Stabilization and Transport
Monica E. Kleinman
Aaron J. Donoghue
Richard A. Orr
Niranjan “Tex” Kissoon
KEY POINTS
 Pediatric critical care transport programs are designed to improve the safety and outcome for critically ill or injured children who require interfacility transfer for specialized care. Resuscitation and stabilization prior to transport are important principles to prevent patient deterioration en route between hospitals.
Pediatric critical care transport programs are designed to improve the safety and outcome for critically ill or injured children who require interfacility transfer for specialized care. Resuscitation and stabilization prior to transport are important principles to prevent patient deterioration en route between hospitals. Providing intensive care in a mobile environment is associated with unique challenges and risks in comparison to the inpatient setting. Aeromedical transport is associated with additional physiologic stresses that should be considered when preparing a patient for interfacility transport.
Providing intensive care in a mobile environment is associated with unique challenges and risks in comparison to the inpatient setting. Aeromedical transport is associated with additional physiologic stresses that should be considered when preparing a patient for interfacility transport. Most critical care therapies can be provided during transport, although little evidence exists for specific treatments that improve patient outcome.
Most critical care therapies can be provided during transport, although little evidence exists for specific treatments that improve patient outcome. Specialized pediatric transport teams appear to have advantages over general critical care teams in terms of appropriateness of therapy and adverse events and, in retrospective studies, reduced mortality. In most cases, children are more likely to benefit from the expertise of the transport team members than from the speed of travel.
Specialized pediatric transport teams appear to have advantages over general critical care teams in terms of appropriateness of therapy and adverse events and, in retrospective studies, reduced mortality. In most cases, children are more likely to benefit from the expertise of the transport team members than from the speed of travel.In developed countries, pediatric critical care is delivered in dedicated specialty units in which trained personnel and advanced resources are concentrated, usually within tertiary care centers. Critically ill or injured children who are admitted to a PICU have an improved outcome compared with children who are admitted to an adult ICU (1). Therefore, it is often necessary to transfer critically ill or injured children to another facility to obtain the appropriate level of pediatric critical care services. Transport is a particularly high-risk phase of a child’s care due to the limitations of a mobile environment with restricted space and resources. Through access to critical care services that traditionally are not available until arrival at the tertiary care center, the use of a specialty transport team may improve patient safety and outcome either by the prevention of deterioration or by the initiation of specific therapies. Pediatric transport programs permit hospitals to extend critical care services into the community so that patients can benefit from specialty care prior to and during interfacility transfer.
HISTORIC DEVELOPMENT OF PEDIATRIC TRANSPORT PROGRAMS
The history of pediatric transport medicine is relatively short compared with other aspects of emergency and critical care. The first formal guidelines for air and ground transports of children were issued by the American Academy of Pediatrics (AAP) in 1986 (2). Shortly thereafter, the AAP granted task force status to Interhospital Transport, and the Section on Transport Medicine was officially established in 1995. More comprehensive guidelines were published in 1993 (3), with subsequent revisions in 1999 and 2006 (4,5).
TRANSPORT IN DEVELOPING COUNTRIES
Most of this chapter focuses on the development and attributes of highly sophisticated tertiary care transport systems in developed countries; however, many alternatives and ingenious systems have evolved in resource-limited settings or less-developed emergency medical and tertiary care networks. Transport is a neglected aspect of care in many areas of the world due to lack of resources (trained personnel, vehicles, resources to pay personnel, lack of roads, and attacks on transport vehicles during conflicts) (6). Under these circumstances, adverse events are high, and improvement in outcomes is not demonstrated. Deciding whether developing and transitional countries should have PICU transport involves a balance of the overall health priorities of that community, and decisions can only be made locally with full knowledge of continuous quality improvement (QI) data. Sophisticated transport systems are unlikely to decrease overall mortality if resources are simply diverted from one entity to another. Sophisticated transport efforts may be of little benefit and may not lead to improved outcomes if pre-PICU practice (IV fluids, supplemental oxygen, bag-valve-mask ventilation and intubation equipment, proper monitoring and resuscitation protocols, etc.) and tertiary PICU facilities are not improved first (7). In resource-limited settings, the cost benefit of a retrieval team must be balanced against compelling and competing primary healthcare priorities such as nutrition, primary care, and immunizations (8). These competing interests and limitations aside, home-grown solutions include bicycles with trailers, tricycles with platforms, motor boats, ox carts in Tanzania, and taxis and buses driven by drivers with training in prehospital emergency management in Ghana. In many other areas of the world, no transport options are available. Despite severely
limited resources for such communities, from a patient perowpanective, the principles and considerations for sound transport medicine are the same in resource-rich and resource-poor settings.
limited resources for such communities, from a patient perowpanective, the principles and considerations for sound transport medicine are the same in resource-rich and resource-poor settings.
