CHAPTER 44
Splanchnic Nerve Blocks
INDICATIONS
The splanchnic nerves transmit the majority of nociceptive information from the viscera. Classically performed for patients with intra-abdominal cancer, indications recently have expanded to include:
• Chronic abdominal pain1
• Chronic pancreatitis pain2
• Differential diagnosis of somatic versus visceral pain3
• Treatment of patients who have failed to obtain relief from celiac plexus blocks3
• Palliation of the acute pain of arterial embolization of the liver for cancer therapy3
• Treatment of pain of abdominal “angina” associated with visceral arterial insufficiency3
CONTRAINDICATIONS
• Local infection
• Sepsis
• Coagulopathy
• Respiratory insufficiency or pleural adhesions (due to risk of pneumothorax)
• Tumors that distort the relevant anatomy
• An abdominal or thoracic aneurism4
RELEVANT ANATOMY
• The sympathetic innervation of the abdominal viscera originates in the anterolateral horn of the spinal cord.5
• Preganglionic fibers from T5-T12 travel with the ventral roots to join the white communicating rami, pass through the sympathetic chain, and synapse on the celiac ganglia.
• The greater, lesser, and least splanchnic nerves are the major preganglionic of the celiac plexus.
• The greater splanchnic originates from the nerve roots of T5-T10 and travels along the vertebral body, through the crus of the diaphragm, and into the ipsilateral celiac ganglion.
• The lesser splanchnic nerve originates from the T10/T11 nerve roots, while the least splanchnic nerve arises from T10-T12; these also travel through the diaphragm to the ipsilateral celiac ganglion6 (Figure 44-1).
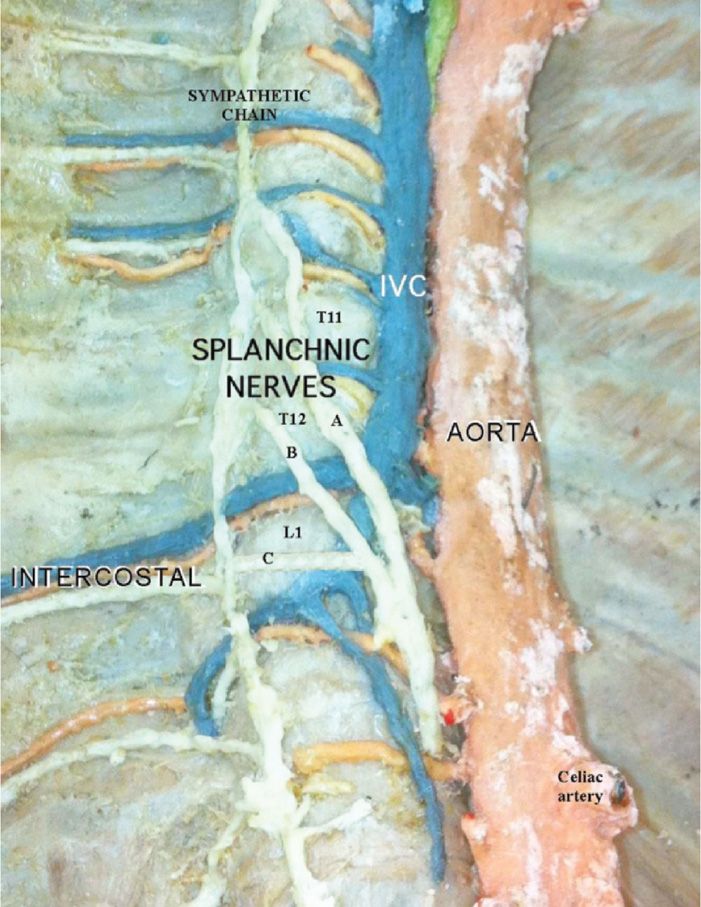
Figure 44-1. Splanchnic nerve anatomy: A = greater splanchnic; B = lesser splanchnic; C = least splanchnic. (Used with permission from Andrea Trescot, MD.)
• These nerves are bound in a narrow compartment made up of the tibial body and pleura laterally, the posterior mediastinum ventrally, and the pleural attachment to the vertebral body dorsally and the crua of the diaphragm caudally.
• The volume of this compartment is approximately 10 cc on each side.7
PREOPERATIVE CONSIDERATIONS
• Documentation of coagulation status and fully informed consent are necessary. Prior to considering neurolysis, the patient should have obtained good but only temporary relief from diagnostic splanchnic blocks, and should be fully aware of the risks of postprocedure diarrhea and orthostatic hypotension form the sympathetic blockade.
• Prior imaging (CT or MRI of the abdomen) should be reviewed preoperatively. Patients usually need sedation, and therefore should be NPO as per the ASA guidelines.
• IV access is mandatory because of the potential hypotension for a successful sympathetic block, and patients are usually pretreated with 500 to 1000 cc of balanced salt solution.
DOCUMENTATION FOR OFF-LABEL INDICATIONS
Because it has traditionally been used only for malignant pain, if the splanchnic nerve block is for chronic, nonmalignant pain, such as chronic pancreatitis, documentation of failure of medication therapy is warranted.
Fluoroscopic Views
Although the technique was originally described as a blind technique, relying on topographic guidance alone,8 fluoroscopic or CT imaging is used. With fluoroscopy, the T12 vertebral body is “squared off” and obliqued to the ipsilateral side.
Positioning of Patient
Patient is positioned prone, usually with a pillow underneath the abdomen. However, patients with ascites or severe abdominal pain may not be able to tolerate the prone position. An anterior approach to the splanchnic nerves is also described below.
Selection of Needles, Medications, and Equipment
• Needles
This technique was originally described utilizing 22-gauge 15-cm Chiba needles. An alternative approach utilizes 22-gauge 3.5-in Quincke (spinal) needles.9 Use of a blunt-tipped, curved needle with an introducer allows the needle to “hug” the vertebral body, stay very medially, and theoretically decrease the risk of pneumothorax. RF needles should be at least as long as those used for the diagnostic procedure, curved and ideally blunt-tipped, with a 10- to 15-mm active tip.
30-gauge needle for skin infiltration
• Extension tubing
• Syringes
2 syringes 5 or 10 cc for medication and contrast.
1 syringe 3 cc for skin infiltration
• Contrast
Nonionic contrast such as Isovue or Omnipaque
• Local anesthetic
For diagnostic and prognostic splanchnic nerve blocks, volumes of local anesthetic ranging from 5 to 10 cc of 1% to 1.5% lidocaine or 0.5% bupivacaine have been described.10 To decrease the risk of local anesthetic toxicity, all local anesthetic should be administered in divided doses.
• Neurolytic agent
For neurolytic injections, 10 cc of absolute alcohol or 6% to 10% aqueous phenol is recommended.10 The phenol can be mixed with contrast.
INTRAOPERATIVE TECHNICAL STEPS
Fluoroscopic Imaging (Posterior Approach)
The original procedure was performed virtually identical to the classic retrocrural approach to the celiac plexus, starting at L1, except that the needles were aimed more cephalad so as to end up at the anterior lateral margin of the T12 vertebral body.11 An alternative approach utilizes 22-gauge, 3.5 in Quincke needles placed 3 to 4 cm lateral to the midline, just below the T12 ribs with slightly mesial trajectory, so that the tip of the needle ends up at the anterolateral margin of T12.
• The patient is placed prone, with a pillow underneath the abdomen, and the T12 vertebral body identified and “squared off” fluoroscopically (Figure 44-2).

Figure 44-2. T12 vertebral body, AP view. (Used with permission from Andrea Trescot, MD.)
• The fluoroscope is then angled obliquely to the ipsilateral side about 45 degrees10 (Figure 44-3).
