INTRODUCTION AND EPIDEMIOLOGY
Trauma to the spine can cause a vertebral spinal column injury, a spinal cord injury, or both. A few studies have tried to estimate the annual incidence of spinal column injury in the general population with results ranging from 11.8 to 64 cases per 100,000,1,2 but no current figures are available for the U.S. population. In contrast, the estimated annual incidence of spinal cord injury in the United States is 40 cases per million or 12,000 new cases per year, with 81% male victims, a mean age of 42.6 years, and a 67% Caucasian predominance.3 Since 2010, the leading causes of spinal cord injury are vehicular (37%), falls (29%), and violence (14%). Lifetime costs for spinal cord injury victims vary according to age at time of injury, severity of injury, and socioeconomic status; however, estimates range in millions of dollars per patient.3
FUNCTIONAL ANATOMY
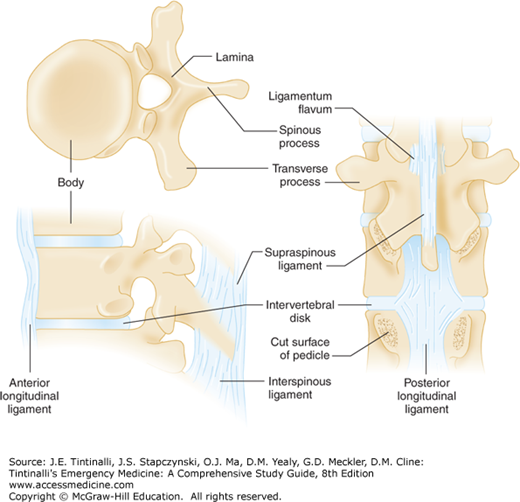
The vertebral column is composed of 33 vertebrae: 7 cervical, 12 thoracic, 5 lumbar, 5 fused sacral, and 4 (usually fused) coccygeal. The axial vertebrae (C1 and C2) are anatomically unique in that they are designed for rotary motion. The odontoid (dens) of the axis (C2) is held against the atlas (C1) by the strong transverse ligament. The remaining vertebrae share some common anatomical features (Figure 258-1). A typical subaxial vertebra is composed of an anterior body and a posterior vertebral arch. The vertebral arch is comprised of two pedicles, two laminae, and seven processes (one spinous, two transverse, and four articular). These articulations enable the spine to engage in flexion, extension, lateral flexion, rotation, or circumduction (combination of all movements). The orientation of these articular facet joints changes at different levels of the spine and accounts for variations in motion of specific regions of the vertebral column. Due to its inherent flexibility, the cervical spine is the most commonly injured region of the spinal column, with most injuries occurring at the C2 level and from C5 to C7.4 The second most common region of injury is in the thoracolumbar transition zone.
A series of ligaments serves to maintain alignment of the spinal column. The anterior and posterior longitudinal ligaments run along the vertebral bodies. Surrounding the vertebral arch are the ligamentum flavum and the supraspinous, interspinous, intertransverse, and capsular ligaments. Between adjacent vertebral bodies are the intervertebral disks, consisting of a peripheral annulus fibrosus and a central nucleus pulposus. The intervertebral disks act as shock absorbers to distribute axial load. When compressive forces exceed the absorptive capacity of the disk, the annulus fibrosus ruptures. This allows the nucleus pulposus to protrude into the vertebral canal, and this may result in spinal nerve or spinal cord compression.
The spinal cord is a cylindrical structure that begins at the foramen magnum, where it is continuous with the medulla oblongata of the brain and extends down the spinal canal to the first and second lumbar vertebrae. The spinal cord gives rise to 31 pairs of spinal nerves: 8 cervical, 12 thoracic, 5 lumbar, 5 sacral, and 1 coccygeal. Each spinal nerve emerges through the intervertebral foramen corresponding to the appropriate spinal cord level. The lower nerve roots form an array of nerves called the cauda equina.
PATHOPHYSIOLOGY
Given their multiple axes of motion, the bony vertebrae can be injured via several mechanisms and present with a number of different injury patterns (Table 258-1).5,6,7,8,9,10
| Mechanism of Injury | Injury | Spinal Column Regions Typically Affected | Image | Notes |
|---|---|---|---|---|
| Flexion | Anterior subluxation (hyperflexion sprain) (usually stable, but depends on the integrity of posterior ligaments) | Cervical |
[Photo contributors: Mark Silverberg, MD/Steven Pulitzer, MD. Reproduced with permission from Shah BR, Lucchesi M, Amodio J (eds): Atlas of Pediatric Emergency Medicine, 2ed, © 2013, McGraw-Hill Education, New York, NY. Figure 20-57.] | Anterior subluxation produces ligamentous failure and may have no associated fractures. Plain films can be normal. However, significant ligamentous injury can display anterior soft tissue swelling, a widening of the spinous processes at the level of injury (“fanning”), posterior widening of the intervertebral space, and cervical disk space alignment ≥11 degrees between adjacent spaces. |
| Atlantoaxial dislocation (unstable) | Cervical |
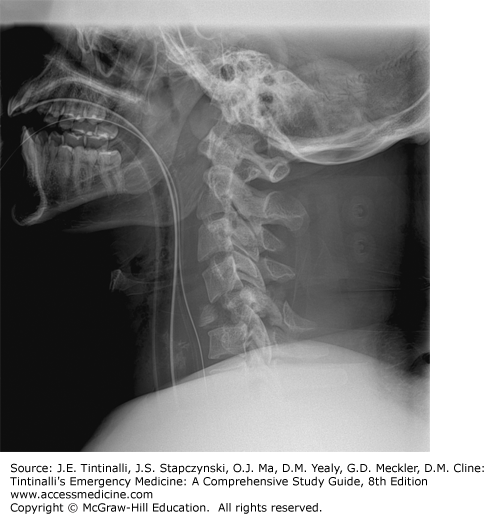
[Used with permission of Jake Block, MD.] | Transverse ligament rupture without an associated fracture can occur in older patients from a direct blow to the occiput. Radiographic diagnosis relies on measuring the predental space, which is the space between the posterior aspect of the anterior arch of C1 and the anterior border of the odontoid. A predental space of >3 mm on a lateral radiograph (2 mm for CT images) implies damage to the transverse ligament; >5 mm implies rupture of the transverse ligament. | |
| Bilateral interfacetal dislocation (unstable) | Cervical |  | Bilateral interfacetal dislocation (locked facets) occurs when the articular masses of one vertebra dislocate anteriorly and superiorly from the articular surfaces of the adjacent vertebra below. Disruption of all ligamentous structures occurs. On radiographs, the vertebral body is dislocated anteriorly ≥50% of its width. These injuries usually present with neurologic deficits due to compromise of the intervertebral foramen, unless the dislocation is only partial (perched facets). | |
| Simple wedge (compression) fracture (usually stable) | Cervical; TL |
[Reproduced with permission from Block J, Jordanov MI, Stack LB, Thurman RJ (eds): The Atlas of Emergency Radiology. McGraw-Hill, Inc., 2013. Fig 11-22 Part A.] | Most common thoracic fracture (52%).5 A vertebral wedge fracture typically involves a fracture of the superior end plate of the vertebral body while sparing the inferior end plate. An isolated simple wedge fracture is stable, but the presence of significant posterior ligamentous disruption can make the injury unstable. A simple wedge fracture is differentiated from a burst fracture by the absence of a vertical fracture of the vertebral body and lack of bulging of the posterior vertebral border. | |
| Spinous process avulsion (clay shoveler’s) fracture (stable) | Cervical |
[Reproduced with permission from Block J, Jordanov MI, Stack LB, Thurman RJ (eds): The Atlas of Emergency Radiology. McGraw-Hill, Inc., 2013. Fig 11-10 Part A.] | This is an avulsion off the end of one of the lower cervical spinous processes (classically C7). It is thought to be caused by strong muscle contractions pulling on the bone via the ligamentous complex. It is not associated with neurologic compromise. | |
| Flexion teardrop fracture (highly unstable) | Cervical |
[Reproduced with permission from Block J, Jordanov MI, Stack LB, Thurman RJ (eds): The Atlas of Emergency Radiology. McGraw-Hill, Inc., 2013. Fig 11-1.] | Extreme hyperflexion causes complete disruption of the spinal ligaments at the level of injury. The “teardrop” is the anteroinferior portion of the vertebral body that is separated and displaced from the vertebral body by the anterior spinal ligament. “Fanning” of the spinous processes may be present, with or without fracture. A sagittal fracture through the vertebral body may be seen on CT. Anterior spinal cord syndrome is associated with this injury | |
| Flexion-rotation | Unilateral facet dislocation (stable unless associated with an articular mass fracture) | Cervical |
[Reproduced with permission from Simon RR, Sherman Scott C (eds): Emergency Orthopedics, 6th ed. McGraw-Hill, Inc., 2011. Fig 9-21B.] | A unilateral facet dislocation occurs when the articular mass and inferior facet on one side of the vertebra are anteriorly dislocated. On a lateral radiograph, the involved vertebral body will be displaced <50% of its width. On the anterior view, the spinous process at the level of the rotation will be pointing toward the side that is dislocated. |
| Fracture of lateral mass (can be unstable) | Cervical |
Comminuted fracture of the lateral mass of C4 extending into the right lamina. | Typically presents with severe neck pain and sometimes radicular symptoms. May be associated with Brown-Séquard syndrome or vertebral artery injury; therefore, some experts feel that magnetic resonance angiography should be done in all patients with this lesion.6 A pillar fracture is a type of lateral mass fracture that consists of an isolated vertical or oblique fracture through the lateral mass. The adjacent lamina and pedicle remain intact. The fractured articular mass is displaced posteriorly and may be visible as a double outline on the lateral radiograph. | |
| Flexion-distraction | Anterior compression with associated transverse fracture through vertebral body (unstable) | TL |
Arrow points to splaying of the posterior elements. [Reproduced with permission from Block J, Jordanov MI, Stack LB, Thurman RJ (eds): The Atlas of Emergency Radiology. McGraw-Hill, Inc., 2013. Fig 11-27C.] | These injuries are associated with seatbelt injuries, especially when lap belts alone are used. Radiographic findings include posterior vertebral wall fracture, increased height of the posterior vertebra, and “fanning” of the spinous processes. The Chance fracture variant presents with minor anterior vertebral compression and significant distraction of the middle and posterior ligamentous structure. It often occurs from T11 to L2 (TL transition zone). These injuries are often misdiagnosed as an anterior compression fracture. They may require CT to visualize and are often associated with intra-abdominal injuries. |
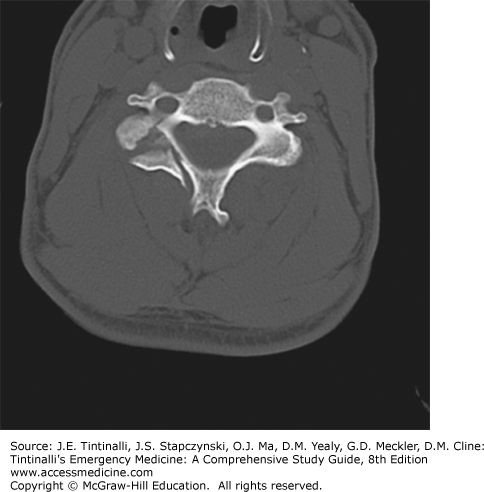
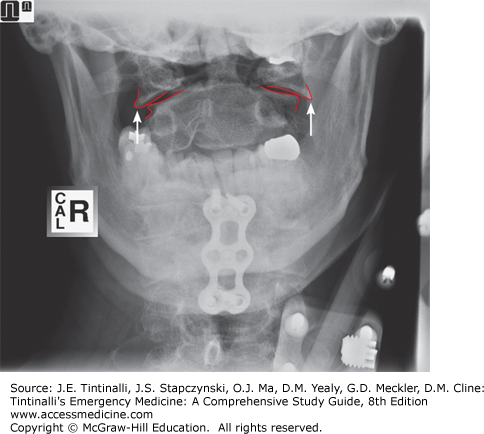
| Vertical compression | Jefferson burst fracture of atlas (potentially unstable) | Cervical |
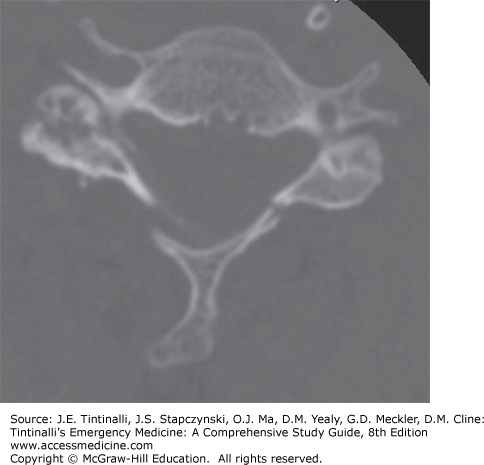
[Reproduced with permission from Block J, Jordanov MI, Stack LB, Thurman RJ (eds): The Atlas of Emergency Radiology. McGraw-Hill, Inc., 2013. Fig 11-13.] | Vertical compression forces the occipital condyles downward and produces a burst fracture by driving the lateral masses of C1 apart. This is best seen as outward displacement of the lateral masses on the open-mouth odontoid radiograph or on CT. If displacement of both lateral masses (measured as offset from the superior corner of the C2 vertebral body on each side) is >7 mm when added together, rupture of the transverse ligament is likely, and the spine is unstable. |
| Burst fracture (unstable) | Cervical; TL |
Arrow shows posterior displacement of posterior vertebral body cortex. [Reproduced with permission from Block J, Jordanov MI, Stack LB, Thurman RJ (eds): The Atlas of Emergency Radiology. McGraw-Hill, Inc., 2013. Fig 11-31B.] | A burst fracture occurs when a vertebra is crushed by an axial load, causing fragments to displace in all directions. The lateral radiograph may show an obvious fracture of the end plates, but sometimes all that is seen is a bowing or disruption of the posterior cortex of the affected vertebra. The anterior radiographic view may show a vertical fracture through the vertebral body and widening of the interpedicular distance. The burst fracture is usually obvious on CT. The spinal cord may be injured if a retropulsed fragment enters the spinal canal. | |
| Extension | Hyperextension dislocation (unstable) | Cervical |
[Reproduced with permission from Schwartz DT (ed): Emergency Radiology: Case Studies. McGraw-Hill, Inc., 2008. Sect V: Cervical Spine Radiology; Fig 6.] | Extreme hyperextension can cause a complete tear of the anterior longitudinal ligament and intervertebral disk, with disruption of the posterior ligamentous complex. On the lateral radiographic view, the vertebrae may appear normal if the dislocation spontaneously reduces or if the injury is masked by a cervical immobilization collar. Prevertebral soft tissue swelling may be the only radiographic finding present. Anterior disk space widening or fracture of the anteroinferior end plate of the vertebral body may occur. Patients usually present with a central cord syndrome. |
| Hyperextension teardrop fracture or extension corner avulsion fracture (unstable in extension) | Cervical |  | Hyperextension may cause the anterior longitudinal ligament to avulse a fragment off the anteroinferior corner of the vertebral body. The height of the avulsed fragment usually exceeds its width. This fracture is more common in older patients with osteoporosis. | |
| Fracture of posterior arch of atlas (stable) | Cervical |
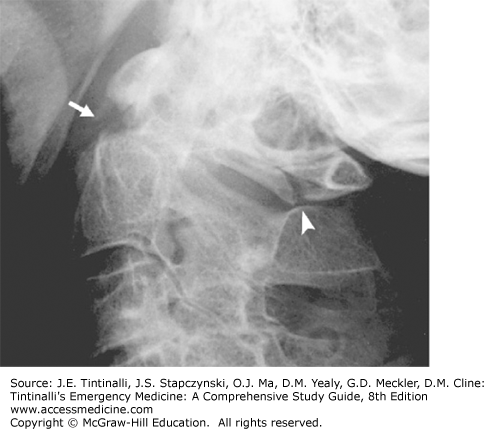
Arrowhead indicates the posterior arch fracture. There is also a displaced dens fracture (arrow). [Reproduced with permission from Galli, et al: Emergency Orthopedics: The Spine. New York, NY: McGraw-Hill;1989] | Fracture occurs from wedging of the posterior arch between the occipital bone and the C2 vertebra. A CT is indicated to rule out an associated Jefferson fracture or a dens fracture. | |
| Laminar fracture (usually stable) | Cervical |
Bilateral laminar fractures. [Reproduced with permission from Simon RR, Sherman SC (eds): Emergency Orthopedics, 6th ed. McGraw-Hill, Inc., 2011. Fig 9-26B.] | Laminar fractures may be associated with spinous process fractures. They may not be evident on plain radiographs and usually require CT for diagnosis. | |
| Traumatic spondylolisthesis (hangman’s fracture) (unstable) | Cervical |  | The hangman’s fracture is a fracture of both pedicles of C2, with the anterior displacement of C2 on C3. This was associated with the neck hyperextension from judicial hangings, where the noose knot is placed under the subject’s chin and snaps the head backward. Suicidal hangings do not usually cause extreme hyperextension and are not associated with the hangman’s fracture. Because the spinal canal at the level of C2 is large, a hangman’s fracture does not cause neurologic injury. | |
| Injuries caused by a combination of mechanisms or poorly understood mechanisms | Occipital condyle fractures (usually stable) | Cervical |
[Reproduced with permission from Block J, Jordanov MI, Stack LB, Thurman RJ (eds): The Atlas of Emergency Radiology. McGraw-Hill, Inc., 2013. Fig 11-11B.] | Occipital condyle fractures are rarely visible on plain radiographs and usually require CT imaging for detection. Presentation is rather variable due to proximity of multiple neurovascular structures.7 Neurologic impairment is common and usually involves lower cranial nerve deficits and/or limb weakness. |
| Atlanto-occipital dissociation (AOD) (highly unstable) | Cervical |
[Photo contributors: Konstantinos Agoritsas, MD/Steven Pulitzer, MD. Reproduced with permission from Shah BR, Lucchesi M, Amodio J (eds): Atlas of Pediatric Emergency Medicine, 2nd ed. © 2013, McGraw-Hill Education, New York, NY. Fig 20-52.] | Secondary to high-energy impact. Historically, strongly associated with mortality8; however, modern patients may survive due to better prehospital care/transport. The classic presentation is paralysis of upper extremities with lack of lower extremity paralysis or weakness (cruciate paralysis).9 However, presentation can be variable with a common presentation being lower cranial nerve deficits. CT may be required for detection. In radiographs in the normal patient, the distance between the basion and the superior cortex of the dens (basion-dental interval [BDI]) should be ≤10 mm in adults (≤8.5 mm on CT). In addition, the distance from the basion to the posterior border of the body of C2 (basion-atlantal interval [BAI]) should be ≤12 mm anterior displacement or ≤4 mm posterior displacement on a lateral radiograph. If there are abnormalities in both the BDI and BAI, this strongly suggests the existence of AOD.10 | |
| Odontoid (dens) fractures (type II and III are unstable) | Cervical |
Type 1 odontoid fracture. [Reproduced with permission from Block J, Jordanov MI, Stack LB, Thurman RJ (eds): The Atlas of Emergency Radiology. McGraw-Hill, Inc., 2013. Fig 11-18.]
Type 2 odontoid fracture. [Reproduced with permission from Block J, Jordanov MI, Stack LB, Thurman RJ (eds): The Atlas of Emergency Radiology. McGraw-Hill, Inc., 2013. Fig 11-19C.]
Type 3 odontoid fracture. [Reproduced with permission from Block J, Jordanov MI, Stack LB, Thurman RJ (eds): The Atlas of Emergency Radiology. McGraw-Hill, Inc., 2013. Fig 11-20C.] | Frequently involves other injuries to the cervical spine and multisystem trauma. Conscious patients will usually describe immediate and severe high cervical pain with muscle spasm. The pain may radiate to the occiput. Neurologic injury is present in 18% to 25% of cases with odontoid fractures, ranging from minimal sensory or motor loss to quadriplegia. Odontoid fractures are classified according to the level of injury. CT can miss odontoid fractures if the fracture line is aligned with the cut of the CT (en face). | |
| Translational fracture-dislocation (unstable) | TL |
T10-T11 fracture-dislocation. | This is a high-energy disruption of all three columns of spine and is readily apparent both on radiographs and CT. Patients commonly present with severe neurologic findings. These fractures are most often unstable; however, in the absence of destabilizing rib cage fractures, lesions above T7 can be stable. | |
| Sacrum and coccyx fractures | Sacral fracture |
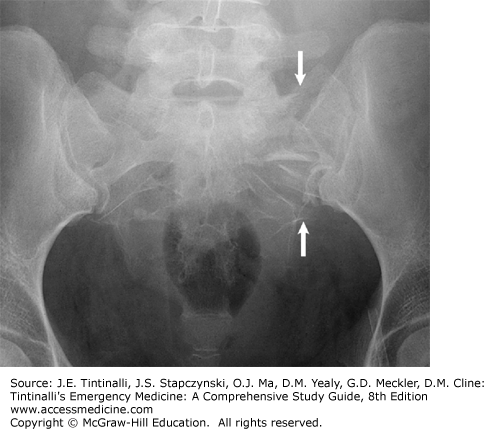
[Reproduced with permission from Block J, Jordanov MI, Stack LB, Thurman RJ (eds): The Atlas of Emergency Radiology. McGraw-Hill, Inc., 2013. Fig 8-16A.] | Usually associated with pelvic fracture(s). Transverse fractures through the body can injure the cauda equina. Longitudinal fractures can cause radiculopathies. Central sacral fracture can present with bowel/bladder incontinence. | |
| Coccyx fracture |
[Reproduced with permission from Block J, Jordanov MI, Stack LB, Thurman RJ (eds): The Atlas of Emergency Radiology. McGraw-Hill, Inc., 2013. Fig 8-24.] | Coccygeal injuries are usually associated with a direct fall onto the buttocks, with resultant coccyx pain exacerbated by sitting or straining. Localized tenderness can be elicited with coccyx palpation during a rectal exam, but this is not required for diagnosis. Imaging is not needed to diagnose coccygeal fractures. Treatment is symptomatic with analgesics and use of a rubber doughnut pillow. |
The variable anatomic qualities of the regions of the spinal column cause characteristic injury patterns in each region. The exposure and extreme mobility of the cervical spine (C1-C7) make it particularly vulnerable to injury, because it is the most flexible and mobile portion of the spinal column. The cervicothoracic junction (C7-T1) is one of the transitional zones of the spinal column, which are locations where the vertebral morphology changes. This designation is important because transitional zones sustain the greatest amount of stress during motion and are most vulnerable to injury. In contrast to the cervical spine, the thoracic spine (T1-T10) is a rigid segment, with its stiffness enhanced by articulation with the rib cage. Therefore, not only is injury to the thoracic spine less common than in other regions, but this also means that the presence of a thoracic vertebral injury indicates the patient was subjected to severe traumatic forces and is at high risk for intrathoracic injuries. Moreover, the spinal canal in the thoracic region is also narrower than in other regions. This increases the risk of cord injury, which is often complete when it occurs. The thoracolumbar junction (T11-L2) is a transitional zone between the highly fixed thoracic and relatively mobile lumbar spine. In addition to this change in bone anatomy, the thoracolumbar junction serves as the level of transition from the end of the spinal cord (about L1) to the nerve roots of the cauda equina. Relative to the thoracic spine, the width of the spinal canal in the thoracolumbar region is greater. Therefore, despite a large number of vertebral injuries at the thoracolumbar junction, most do not have neurologic deficits, or, if present, they are partial or incomplete. Relative to the thoracic and thoracolumbar regions, the lower lumbar spine (L3-L5) is more mobile. Because of the width of the spinal canal in the lumbar region and the ending of the spinal cord at the L1 level, isolated fractures of the lower lumbar spine rarely injure the spinal cord or result in neurologic injury. The sacrum and coccyx form the lower portion of the spinal column. The vertebral foramina of the sacrum together form the sacral canal that contains the nerve roots of the lumbar, sacral, and coccygeal spinal nerves and the filum terminale. The coccyx, which articulates with the sacrum, consists of four vertebrae fused together. When neurologic injuries occur, they are usually complete cauda equina lesions or isolated nerve root deficits. Sacral fractures that involve the central sacral canal can produce bowel or bladder dysfunction.
Much has been written regarding determining whether or not a particular injury is “stable.” Spinal stability is defined as the ability of the spine to limit patterns of displacement under physiologic loads so as not to damage or irritate the spinal cord or nerve roots. Several paradigms have been created, including the Denis column system, which splits the spinal column into anterior, middle, and posterior elements.11 A spine injury is considered unstable if at least two columns of a particular region are involved. Although this schema and other instability scoring systems have been published,12,13,14 determining spinal stability after an acute injury in the ED is particularly difficult. This is because these injuries often occur in the setting of polytrauma, altered mental status, and severe pain, which may result in suboptimal initial imaging. In addition, many EDs lack quick access to emergent MRI to evaluate the spinal ligaments. Therefore, assume any spine fracture is unstable and maintain appropriate precautions until expert consultation can be obtained from a spine surgeon.
Damage to the spinal cord is the result of two types of injury. First is the primary injury from mechanical forces from traumatic impact. This insult sets into motion a series of vascular and chemical processes that lead to secondary injury. The initial phase is characterized by hemorrhage into the cord and formation of edema at the injured site and surrounding region. Local spinal cord ischemia ensues secondary to vasospasm and thrombosis of the small arterioles within the gray and white matter. Extension of edema may further compromise blood flow and increase ischemia. A secondary tissue degeneration phase begins within hours of injury. This is associated with neural membrane dysfunction, driven by a pathologic excitation of sodium ion channels, an influx of calcium ions, and the release of glutamine.15 Cell death ensues from a combination of mechanisms including electrolyte imbalances, cell edema, and the formation and release of oxidative substances.15
The severity of spinal cord injury determines the prognosis for recovery of function, so it is important to distinguish between complete and incomplete spinal cord injuries. The American Spinal Injury Association defines a complete neurologic lesion as the absence of sensory and motor function below the level of injury. This includes loss of function to the level of the lowest sacral segment. In contrast, a lesion is incomplete if sensory, motor, or both functions are partially present below the neurologic level of injury. This may consist only of sacral sensation at the anal mucocutaneous junction or voluntary contraction of the external anal sphincter upon digital examination. Complete lesions have a minimal chance of functional motor recovery. Patients with incomplete lesions are expected to have at least some degree of recovery. The differentiation between complete and incomplete spinal cord damage may be complicated by the presence of spinal shock. Patients in spinal shock lose all reflex activities below the area of injury, and lesions cannot be deemed truly complete until spinal shock has resolved.
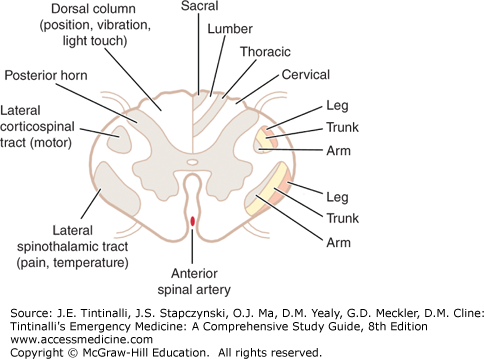
A significant number of descending and ascending tracts have been identified in the spinal cord (Figure 258-2). The three most important of these in terms of neuroanatomic localization of cord lesions are the corticospinal tracts, spinothalamic tracts, and dorsal (posterior) columns.
The corticospinal tract is a descending motor pathway. Its fibers originate from the cerebral cortex through the internal capsule and the middle of the crus cerebri. The tract then breaks up into bundles in the pons and finally collects into a discrete bundle, forming the pyramid of the medulla. In the lower medulla, approximately 90% of the fibers cross to the side opposite that of their origin and descend through the spinal cord as the lateral corticospinal tract. These fibers synapse on lower motor neurons in the spinal cord. The 10% of corticospinal fibers that do not cross in the medulla descend in the anterior funiculus of the cervical and upper thoracic cord levels as the ventral corticospinal tract. Damage to the corticospinal tract neurons (upper motor neurons) in the spinal cord results in ipsilateral clinical findings such as muscle weakness, spasticity, increased deep tendon reflexes, and a Babinski’s sign.
The two major ascending pathways that transmit sensory information are the spinothalamic tracts and the dorsal columns. The spinothalamic tract transmits pain and temperature sensation. As the axons of the first neurons enter the spinal cord, most ascend one or two levels before entering the dorsal gray matter of the spinal cord, where they synapse with the second neuron of the spinothalamic tract. The second neuron immediately crosses the midline in the anterior commissure of the spinal cord and ascends in the anterolateral funiculus as the lateral spinothalamic tract. When the spinothalamic tract is damaged, the patient experiences loss of pain and temperature sensation in the contralateral half of the body. The (pain and temperature) sensory loss begins one or two segments below the level of the damage.
The dorsal columns transmit vibration and proprioceptive information. Neurons enter the spinal cord proximal to pain and temperature neurons. They differ from pain and temperature neurons in that they do not immediately synapse in the spinal cord. Instead, these axons enter the ipsilateral dorsal column and do not synapse until they reach the gracile or cuneate nuclei of the medulla. From these nuclei, fibers cross the midline and ascend in the medial lemniscus to the thalamus. Injury to one side of the dorsal columns will result in ipsilateral loss of vibration and position sense. The sensory loss begins at the level of the lesion. Light touch is transmitted through both the spinothalamic tracts and the dorsal columns. Therefore, light touch is not completely lost unless there is damage to both the spinothalamic tracts and the dorsal columns.