ORGANIZATION OF PEDIATRIC TRANSPORT SYSTEMS
Pediatric critical care transport programs are part of the continuum of care of emergency medical services (EMS) for children and are intended to provide a safe environment during transfer between healthcare institutions. In designing a pediatric transport program to meet the specific needs of the region served, considerations should include the resources of the referring and receiving hospitals, the characteristics of the patient population, and the area’s geography and accessibility.
Most specialty pediatric transport services are hospital based. Several models exist, including the use of on-duty staff who are relieved of other duties to perform patient transport, “on-call” staff who respond from home, and dedicated pediatric transport team members who are on-site and do not have other patient care responsibilities. Each program design has obvious advantages and disadvantages in terms of mobilization time, personnel utilization, and cost. No consensus exists concerning the volume of patient transfers required to justify a dedicated pediatric transport team, and each institution must consider the economic and staffing implications of the various program structures.
Established transport services have certain organizational features in common. In addition to trained and qualified staff, essential components include (a) online medical control by qualified physicians, (b) ground and air ambulance capabilities, (c) a coordinated communications system, (d) written clinical and operational guidelines, (e) a comprehensive program for quality and performance improvement, (f) a database to track activity and permit patient follow-up, (g) medical and nursing leadership, (h) administrative resources, and (i) institutional endorsement and financial support (5).
Administrative Issues
While the pediatric transport team’s primary objective is to provide high-quality critical care services, there are myriad administrative considerations that distinguish operation of a transport program from other hospital-based activities. Among other things, the transport program leadership has responsibility for treatment protocols, ambulance licensure, emergency vehicle operation and maintenance, and transfer agreements. Clinicians, medical directors, and administrative leaders must closely collaborate to ensure the safety and quality of all aspects of the transport system. A full discussion of the administrative issues is beyond the scope of this chapter, but there are several excellent resources in print and online (5) (http://www.emscnrc.org/EMSC_Resources/Publications.aspx).
Training, Certification, and Licensure
Most transport teams are multidisciplinary and include members with expertise in communications and out-of-hospital care and highly trained hospital-based providers. At present, no uniform national curriculum exists for critical care transport clinicians, either adult or pediatric. Several organizations have nationally recognized certification programs for certain types of transport team members, such as flight nurses and critical care paramedics. Although board certification or a certificate of special competency in transport medicine has not yet been established, most physicians who provide medical direction or participate in patient care during transport are trained in emergency medicine, critical care, or neonatology. Attending physicians who provide medical control to the team must be licensed to practice medicine in the state in which the base hospital is located. If physicians in training (fellows or residents) are part of the transport team, requirements for participation, supervision, and evaluation must be developed. Orientation to the specialized transport equipment and safety considerations in the mobile environment are essential, as many physicians have never practiced acute care outside a hospital setting.
Multiple standardized life support courses provide certification in specialty areas such as neonatal resuscitation, pediatric resuscitation, advanced trauma care, and disaster management. While these programs provide an opportunity for skills review and to practice a consistent approach to common acute situations, they are not adequate to establish competency in a specific area of clinical care. While there are no evidence-based guidelines for initial training requirements for nonphysician transport providers, recommendations have been published for procedural training for pediatric and neonatal transport nurses, as well as guidelines for skill assessment and retention (9,10).
The term “scope of practice” describes the clinical abilities and skill set for each team member, and may vary depending on an individual’s educational background or experience, even among staff with the same professional degree. Scope of practice is also used to refer to the specific clinical activities permitted by a healthcare facility or state regulatory agency such as the Department of Health. As healthcare providers, transport team members must be licensed for their professional practice according to the regulations of the state in which their service is based.
Standard operating procedures, protocols, and guidelines should be established for transport team members by the team’s administrative and medical leadership. Patient care protocols define a team’s usual approach to specific patient problems and, for nonphysician teams, provide standing orders for therapies that can be provided without contact with medical control. Protocols also allow the team to function in the event that a patient’s condition changes and the medical control physician cannot be immediately contacted.
Many transport teams provide services in multiple states or even in multiple countries. It is not necessary for each transport team professional to be licensed in every jurisdiction in which the team may provide patient care; instead, transport personnel are considered to be practicing within their home state for purposes of licensure, regardless of the patient’s location. Transport team members are typically credentialed by the institution where they are based or with which they are primarily affiliated. However, by the nature of their work, they regularly provide patient care in facilities in which they do not have clinical privileges. This situation is best addressed by the creation of preapproved interfacility transfer agreements between the referring and receiving institutions.