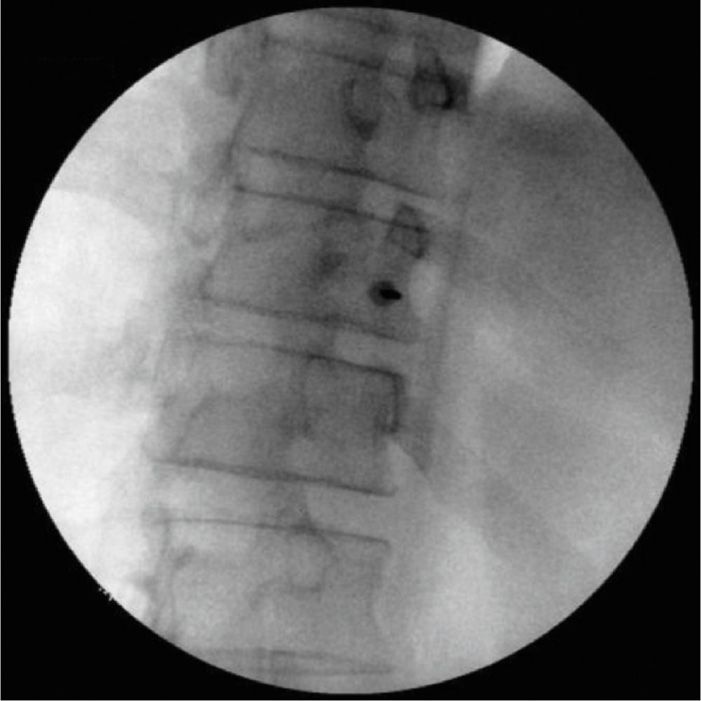
Figure 44-3. Splanchnic injection site, oblique view. (Used with permission from Andrea Trescot, MD.)
• If the diaphragm overlies the T12 vertebra and its rib, then the T11 vertebral body is identified instead.4
• The needle (or introducer if a blunt-tipped needle is used) is then introduced through the skin just over the lateral border of the vertebral body (Figure 44-4). The point of entry for either level (T11 or T12) is at the junction of the rib and vertebra.
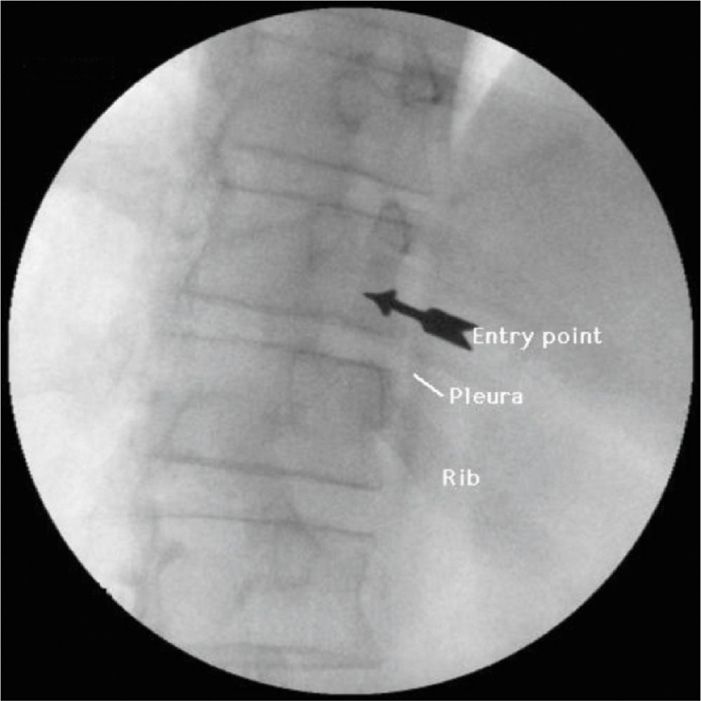
Figure 44-4. Initial needle placement, oblique view. (Used with permission from Andrea Trescot, MD.)
• Placing the entry point slightly caudad of the most narrowed portion of the vertebral body (the waist) will allow the needle to be repositioned slightly superiorly if bony contact was made prior to optimum needle placement.
• In the lateral view, the needle is advanced until it reaches the junction of the anterior one-third and the posterior two-thirds of the vertebral body (Figure 44-5). If using a curved needle, keep the curve pointing medially, rotating the tip laterally briefly if contact with bone is made too early.

Figure 44-5. Final needle placement, lateral view. (Used with permission from Andrea Trescot, MD.)
• Once the final needle placement is confirmed, nonionic contrast is injected to confirm that the tip of the needle is not vascular or intrapleural (Figure 44-6).

Figure 44-6. Contrast injection, oblique view. (Used with permission from Andrea Trescot, MD.)
• Reconstruction CT images may help with visualization of the approach (Figure 44-7A-C)
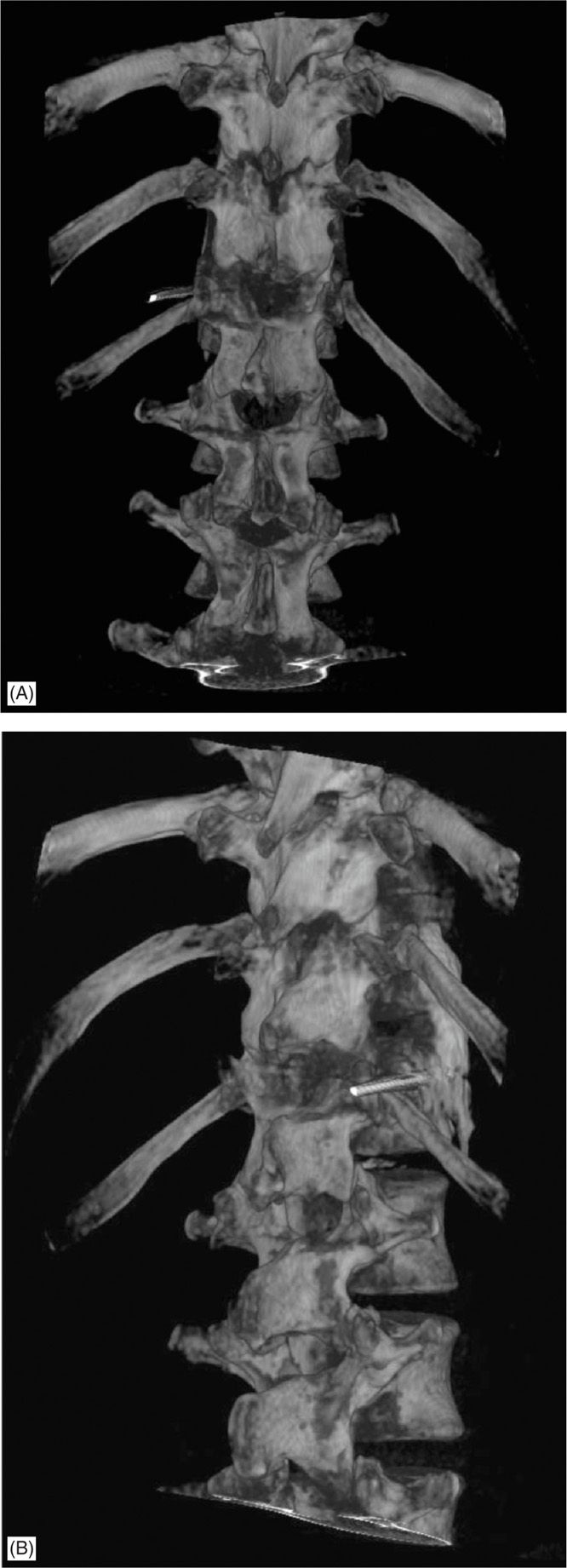

Figure 44-7. (A-C) CT reconstruction splanchnic needle placement. (A) AP view, (B) oblique view, (C) lateral view. (Used with permission from Andrea Trescot, MD.)
Diagnostic blocks
![]() 5 to 10 cc of local anesthetic should give good relief.
5 to 10 cc of local anesthetic should give good relief.
![]() The author uses 1% lidocaine for quick, good relief on the table, followed by same volume of 0.5% bupivacaine about 5 minutes later.
The author uses 1% lidocaine for quick, good relief on the table, followed by same volume of 0.5% bupivacaine about 5 minutes later.
![]() Because of the risk of intravascular injection, all local anesthetic injections should be instilled in divided doses.
Because of the risk of intravascular injection, all local anesthetic injections should be instilled in divided doses.
Neurolytic blocks
![]() 12 to 15cc of absolute alcohol or 6% to 10% phenol is used.10
12 to 15cc of absolute alcohol or 6% to 10% phenol is used.10
![]() Because of the likelihood of pain on injection, a similar volume of local anesthetic should be injected first.
Because of the likelihood of pain on injection, a similar volume of local anesthetic should be injected first.
Radiofrequency ablation
![]() The needle is placed as for the diagnostic injection, in the mid-third of the vertebral body.
The needle is placed as for the diagnostic injection, in the mid-third of the vertebral body.
![]() Once the needle is in place, the stylet is removed and RF probe is placed through the needle.
Once the needle is in place, the stylet is removed and RF probe is placed through the needle.
![]() Impedance should be less than 250 Ω.
Impedance should be less than 250 Ω.
![]() Using sensory stimulation up to 1mV, the patient should report stimulation into the epigastric region.10
Using sensory stimulation up to 1mV, the patient should report stimulation into the epigastric region.10
![]() If the patient reports a band-like stimulation pattern, they are describing intercostal stimulation, and the needle should be advanced slightly.
If the patient reports a band-like stimulation pattern, they are describing intercostal stimulation, and the needle should be advanced slightly.
![]() Motor stimulation up to 2mV should not cause intercostal stimulation.
Motor stimulation up to 2mV should not cause intercostal stimulation.
![]() After the needle is in the proper position, confirmed by stimulation and fluoroscopy patterns, 2 cc of 2% lidocaine is injected through the needle to provide analgesia for the lesioning.
After the needle is in the proper position, confirmed by stimulation and fluoroscopy patterns, 2 cc of 2% lidocaine is injected through the needle to provide analgesia for the lesioning.
![]() It is important to wait for a few (2-3) minutes to allow the local anesthetic to take effect. The author recommends lesioning for 60 seconds at 85 degrees and then repeating after rotating the needle 180 degrees; Waldman and Pratt10 describe 90 seconds at 80 degrees.
It is important to wait for a few (2-3) minutes to allow the local anesthetic to take effect. The author recommends lesioning for 60 seconds at 85 degrees and then repeating after rotating the needle 180 degrees; Waldman and Pratt10 describe 90 seconds at 80 degrees.
![]() After lesioning, inject 2 to 5 cc of 0.5% bupivacaine (with or without 40 mg of methylprednisolone or Sarapin®) to provide postoperative analgesia.
After lesioning, inject 2 to 5 cc of 0.5% bupivacaine (with or without 40 mg of methylprednisolone or Sarapin®) to provide postoperative analgesia.
Fluoroscopic Transdiscal Approach
Plancarte et al12 described a transdiscal posterior approach to the splanchnic nerves.
• The patient is placed in the prone position with a pillow beneath the abdomen. Prophylactic antibiotic should be given intravenously 30 minutes before the procedure.
• The T11-T12 interspace is identified under fluoroscopy.
• Next, the fluoroscopy is obliqued 15 to 20 degrees.
• After local anesthetic infiltration of the skin and the subcutaneous tissues, a 22-gauge, 10-cm needle is introduced lateral to the inferior aspect of the facet joint and advanced through the disc.
• 0.5 cc of contrast solution is administered to verify needle position within the disc by lateral and AP views.
• The needle is then advanced further under lateral fluoroscopic control, using saline in a 3-cc syringe for loss of resistance.
• When the needle has passed outside the disc space, 3 mL of contrast is administered to verify its final position. The dye spread should be a vertical line.
• Plancarte et al used 5 cc of 10% aqueous phenol injected through the needle followed by 0.5 cc of air before drawing the needle back to prevent the spread of the neurolytic solution within the disc material.
• When the needle was drawn back in the disc, cefazolin 50 mg in 1 mL was administered to the disc to prevent discitis, prior to removing the needle completely.
CT Imaging (Anterior Approach)
The theoretical advantages of an anterior CT approach to the splanchnic nerves include:
• Reduced discomfort by avoiding a prolonged prone position
• CT evaluation of anatomic distortions (from tumor or surgery)
• Less sedation for critically ill patients
Mercadante et al13 described an anterior CT approach, using a 20-cm-long needle with a stylet inserted under CT guidance, passing through the space between aorta and vena cava, choosing the best trajectory to avoid organ perforation and to place the tip of the needle in the retrocrural area bilaterally. Two milliliters of contrast medium were injected through both needles to confirm the proper spread. Neurolysis was achieved by injecting 12 mL of alcohol through each needle. An anterior approach involves the passage of the needle through the viscera; however, this is not usually associated with relevant complications.14
Postprocedure Considerations
The risks of splanchnic nerve blocks are similar to those of celiac plexus blocks, though the rate of pneumothorax, thoracic duct injury, and unexpected spread of injected drugs onto the somatic nerve roots are reportedly higher than those for transcrual approaches to the celiac plexus.7 It would be prudent to perform a chest x-ray postoperative to rule out an early pneumothorax, because the needle passes so closely to the lung (Figure 44-8), a reason to consider blunt-tipped needles. Because of the risk of pneumothorax, extreme caution should be used if performing this injection bilaterally at the same sitting.
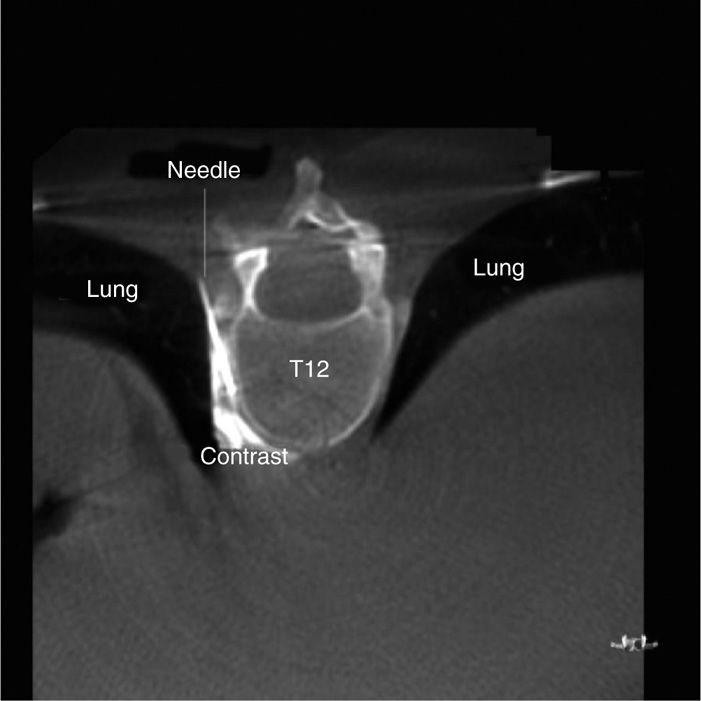
Figure 44-8. CT axial view showing proximity of the needle to the lung. (Used with permission from Andrea Trescot, MD.)
MONITORING OF POTENTIAL COMPLICATIONS
• Because this is a sympathetic block, there is a potential for hypotension, and therefore IV access is necessary. Without fluid prophylaxis (500-1000 cc of balanced salt solution), clinically significant hypotension can be expected in 30% to 60% of patients.15
• Patients also need to be warned regarding orthostatic hypotension and diarrhea as potential side effects.
• Pneumothorax is most obvious potential complication, and patient should be counseled to present to an emergency room if they develop shortness of breath pain or chest pain. Bilateral procedures at the same sitting should be avoided if possible.
• On the left side, chylothorax is a possibility, due to trauma of the thoracic duct.
• Subarachnoid or epidural injections were more common with the blind techniques.15
• Retrograde flow of local anesthetic or neurolytic agents have been described, causing the potential for subarachnoid or epidural injections as well as paraplegia or nerve injuries.10
• Imaging would be expected to decrease the risks of this procedure; however, a large review of complications in 1988 did not show any decrease in complications when using radiologic guidance.16
CLINICAL PEARLS AND PITFALLS
Given the higher incidence of pneumothorax associated with splanchnic nerve block relative to celiac plexus block, splanchnic nerve block perhaps should be reserved for patients with upper abdominal and retroperitoneal pain that fails to respond to celiac plexus block. Waldman and Pratt10 described keeping the tip of the curved RF needle facing laterally initially until it passes the foramen. Then the tip can be turned medially once it reaches the lateral surface of the vertebral body. This ensures the needle remains medial to the interpleural surface and in close contact with the vertebral body. As a reminder, the phrenic nerve also transmits nociceptive information from the upper abdominal viscera, referred to the supraclavicular region and should be considered in all patients with upper abdominal pain.3
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree