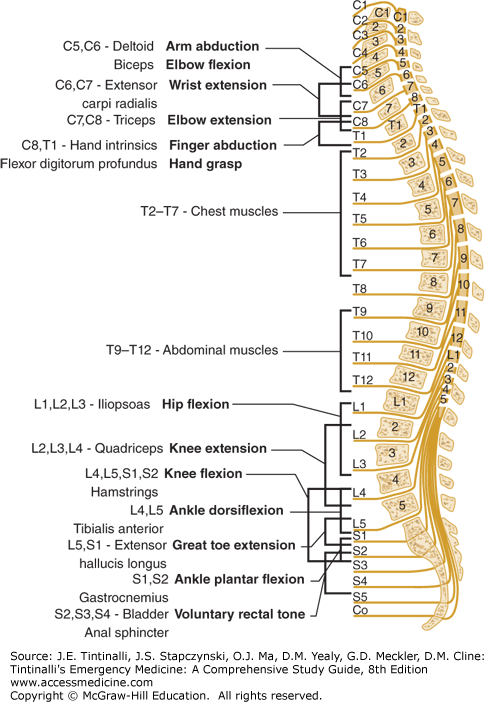
Each spinal nerve is named for its adjacent vertebral body (see Figure 258-3). In the cervical region, there is an additional pair of spinal nerve roots compared to the number of vertebral bodies. The first seven spinal nerves are named for the first seven cervical vertebrae, each exiting through the intervertebral foramen above its corresponding vertebral body. The spinal nerve exiting below C7, however, is referred to as the C8 spinal nerve, although no eighth cervical vertebra exists. All subsequent nerve roots, beginning with T1, exit below the vertebral body for which they are named.
During fetal development, the downward growth of the vertebral column is greater than that of the spinal cord. Because the adult spinal cord ends as the conus medullaris at the level of the lower border of the first lumbar vertebra, the lumbar and sacral nerve roots must continue inferiorly below the termination of the spinal cord to exit from their respective intervertebral foramina. These nerve roots form the cauda equina. A potential consequence of this arrangement is that injury to a single lower vertebra can involve multiple nerve roots in the cauda equina. For example, an injury at the L3 vertebra can involve the L3 nerve root as well as the lower nerve roots that are progressing to a level caudal to the L3 vertebra.
PREHOSPITAL CARE
The prehospital treatment of patients with spinal injury involves recognition of patients at risk, appropriate immobilization, and triage to an appropriate facility (see chapters 1, “Emergency Medical Services” and 2, “Prehospital Equipment”). Presume that patients with an appropriate traumatic mechanism who have complaints of neck or back pain, tenderness on prehospital exam, neurologic complaints, significant injury above the clavicles, or altered sensorium that precludes accurate evaluation of the spine to have a spinal cord injury, and take appropriate spinal precautions. Transport of the patient to a center that is capable of rapid diagnostics and therapeutics is important to optimize outcome following spinal injury.
Prehospital care for spinal injuries traditionally involves immobilization of the entire spine at the scene with a rigid cervical collar (or similar devices) plus a long backboard. However, there is little evidence that cervical collars and/or long spine boards reduce neurologic injury, spinal instability, or mortality.16,17 In contrast, cervical collars and long backboards can induce complications such as pressure sores,18,19 patient discomfort,20 and respiratory compromise.21 In light of these data, some experts have recommended retaining the cervical collar but transporting the patient on a gurney with a scoop stretcher22 or other soft, padded devices23 to avoid the rigid spine board. Some authors have even proposed abandoning the routine use of cervical collars.24 Nevertheless, in the absence of controlled data regarding the safety of such measures, current neurosurgery guidelines25 still recommend usage of the rigid cervical collar and long spine board. In contrast, spinal immobilization is no longer recommended for fully conscious, neurologically intact patients with isolated penetrating neck injury because collars can delay resuscitation and obscure neck injuries.26,27
INITIAL ED STABILIZATION
ED evaluation of the patient with potential spinal injury should not differ substantially from that of any patient with multiple injuries, with the first priority being the airway. The higher the level of spinal injury, the more likely is the need for early airway intervention. For example, unstable spine lesions above C3 can cause immediate respiratory arrest, and lesions affecting C3-C5 can affect the phrenic nerve and diaphragm function. For this reason, some experts recommend that any patient with an injury at C5 or above should have the airway secured by endotracheal intubation
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree