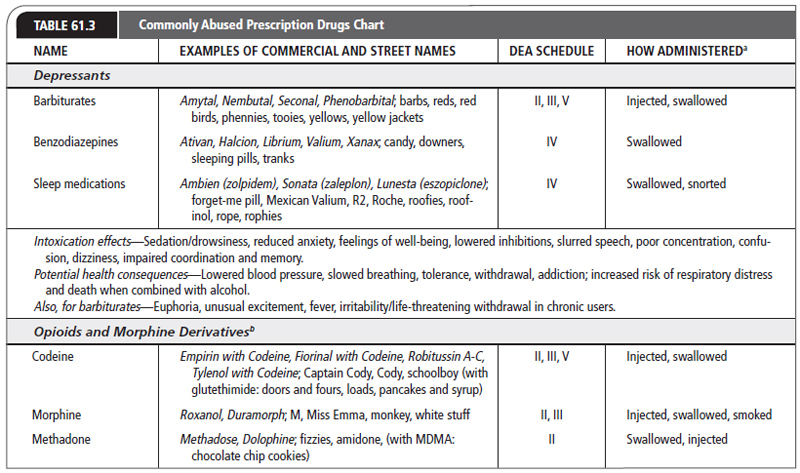
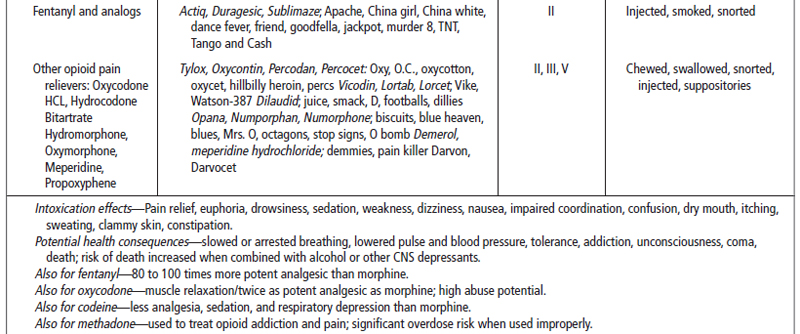
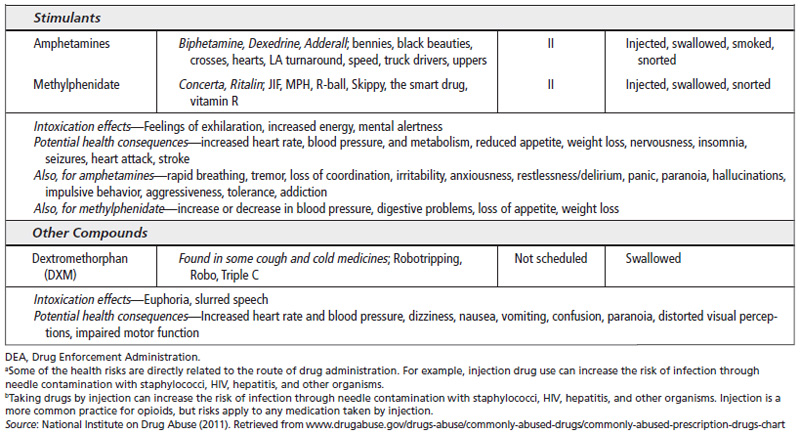
Drugs that are abused are either nonprescribed, or prescribed for a specific use other than recreation, or the desired use of the abuser. Table 61.2 represents some commonly abused drugs, and Table 61.3 presents drugs abused for reasons other than the original prescription.
 HISTORY AND PHYSICAL EXAMINATION
HISTORY AND PHYSICAL EXAMINATION
Screening for alcohol and other drug abuse is a sensitive part of the history and physical examination. An interpersonal relationship between the patient and the provider needs to be established before the provider can expect such questions to be answered in a thorough and honest manner. Some providers ask patients if they have experienced recent trauma (physical or emotional) as a way to elicit problem-drinking behavior. Many accidents are alcohol or other drug related, and the provider needs to screen for alcohol or other drug use when accidental or suspicious trauma occurs.
Questionnaire Assessments
Numerous questionnaires have been designed to identify substance abuse disorders. However, in the absence of a trusting patient-provider relationship, patients may harbor the truth when answering these highly personal questions; a “no” response may be meaningless. Providers must assess the impact of using these questions on their relationship with patients. The most important concept to apply to the use of questionnaires, when they are used, is that a “yes” answer to any question requires further assessment of actual or potential problems related to drug use. The Alcohol Use Disorders Identification Test (AUDIT) is based on a large multinational sample, and attempts to differentiate between harmful alcohoi use, dependence symptoms, and hazardous alcohol use (Babor, Higgins-Biddle, Saunders, & Monteiro, 2001).
Diagnostic Criteria—Mental Health Criteria
The APA, in the Diagnostic and Statistical Manual of Mental Disorders, 5th Edition (DSM-5), identifies substance-related and addictive disorders (related to intoxication and withdrawal) in the following categories:
 Alcohol-related disorders
Alcohol-related disorders
 Caffeine-related disorders
Caffeine-related disorders
 Cannabis-related disorders
Cannabis-related disorders
 Halluc inogen-related disorders
Halluc inogen-related disorders
 Inhala nt-related disorders
Inhala nt-related disorders
 Opioid-related disorders
Opioid-related disorders
 Sedative, hypnotic, or anxiolytic-related disorders
Sedative, hypnotic, or anxiolytic-related disorders
 Stimul ant-related disorders
Stimul ant-related disorders
 Tobacc o-related disorders
Tobacc o-related disorders
 Other (or unknown) substance-related disorder
Other (or unknown) substance-related disorder
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree