CHAPTER 38
Lyme Disease
David I. Jackson, DHSc, PA-C, DFAAPA
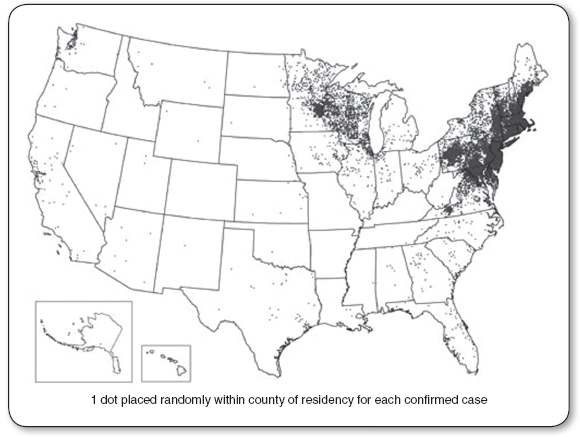
Lyme disease (also called Lyme borreliosis) is a multisystem illness caused by the spirochete Borrelia burgdorferi. It is the most prevalent tick-vectored illness in Europe and the United States (Hubálek, 2009). In 2012, the United States reported 95% of the cases in the Northeast and Great Lakes region (Figure 38.1; Centers for Disease Control and Prevention [CDC], 2013a). The dermatologic and neurologic signs and symptoms were first described in Europe in the early 1900s. In the United States, the first report of a case of erythema migrans (EM), the characteristic skin manifestation, occurred in Wisconsin in 1969. The broader clinical spectrum of the disease was recognized in the mid-1970s with the occurrence of a cluster of arthritis cases in the lower Connecticut River Valley town of Lyme, for which the disease was named.
Largely because this is a complex disease and incompletely studied, knowledge of it has had to be continually updated. This has created confusion and controversy. For example, it was first thought that the etiological agent was a virus until the causative spirochete was discovered (Burgdorfer et al., 1982). Initially, the disease was termed Lyme arthritis, and “no arthritis, no Lyme” was a common dictum. The illness is now known to be more complex, and the name has been changed to Lyme disease. Arthritis is a common, but not necessary, component.
Patients who fulfill the diagnostic criteria are more numerous and geographically widespread than previously thought (Figure 38.1). Both seronegativity and persistent infection after standard antibiotic therapy have been seen. Failure to obtain a positive culture does not prove absence of infection (CDC, 2013a).
The primary care provider’s role is paramount in the diagnosis and treatment of Lyme disease, as early diagnosis and treatment translate into better outcomes. The best opportunity for an accurate early diagnosis is the characteristic EM or bull’s-eye rash stage (Figure 38.2; CDC, 2005a). The rash, however, may be transient, whereas the infection can persist and disseminate.
Patients may get the rash, make an appointment that is 2 weeks away, and then have the rash fade. Believing they are getting well, patients might cancel the appointment, and an early therapeutic and diagnostic opportunity is missed. The rash is often relatively asymptomatic, and because tick bites on the hands and face are unusual, rarely are they found on a cosmetically sensitive body area. This adds to the lack of awareness by the patient of the importance of medical evaluation (which, ideally, should be made within 2 or 3 days of the appearance of symptoms), so the chances of dissemination, canceled appointments, and missed pathology are all increased.
Researchers and providers are still on the front end of the learning curve for this complicated disease, especially when it is in the late or disseminated phase. Providers can best serve their patients with education, early diagnosis, and effective treatment.
 ANATOMY, PHYSIOLOGY, AND PATHOLOGY
ANATOMY, PHYSIOLOGY, AND PATHOLOGY
Pathology
Lyme disease is transmitted by the bite of a tick infected with the causative spirochete, B. burgdorferi. Ixodes scapularis ticks are the main vectors in North America. The tick itself may be as small as the period at the end of this sentence. Incubation time from tick attachment to disease onset can range from 3 to 30 days, with the average being about 1 week (CDC, 2013b). The longer the tick is attached, the greater the likelihood of infection. Ticks that are removed within 24 hours are far less likely to transmit disease (Steere, Coburn, & Glickstein, 2004). Because most tick activity is in the summer, it is no surprise that June and July have the highest infection rates, although some new cases are reported year round (CDC, 2012).
Lyme disease can usually be divided into three phases:
1. Early localized: EM rash only, with no other symptoms.
2. Early disseminated: Rash plus evidence of spread (e.g., fever, headache, lymphadenopathy).
3. Late: Infection has spread sufficiently to cause arthritis, carditis, neurologic involvement, or other late manifestations.
As with other spirochetal diseases, such as syphilis, Lyme borreliosis can have early and late phases and protean clinical manifestations that involve several organ systems. The EM rash involves the skin in about 60% of infected patients. A flu-like illness involving nausea and headache can also occur in the early phase. If untreated, or when treatment failure occurs, Lyme borreliosis can result in the spread of the bacteria to various areas of the body, including the skin, joints, eyes, heart, and the central and peripheral nervous systems. A migratory oligoarthritis is common, with the knee being the joint most commonly affected. The most prevalent neuropathy is facial or seventh nerve palsy (Bell’s palsy). Additional complications can include involvement of other peripheral nerves, radiculoneuropathy, lymphocytic meningitis, acute onset of high-grade (second- or third-degree) heart block, atrioventricular conduction defects, and myocarditis. Less common conditions range from myositis to keratitis.
 EPIDEMIOLOGY
EPIDEMIOLOGY
Most cases of Lyme disease occur in two generally recognized main endemic foci: the northeast and the north-central regions. Lyme disease has been identified in all 50 states. The incidence of Lyme disease within endemic states is 1 per 2,000 (Murray & Shapiro, 2010). Lyme disease has been identified in all age groups, but is most common in 5- to 14-year-olds, with males outnumbering females (Bacon, Kugeler, & Mead, 2008). The CDC reports, “During the localized (early) stage of illness, Lyme disease may be diagnosed clinically in patients who present with an EM rash. Serological tests may be insensitive at this stage. During the disseminated disease, however, serological tests are usually positive” (CDC, 2013b).
 DIAGNOSTIC CRITERIA
DIAGNOSTIC CRITERIA
Lyme disease is a clinical diagnosis that can be very difficult to confirm because the symptoms and signs may mimic those of other diseases. Great care should be taken to consider and rule out other illnesses. If the individual is in contact with the tick less than 24 hours, transmission of Lyme disease is unlikely; therefore, testing and treatment are not recommended. In areas where Lyme is endemic, diagnosis is typically based on clinical findings. Currently, the CDC recommends a two-tiered testing strategy for Lyme disease. The process begins with an enzyme immunoassay (EIA) or immunofluorescence assay (IFA). If the results are negative, an alternative diagnosis should be considered. If the patient has had symptoms for up to 30 days, the provider may treat the patient and follow-up with a convalescent serum. If the first test is positive or yields equivocal results, two options are available: (a) If the patient has had symptoms for up to 30 days, an immunoglobulin M (IgM) Western blot is performed; (b) if the patient has had symptoms for more than 30 days, the immunoglobulin G (IgG) Western blot is performed (CDC, 2011). The CDC has developed surveillance case definitions to be used for national reporting of Lyme disease (Table 38.1). These criteria are not designed for clinical diagnosis, but for surveillance. Patients whose disease meets these surveillance criteria should be reported by notifying the local or state health department. Lyme disease is reportable in all 50 states.
Laboratory Criteria for Diagnosis
For the purposes of surveillance, the definition of a qualified laboratory assay is
 Positive culture for B. burgdorferi, OR
Positive culture for B. burgdorferi, OR
 Two-tier testing (Figure 38.3) interpreted using established criteria, where:
Two-tier testing (Figure 38.3) interpreted using established criteria, where:
 Positive IgM is sufficient only when ≤30 days from symptom onset
Positive IgM is sufficient only when ≤30 days from symptom onset
 Positive IgG is sufficient at any point during illness
Positive IgG is sufficient at any point during illness
 Single-tier IgG immunoblot seropositivity using established criteria
Single-tier IgG immunoblot seropositivity using established criteria
CDC Clinical Case Definition |
CASE CLASSIFICATION |
Confirmed: A case that meets one of the following clinical case definitions: Erythema migrans or at least one late manifestation, as defined below, and laboratory confirmation of infection |
LATE MANIFESTATIONS |
For purposes of surveillance, late manifestations include any of the following when an alternate explanation is not found: |
|
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree