Fig. 13.1
Gastric body partition, gastrojejunostomy, and simple closure of the perforated peptic ulcer. A lateral duodenostomy may be added for bile drainage
For gastric ulcers
While benign gastric ulcers can perforate, excision of the ulcer for pathologic examination is primordial to rule out the possibility of malignancy.
Malignancy, although unusual, occurs in elderly patients.
During the emergency operation, it is often impossible to confirm the diagnosis, particularly when a frozen section is unavailable.
A two-stage operation can be preferred in this setting, with the initial operation being a damage control procedure directed to perforation and peritonitis.
After recovery and histological confirmation of malignancy, adequate staging can be completed, and a radical oncological operation, if appropriate, may be planned.
Nonoperative management
As many as 50 % of perforations will seal without formal surgical intervention, and nonoperative management (NOM) can be an option in these patients if:
Hemodynamically stable
Onset of symptoms of less than 24 h
Minimal pain
Absence of systemic signs of sepsis
Age under 70
Requires close observation and a low threshold for surgical intervention if clinical deterioration occurs
However, all patients with severe comorbidities, hemodynamic instability, onset of symptoms longer that 24 h in duration, peritonitis on physical examination, and systemic signs of sepsis and those who are age 70 or greater should be considered for early operative intervention.
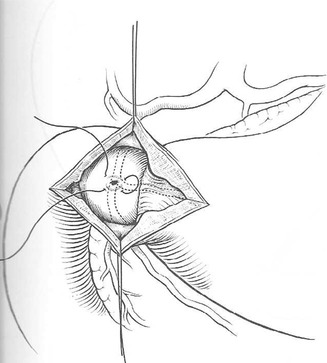
Fig. 13.2
Duodenotomy and suturing
13.3.2 G-D Bleeding
The most common causes of upper GI tract bleeding are gastric and duodenal ulcers (55 %), followed by acute gastric erosions (18 %), Mallory-Weiss tears (10 %), esophageal varices (6 %), and gastric carcinoma (6 %). Surgery for a bleeding ulcer is infrequent today but still necessary in some settings that do not respond to nonsurgical alternatives.
Patients bleeding from ulcers of the posterior wall of the duodenal bulb require surgical treatment when life-threatening hemorrhage cannot be controlled by endoscopic treatment (see upper GI endoscopy) or arterial embolization.
Direct suture (Fig. 13.2)
Hemostasis is obtained via duodenotomy by underrunning the base of the DU (and bleeding vessel) with deeply placed sutures.
Caution is warranted upon duodenotomy closure to avoid narrowing of the lumen.
Dubois’ operation (antroduodenectomy without ulcer excision and gastroduodenal anastomosis) (Fig. 13.3a, b) is an alternative.
Fig. 13.3
(a) Antroduodenectomy, which respects the posterior ulcer without its dissection. (b) For the anastomosis, the posterior side of the gastric stump is applied to the anterior side of the ulcer
13.3.2.1 Risks
Papilla is usually far away, further down.
Common bile duct: an intraoperative cholangiogram should be performed in case of doubt.
Closure: the duodenotomy should be closed without constricting the lumen (prefer sutures perpendicular to intestinal lumen)
For example, when duodenotomy is extended across the pylorus (Heineke-Mikulicz pyloroplasty)
In the rare cases of persistent bleeding after sphincterotomy by ERCP, a longitudinal duodenotomy in the second part will allow access to the papilla of Vater. After control by suture ligature, it is advisable to convert the sphincterotomy to sphincteroplasty.
13.4 Surgical Techniques
13.4.1 Access and Exposure
13.4.1.1 Incisions
Both the stomach and duodenum can be reached easily via a midline laparotomy.
An extended transverse incision offers adequate duodenal exposure.
For laparoscopic access, the trocar setup is similar to that for elective gastric (and hiatal) surgery, or for the duodenum, as for cholecystectomy.
13.4.1.2 Intraoperative Landmarks
The pylorus is recognized by palpation in open surgery and by the pyloric vein of Mayo in both open and laparoscopic surgery.
13.4.1.3 Exposure
In open surgery, the posterior wall of D1 can be explored from the lesser sac, by opening a window in the gastrohepatic ligament and the greater omentum. The right index finger is placed to palpate the posterior wall.
Complete exposure and mobilization of the whole duodenum can be achieved either through laparoscopy or laparotomy with two maneuvers:
1.
Kocher’s maneuver (KM)
KM0 allows access to the supra-mesocolic duodenum.
The retroperitoneum is opened lateral to the duodenal loop (D2).
The peritoneal incision continues through an avascular plane, extending from the lower part of the foramen of Winslow along the lateral border of D2 down to the right portion of the root of the transverse mesocolon, until revealing the right genital vein, inferior vena cava, and aorta (Fig. 13.4). This allows visualization of D3.
Fig. 13.4
Kocher’s maneuver
2.
The Cattell and Braasch maneuver (right medial visceral rotation) (Fig. 13.5)

Fig. 13.5
The Cattell and Braasch maneuver
The right and transverse colon and the root of the small bowel are moved to the left.
Small bowel is mobilized by sharply incising its retroperitoneal attachments from the right lower quadrant to the ligament of Treitz.
Incision of the ligament of Treitz allows mobilization of the duodenojejunal juncture and exposes D4.
13.4.1.4 Duodenal Decompression
Rationale: protect the primary duodenal repair with the goal of decreasing the risk of duodenal suture dehiscence.
Techniques
Duodenostomy tube
The tube should exit the duodenum away from the suture line, preferably from the duodenal stump closed around the tube, and the site should be covered with the omentum. An external drainage should be placed next to the suture line.
Different techniques of decompression have been used (Fig. 13.6):
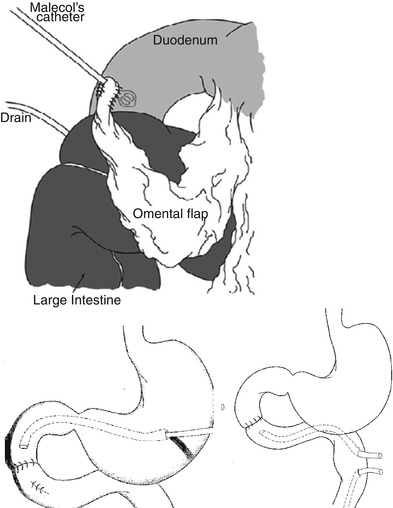
Fig. 13.6
Different techniques of duodenal decompression
Primary, where the tube is inserted into the duodenum and the exit site is covered with a few stitches (Witzel technique)
Antegrade, where the duodenum is proximally decompressed with a tube passed through a gastrotomy and across the pylorus
Retrograde, where the tube is placed distally through the jejunum
Triple tube decompression was introduced in trauma surgery as a “triple ostomy” (nasogastric tube or gastrostomy, retrograde and antegrade tubes for duodenal decompression, and feeding jejunostomy, respectively). Disadvantages include new perforations in the gastrointestinal tract, lack of evidence as to the efficacy to decompress appropriately, and the possibility of accidental tube extraction.
The duodenostomy tube stays patent for a few days and should not be removed until the tube path has been blocked, usually after minimum of 10–12 days (interval variable according to the indication, the local and general conditions of the patient, bowel function recovery, and nutritional status).
13.4.1.5 Duodenal Resection
Very uncommon.
Resection of D1 can theoretically be done in cases of complicated duodenal ulcers.
Resection of D2 is not possible because of the shared vascular supply with the pancreas.
Mobilization of the duodenum a few millimeters from the pancreas is necessary to avoid tension.
Interrupted nonabsorbable 3/0–4/0 sutures are preferable.
A drain should always be left in place, and depending on circumstances, a tube duodenostomy might be considered.
In atypical resections, mainly in D2 and D3, when duodenoduodenostomy is not possible, several alternatives exist:
Roux-en-Y duodenojejunostomy (preferred)
Jejunal patch
Special situation: hemorrhage from an aortoduodenal fistula.
D3 is fixed retroperitoneally and in close proximity to the aorta and therefore is the bowel segment most vulnerable to vascular impingement.
Besides aortic reconstruction with patch graft, a duodenorraphy or segmental duodenal resection might be necessary (access via Cattell and Braasch maneuver).
13.4.1.6 Pyloric Exclusion (Fig. 13.7)
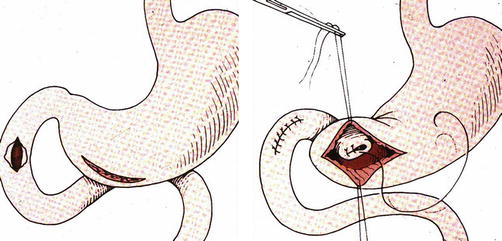
Fig. 13.7
Pyloric exclusion
Devised in trauma setting as alternative to the more extensive duodenal diverticulization procedure (goals: shorten the operative time and make the procedure reversible)
Indicated after large posterior iatrogenic duodenal perforations during ERCP and/or stent placement when the perforation (seen many hours after the insult) is not amenable to primary closure (induration and inflammation of the tissues)
Technique:
After primary repair of the duodenal defect, if possible.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree







