
Spontaneous Pneumothorax and Pneumomediastinum
Susan M. Dunmire
Spontaneous pneumothorax and pneumomediastinum are sometimes challenging, yet critical to diagnose and treat for patients presenting in the emergency department (ED). These entities should be considered in any individual who presents with the acute onset of shortness of breath, chest pain, or subcutaneous emphysema.
A pneumothorax is defined by the presence of gas within the pleural space. When it occurs in the absence of penetrating or blunt injury to the chest wall, it is termed a spontaneous pneumothorax. A primary spontaneous pneumothorax occurs in individuals with no clinical or radiographic evidence of lung disease, whereas a secondary spontaneous pneumothorax occurs in individuals with underlying lung pathology. With large accumulations of air in the pleural space, a tension pneumothorax, characterized by hypotension due to impaired venous return, may develop (Fig. 78.1).
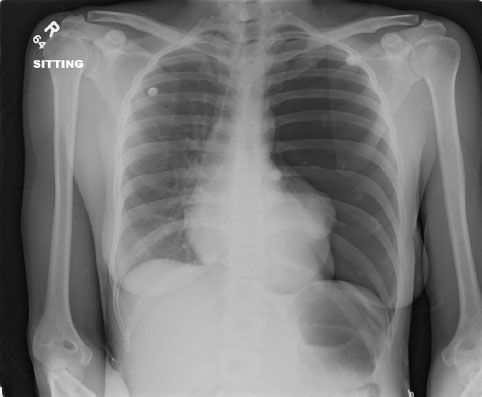
FIGURE 78.1 Left tension pneumothorax with shift of mediastinum to the right.
A primary spontaneous pneumothorax is often the result of rupture of small subpleural cysts or blebs. More than 10% of patients will report a positive family history of spontaneous pneumothorax. A mutation in the gene encoding for folliculin (FLCN) has been identified in individuals with familial spontaneous pneumothorax (1). Spontaneous pneumothorax recurs in up to 50% of patients within 2 years.
One of the most common causes of secondary pneumothorax is chronic obstructive pulmonary disease with rupture of bullae through the visceral pleura. The presentation can be misleading in that patients may report only a worsening of chronic dyspnea. The unsuspected pneumothorax is often found on chest radiography during the evaluation of a suspected exacerbation.
Pneumocystis carinii pneumonia has become an increasingly common cause of secondary pneumothorax. A subgroup of patients with Pneumocystis pneumonia has an accelerated inflammatory response, with spontaneous rupture of necrotic lung tissue, resulting in pneumothorax (2). Other less common causes of secondary pneumothorax include malignancy, asthma (sometimes presenting as sudden severe respiratory compromise), cystic fibrosis, pulmonary infarction, histiocytosis X, and Hamman–Rich syndrome (acute interstitial pulmonary fibrosis). Patients with cystic fibrosis who experience a spontaneous pneumothorax have a significantly higher morbidity and mortality (3). Patients with significant underlying lung pathology may have respiratory decompensation with a relatively small pneumothorax, and therefore require aggressive therapy and close monitoring.
Another less common entity is catamenial pneumothorax. This is a spontaneous pneumothorax occurring in young females at the time of menstruation. Although its etiology is multifactorial, in some patients it is due to small implants of endometrial tissue in the pleural lining (4,5).
Spontaneous pneumomediastinum occurs when there is a sudden increase in intra-alveolar pressure resulting in alveolar rupture and dissection of air into the mediastinum. In a recent retrospective study, the use of illegal drugs (inhaling cocaine, smoking crack cocaine, and smoking marijuana) was the most common precipitating factor for a spontaneous pneumomediastinum (6). Other causes include vomiting, retching, Valsalva maneuver, and a history of recent endoscopy. Although a spontaneous pneumomediastinum is usually a benign entity, more serious causes such as esophageal rupture must be considered.
CLINICAL PRESENTATION
Primary spontaneous pneumothorax commonly occurs in young adults (male-to-female ratio 5:1) between the ages of 20 and 40 (7). Affected individuals tend to be tall and thin and frequently have a history of cigarette smoking (8). There is also a strong association with Marfan syndrome (9).
Patients with spontaneous pneumothorax typically present with the sudden onset of constant ipsilateral chest or shoulder pain that may or may not increase with inspiration. The majority of patients complain of dyspnea, although the severity depends on the size of the pneumothorax. Most patients have the onset of symptoms at rest or during sleep. Rarely, spontaneous pneumothorax can present as a tension pneumothorax with severe cardiopulmonary compromise.
Symptoms in adults with spontaneous pneumomediastinum include retrosternal chest pain and, less frequently, subcutaneous emphysema due to tracking of air into the chest wall, neck, face, abdominal wall, and scrotum. If enough air accumulates in the mediastinum, the pleura can rupture, resulting in an associated pneumothorax in 6% to 10% of patients (10,11). Spontaneous pneumomediastinum in infants is a much more serious entity and can cause cardiopulmonary compromise by compression of the hilum (12).
DIFFERENTIAL DIAGNOSIS
Pulmonary embolism, exacerbation of chronic obstructive pulmonary disease or asthma, pneumonia, thoracic aortic dissection, and myocardial ischemia should all be in the differential diagnosis of a patient with shortness of breath and chest pain. Often the diagnosis of spontaneous pneumothorax is not considered until the chest radiograph is obtained.
Spontaneous pneumomediastinum usually presents as substernal chest pain. The differential diagnosis includes myocardial ischemia, gastroesophageal reflux, pulmonary embolism, and pneumonia.
Once the diagnosis of pneumothorax has been made, the physician should reevaluate the history and physical examination to ensure that there is no sign of blunt or penetrating trauma. An elderly person may have forgotten a recent fall that resulted in rib fractures and an underlying pneumothorax. A puncture site in the neck or supraclavicular area can easily be missed in an unsuspected drug abuser who has penetrated the pleural space.
ED EVALUATION
Physical findings are frequently not helpful in making the diagnosis of a small to moderate sized spontaneous pneumothorax. Patients often exhibit mild resting tachycardia and tachypnea. Depending on the extent of the pneumothorax, breath sounds may be diminished unilaterally. The presence of hypotension, tachycardia (>140 beats/min), or tracheal deviation should immediately alert the emergency physician to the possibility of a tension pneumothorax requiring emergent decompression.The diagnosis of pneumothorax is usually made by chest radiography, which reveals a peripheral lucent area containing no lung markings. It is unnecessary to perform inspiratory and expiratory films as they are equally sensitive for the diagnosis of a pneumothorax (13).
A chest CT is helpful in the detection of a small pneumothorax and pleural blebs. This can guide therapy, as video-assisted thoracoscopic surgery (VATS) may be considered in patients with PSP with visible blebs on CT. CT also allows for assessment of pleural blebs on the contralateral lung.
Bedside ultrasound as a diagnostic tool for pneumothorax has a higher sensitivity and similar specificity to chest radiography (14). It can be useful in the setting of patient who is too unstable to have an upright chest radiograph. Positive findings for pneumothorax include an absence of the lung sliding sign and the comet tail.
Patients with a significant (>25%) pneumothorax have an increase in the alveolar–arterial oxygen gradient, although an arterial blood gas is rarely necessary. The electrocardiogram is not helpful for diagnosis. Nonspecific changes, including T-wave inversion in the precordial leads, decreased amplitude of the R wave, and left axis deviation, are often noted.
The diagnosis of a spontaneous pneumomediastinum is often overlooked and requires a thorough examination and a high index of suspicion. Auscultation of the heart may reveal a “crunching” sound during systole (Hamman sign). Rarely, subcutaneous air may be present. A very thin lucent stripe can be seen outlining the heart and the mediastinum (Fig. 78.2). A lateral neck radiograph may reveal subcutaneous air. Up to 10% of clinically suspected pneumomediastinum will negative chest x-rays. CT scan is 100% sensitive and specific in detecting pneumomediastinum (Fig. 78.3) (15). The electrocardiogram is useful only in helping to rule out ischemia in the patient presenting with substernal chest pain. Additional diagnostic testing, including esophagography, bronchoscopy, and esophagogastroduodenoscopy in nontraumatic pneumomediastinum is rarely indicated unless there is a high clinical suspicion of esophageal rupture (a history of recent instrumentation or forceful vomiting) (16).

FIGURE 78.2 Chest radiograph with pneumomediastinum.