Finances and Reimbursement
Just as emergency medical care for critically ill or injured children should be provided regardless of the patient’s insurance status or ability to pay, a transport team’s response to a request for emergent interfacility transfer should not depend on financial factors. Regardless, it is important to recognize that transport services are resource intensive and, when considered in isolation, typically represent a source of revenue loss for an individual patient. Administrators must understand that transport teams facilitate patient entry into the hospital’s system and cannot be expected to be independently profitable.
On a less-measurable basis, the availability of high-quality interfacility transport services is expected to promote satisfaction and appreciation among referring physicians and families.
On a less-measurable basis, the availability of high-quality interfacility transport services is expected to promote satisfaction and appreciation among referring physicians and families.
Reimbursement for critical care transport services varies widely among states and between insurance providers. As in other areas of healthcare, reimbursement for transport services has consistently declined while costs have increased. If the transport team composition includes an attending physician, CPT codes exist for face-to-face care of a child during transport. Additional codes include those for telephone consultation with the referring physician prior to the transport team’s arrival, and non-face-to-face medical direction provided by the medical control physician.
Most costs (e.g., equipment and salaries) associated with operating a critical care transport service are fixed. Significant expenses include vehicle maintenance, repairs, and insurance; durable medical equipment; and disposable supplies. As in other areas of healthcare, personnel salaries and benefits constitute most of a transport team’s budget, and as team members are often more senior and experienced, their salaries may be accordingly higher.
In the United States, the practice of interfacility patient transfer is regulated by federal laws that serve to protect patients who present to Medicare-participating hospitals with an emergency condition. The Consolidated Omnibus Budget Reconciliation Act (COBRA) was first passed in 1986; one component of this legislation was the Emergency Medical Transportation and Labor Act (EMTALA). EMTALA was created to prevent “patient dumping”; that is, the transfer to another facility of an individual presenting for emergency care without assessment or stabilizing treatment (Table 26.1). EMTALA was last revised in 2010, and regular revisions can be expected in the future (http://www.cms.hhs.gov/EMTALA) (11). Physicians who transfer patients under emergency circumstances should be aware of the regulations in their practice locale and be familiar with the requirements for communication and documentation (12).
Risk Management and Insurance
Unlike personnel who function solely within a hospital setting, transport team members provide care in hazardous environments during ground and air transports. Because they are exposed to an increased risk of injury and death, programs should consider requesting additional insurance coverage for staff participating in critical care transport. Collisions and crashes involving pediatric and neonatal teams are uncommon, with surveillance data suggesting that one collision or crash occurs for every 1000 patient transports. Collisions or crashes resulting in serious injuries or death are even less common and occur at a rate of 0.55 injuries or deaths per 1000 transports (13). Although most fatal events are the result of aircraft crashes, ground collisions account for most transportrelated injuries and are often moderate or severe in nature. Because transport team members tend to be young, with many productive years ahead of them, disability coverage is important to provide financial security following an accident or work-related injury.
|
Transfer Agreements
It is important to cultivate relationships with transferring facilities to promote patient referrals and to improve the coordination of patient care. In the current financial climate, many smaller hospitals are reducing pediatric subspecialty services and referring sicker children to tertiary facilities. Transfer agreements establish policies that clearly define administrative procedures and the roles and responsibilities of the referring and receiving facilities. These agreements may include language that indicates acceptance of acutely ill patients by the receiving hospital, as well as an understanding that recuperating patients will be eturned to the referring facility. Transfer agreements must comply with local, state, and federal mandates. The EMS for Children (EMSC) program has published sample pediatric transfer guidelines for adoption by different states or programs (http://www.emscnrc.org).
Quality Improvement and Accreditation
The construction of a well-functioning transport program begins with a strong foundation of personnel, training, equipment, communication system, and vehicles (ambulance, helicopter, and/or fixed-wing aircraft). Continued monitoring and evaluation of the transport program are critical to ensuring quality patient care and promoting the program’s success. A written QI plan is essential and should begin with an explanation of the mission of the transport service and the goals for the QI program. It should delineate the lines of authority for performing quality measurement activities and should demonstrate how that authority interfaces with the governing body for the transport service. A QI program should establish criteria to ensure that the standards of care are practiced by individuals and groups, linking the transport team with the medical director, administrative team, risk management, and other pertinent disciplines to identify opportunities to improve care. Transport programs should analyze every component of the services that they provide to ensure effective, consistent, safe, and state-of-the-art care.
The medical director must actively participate in the QI process if it is to be a viable component of the transport program. The medical director serves in various capacities as a resource, supervisor, moderator, evaluator, and educator. Activities for the medical director related to QI include interviewing, hiring, educating personnel, developing treatment protocols, and reviewing and critiquing clinical care. Supervision of patient care during transport (i.e., online medical control) via direct communication is another important component of ensuring quality of care. The medical director should oversee the posttransport case review process, including audits of charts, recorded audiotapes, and morbidity and mortality conferences.
The Commission on Accreditation of Medical Transport Systems (CAMTS) is an organization that aims to improve the quality of patient care and safety of the transport environment through its voluntary accreditation process. Although originally focused on air transport services, CAMTS now surveys ground, rotor-wing, and fixed-wing programs. Accreditation consists of an application process, site survey, and program review to evaluate the transport service using measurable standards and objective criteria. Accreditation standards are revised every 2-3 years with input from representatives of the medical profession to reflect the dynamic nature of the critical care transport field. As of October 2012, 149 services in North America were accredited by CAMTS. The most recent CAMTS standards for accreditation (9th edition) were released in August 2012 and updated in November 2012 (http://www.camts.org).
THE TRANSPORT ENVIRONMENT
Prehospital Care versus Critical Care Transport
EMS include all aspects of basic life support, advanced life support, and critical care transport in which emergency care is provided at a scene and/or in a vehicle. EMS encompass the prehospital and interfacility components of transport and include hospital-based specialty teams. Most pediatric critical care transport programs provide interfacility transport but do not routinely respond to the scene of an accident or emergency, except if a crash is encountered during travel or if a multicasualty incident or disaster occurs.
Prehospital care providers have variable educational backgrounds and experience in the care of critically ill or injured children. Less than 10% of all ambulance calls nationwide are for infants and children; only a few involve advanced life support, and even less can be classified as critical care. Overall, this frequency translates into three pediatric patient encounters per month for ˜60% of the nation’s paramedics, with <3% of the nation’s paramedics providing emergency care for ≥15 children per month (14).
Limited provider exposure to critically ill children presents a challenge to maintaining pediatric assessment and treatment skills. For example, in a moderately-sized EMS system with 50 active advanced life support providers, each provider would be expected to have one pediatric bag-valve-mask case every 1.7 years, one pediatric intubation case every 3.3 years, and one intraosseous cannulation case every 6.7 years (15). It has also been demonstrated that the ability of a prehospital provider to intubate or provide bag-valve-mask ventilation for a child deteriorates significantly in the 6 months following initial training (16). These data should be considered when selecting the appropriate mode of interfacility transport for an ill or injured child.
Currently, no federal regulations specifically address the interfacility transfer of children, other than EMTALA which pertains to all age groups. The federally funded EMSC program (http://www.emscnrc.org), founded in 1984, has as its mission to ensure that all children and adolescents receive state-of-the-art emergency care throughout the EMS system, from prevention through rehabilitation. The EMSC program provides grants to states to improve existing EMS systems and to develop and evaluate protocols and procedures for treating children.
The care of critically ill or injured children during interfacility transport presents unique challenges for assessment, monitoring, diagnosis, and treatment. Thorough preparation and appropriate equipment are required to permit safe and effective management during transport. The clinical assessment of patients, both by physical examination and through the use of monitoring equipment, is more difficult in a mobile environment as compared to within the ICU. Both ground and air transports result in noise levels that can prohibit auscultation of lung and heart sounds. Vehicular motion and vibration can result in artifacts in pulse oximetry, electrocardiography, and oscillometric blood pressure monitoring. Despite these limitations, it is possible to perform advanced procedures in a mobile environment. Published reports have described successful endotracheal intubation, pleural decompression, and intraosseous access during both air and ground transports. In general, however, the risk of performing a procedure during transport is considered higher than that in a stationary setting. As a result, the threshold for establishing a secure airway, for example, is lower when interfacility transport is required.
The capacity for laboratory analysis during transport has traditionally been limited, other than the use of reagent strips or glucometers for blood glucose measurement. Recent technologic advances have produced handheld and portable devices that enable point-of-care (POC) testing through the use of rapid assays, thus permitting the analysis of whole-blood chemistries and blood gases. A retrospective review, over 5 years, by a single institution’s critical care transport team showed that POC testing led to significant management changes in 30% of patients, with bedside blood gas analysis having the highest impact on therapy (17). A similar prospective study was performed in which the transport team sampled arterial blood at the referring hospital and during transport; the results influenced management in 86.2% of the patients, with adjustment in mechanical ventilation being most common (18).
With advances in technology, most therapies available in the ICU can be employed during critical care transport; examples include mechanical ventilation (invasive and noninvasive), continuous infusions, administration of inhaled nitric oxide (iNO), and cardiac pacing. Limitations to the performance of specific therapies are largely due to the inability to safely secure equipment for travel. Despite this, several programs have invested in the necessary vehicle modifications to permit such advanced therapies as extracorporeal membrane oxygenation (ECMO) and high-frequency oscillatory ventilation (HFOV) during interfacility transport (19,20,21).
Ground Transport Considerations
Transport by ground is the most common modality of interfacility and prehospital transport. The advantages of ground transport include virtually ubiquitous access, low cost, and ability to respond in most weather conditions. Ambulances are more spacious than most aeromedical transport vehicles and provide the option to perform procedures or clinical interventions in a stationary setting when necessary. Specially equipped ambulances for children have the capability to transport newborns and small infants in isolettes and can be modified to provide adequate infant and child restraint devices, even for critically ill patients.
The disadvantages of ground transport include the impact of severe winter weather, traffic congestion, and road and highway conditions. The use of sirens to facilitate navigation through traffic, although helpful in expediting transport in urban areas, can impair the ability of the team to perform clinical tasks dependent on auscultation. Teams that perform only ground transports should develop a strong working relationship with teams that provide rotor- and fixed-wing transports to allow for optimal coordination of efforts for transports of critically ill children that are time sensitive or involve travel over long distances.
Aeromedical Transport
Aeromedical transport is widely available in the United States and other developed countries. Both rotor-wing (helicopter) and fixed-wing (airplane) aircraft can be adapted for use as critical care transport vehicles. The use of aeromedical services requires an understanding of the unique physiologic stresses and logistic issues associated with rotor- and fixed-wing transports.
Barometric pressure is defined as the sum of the partial pressures of each of the component gases in the atmosphere; it represents the force or weight exerted by the atmosphere at any given altitude. Barometric pressure at sea level is 760 mm Hg and decreases as altitude increases. The component gases exist in constant proportions: nitrogen (78%), oxygen (21%), and very small percentages of other gases, such as carbon dioxide, helium, and hydrogen.
Dalton’s law states that the total pressure of a gas represents the sum of the partial pressures of the different gas components:
As total barometric pressure decreases with increasing altitude, the partial pressure of each gas is reduced. Likewise, the addition of another gas to the mixture decreases the partial pressure of all other gases.
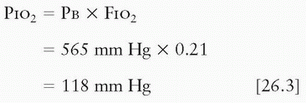
The partial pressure of any inspired gas is determined by the barometric pressure (Pb) and the fraction of the atmospheric gas it represents. In the case of oxygen, for example, PIO2 at sea level can be calculated as follows:
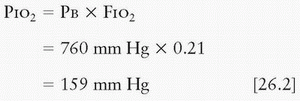
At an altitude of 8000 feet, the partial pressure of inspired oxygen is reduced as follows:
Whereas PiO2 represents the partial pressure of inspired oxygen, the actual partial pressure of oxygen at the alveolar level is affected by the presence of water vapor and carbon dioxide, both of which reduce the partial pressure of oxygen in accordance with Dalton’s law. The amount of carbon dioxide in the alveolar space is, in part, determined by the patient’s metabolism—that is, the respiratory quotient.
The alveolar gas equation defines the relationship between the alveolar partial pressure of oxygen (PaO2), Pb, fraction of oxygen in inspired gas (FIO2), alveolar partial pressure of carbon dioxide (PaCO2), and the respiratory quotient (R), as follows:
Assuming that R is 0.8, PaCO2 is normal (i.e., ˜40 mm Hg), and the partial pressure of water vapor at body temperature (37°C) is 47 mm Hg, the PaO2 while breathing room air at sea level is calculated as follows:
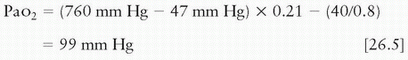
Thus, with increasing altitude and decreasing PB, the resultant PaO2 will decrease. PaO2 can be restored to baseline values by increasing the FIO2. If other factors remain constant, the FIO2 required to maintain the same PaO2 at a lower barometric pressure can be calculated as follows:
The maintenance of a specific barometric pressure in the cabin of an aircraft (i.e., cabin pressurization) ameliorates this effect to some extent, but this is possible only in fixed-wing aircraft and not in helicopters.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree




