4 Spinal Injury Classification Systems F. C. Öner Different classification systems have been used in traumatology to stratify and categorize injuries. Most surgeons consider them necessary tools to provide a conceptual framework for diagnosis and treatment. Furthermore, these schemes are used as systems for communication about the relative severity of the injuries and the result of different treatment options. However, these schemes have been gradually introduced into the field without a proper discussion of their meanings and consequences. Although indispensable in modern clinical practice and academic discussions, a thorough understanding of the types of classifications and what they mean together with an understanding of their strengths and weaknesses is necessary for proper use of these important tools. Especially the advancements in diagnostic imaging and our increasing capacity to help severely injured patients survive make this an urgent task. A clinically relevant classification system not only should take into account the natural history of an injury pattern but also should predict outcome. Ideally, such a system should provide a universal language to describe spinal injuries and should guide clinical decision making. This system must be easy to remember and to use in clinical practice and should provide a platform for prospective research on spinal injuries. The system must be able to stratify injury severity and suggest the prognosis of a given injury.1 Table 4.1 Classification Systems
| Uses | • Stratify and categorize injuries |
| • Conceptual framework for diagnosis and treatment | |
| • Used as system of communication about severity of injury and result of different treatments | |
| Characteristics | • An account of the history of injury and prediction of outcomes |
| • Provide universal language describing injuries | |
| • Guide decision making | |
| • Must be easy to remember | |
| • Provide platform for prospective research | |
| • Must be able to distinguish severity and suggest prognosis | |
| Difficulties with spinal injury classification | • Spine fracture patterns may be progressive |
| • Spine fractures are structural injuries with different injury susceptibilities and different healing potentials | |
| • Approach mechanical and neurologic injury separately | |
| Requirement | • System must allow physician to assess three kinds of stability: |
| 1. Immediate mechanical | |
| 2. Neurologic | |
| 3. Long-term |
Classification of spinal injuries has been an exceptionally contentious subject (Table 4.1). Different schemes have been proposed, discussed, and criticized in an ongoing debate. Considering the complexity of the spine with its central role in the locomotor as well as the nervous system, it is no wonder that this discussion has at times been seen as intractable. The main difficulty lies in the fact that, unlike the fractures of long bones, the pattern of spine fractures may be progressive, evolving into an increasing deformity, and that the spine fractures represent complex injuries of a structure composed of parts with different susceptibility to injury and different healing potentials. Adding to the confusion, injury to the mechanical integrity of the spinal column and the neurologic injury have been approached separately. Stability has been a key concept, but it is usually poorly defined, and the term is used inconsistently. The most reliable and mentally reproducible concept of stability was described in the 1970s by White and Panjabi:2
Clinical instability is defined as a loss in the ability of the spine under physiologic loads to maintain relationships between vertebrae in such a way that there is neither damage nor subsequent irritation to the spinal cord or nerve roots. In addition there is no development of incapacitating deformity or pain due to structural changes.
This means that a useful classification system should enable the surgeon to make an educated guess about three kinds of stability:
- Immediate mechanical stability
- Neurologic stability
- Long-term stability
 Classification of Neurologic Injury
Classification of Neurologic Injury
Classification of the neurologic injury as a result of traumatic spinal conditions has been one of the fields where people can reach a consensus easily, but a lot of uncertainty remains due to the practical difficulties of conducting a thorough neurologic exam by trauma victims. In general, the neurologic syndromes associated with spinal cord or cauda equina are well defined, and a trained clinician can usually define the place and extent of pathology quite accurately as soon as a complete neurologic exam is possible (Table 4.2). In trauma patients, however, many factors, such as multiple injuries, and subdued consciousness levels as a result of brain injury, substance use, or emergency intubation, make it often impossible to carry out a reliable neurologic exam. It is generally accepted that a reliable neurologic status can be determined only after multiple neurologic exams within 48 to 72 hours of the injury. The treating surgeons should always keep this uncertainty in mind during their decisions on treatment. There is a big difference in the prognosis between complete and incomplete spinal cord injuries, and it is advisable not to declare a patient a total paraplegic unless one is absolutely sure.
The Frankel classification was the first universally used system to categorize the patients with neurologic injury according to their remaining useful function for rehabilitation. As a result, this was a rather coarse classification. The American Spinal Injury Association (ASIA) has refined this scheme and developed a system to determine sensory and motor levels separately and finally to reach an ASIA impairment scale3 (Fig. 4.1). Although the reproducibility of this scale has not been studied sufficiently, this scheme has found general acceptance and is recommended in every patient with spinal injury.
 Classification of Fractures
Classification of Fractures
All classification systems in traumatology are based on the assumption that the interaction between the chaotic forces causing the trauma and the human body would yield some recognizable, reproducible, and meaningful patterns of injury. Although the evidence for this basic assumption is frustratingly weak, practitioners generally accept that this approach has led to substantial improvement in trauma care and education. Many fracture classification schemes have been introduced for different anatomical areas of the spinal column. Traditionally two basic approaches to classification can be recognized: descriptive and mechanistic. Many of the schemes are a combination of these two basic approaches.
Anatomical Areas of the Spine
Although the basic anatomical plan of the spine is the same throughout the spinal column, very ancient and specific adaptations exist in the cranial and caudal extremities. Cranially, the occiput-C spine junction is formed by a special anatomical structure called the occipito-atlanto-axial complex. The most caudal section is formed by the fusion of the last five or six spinal segments into the sacrum, which is also a part of the pelvic ring. Besides these special forms in the extremities, the vertebrae of the cervical, thoracic, and lumbar spine show variations in the different parts of the basic plan and react differently to traumatic forces. Usually these regions are treated separately (Table 4.3).
Table 4.2 Neurologic Injury Classification
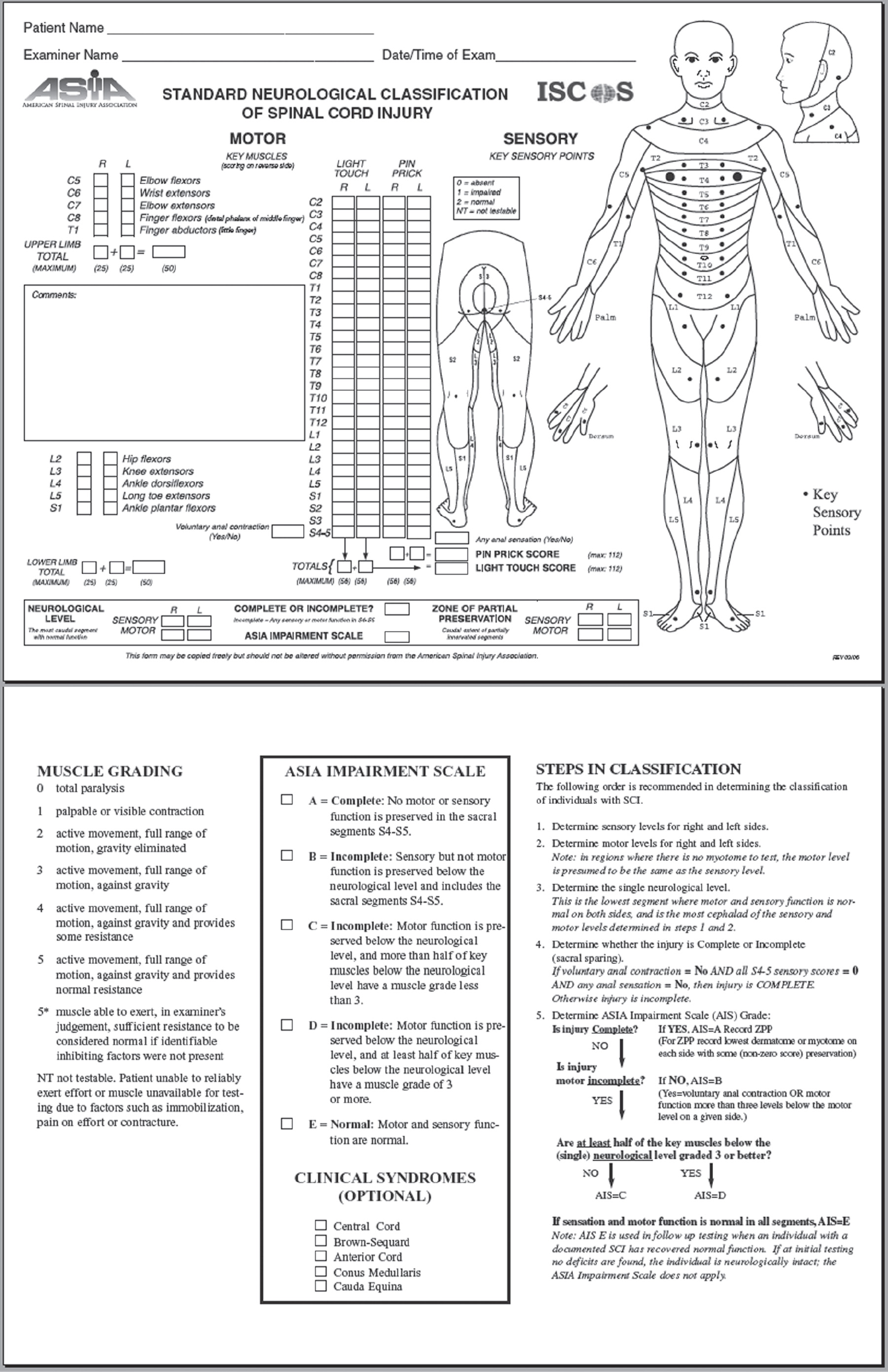
Fig. 4.1 Classification of neurologic injury according to the American Spinal Injury Association.
Table 4.3 Vertebral Regions Reacting Differently to Trauma Due to Structure
| Occipito-atlanto-axial junction | C0-C2 |
| Subaxial spine | C3-C6 |
| Cervicothoracic junction | C7-T3 |
| Thoracic spine | T4-T9 |
| Thoracolumbar junction | T10-L2 |
| Lumbar spine | L3-L5 |
| Sacrum |
Conventionally, separate systems have been used for the upper cervical, subaxial, thoracic, and lumbar and sacral fractures.
Upper Cervical Injuries and Fractures
The first two vertebrae have evolved into a radically different body plan to form a special structure, allowing the junction of the cranium with the cervical spine (Table 4.4). This special occipitocervical junction containing the occipital condyle-atlas and atlas-axis connection is capable of extreme rotation, especially between C1 and C2. This is achieved by the fusion of the central section of the body of C1 to C2 as the odontoid process, and the conversion of the rest of the intervertebral disk space into a special kind of a facet joint, allowing an orientation parallel to the base of the skull. This atlantoaxial complex is joined to the skull through occipital condyles and strong ligaments (Fig. 4.2). Although injuries are usually classified under condyle fractures, atlas fractures, and axis fractures, one should not forget that this is a strongly integrated complex, and injury to one part has consequences for the whole complex. The classification systems used for this complex are descriptive and not validated.
Occipitocervical Dislocations
These dislocations are uncommon injuries probably because of their fatal outcomes. Thanks to advanced trauma life support (ATLS), however, more patients survive these injuries and are diagnosed. They are more common in children because of their relatively bigger head size. In autopsy studies, they represent more than 10% of cervical injuries. A descriptive classification has been suggested, but its value is questionable because of the infrequency of reported cases. According to this classification, type I represents anterior, type II vertical, and type III posterior displacements. Also, a type IIA injury has been described where the vertical displacement takes place between C1 and C2.4
Occipital Condyle Fractures
Table 4.4 Upper Cervical Fractures and Occipitocervical Dislocations
| Structure | • Contains occipital condyle-atlas and atlas-axis connection capable of extreme rotation |
| Occipitocervical dislocation | • Uncommon due to high fidelity rate |
| • More common in children | |
| • Represent 10% of cervical injuries | |
| • Classification: | |
| 1. Type I: anterior dislocation | |
| 2. Type II: vertical dislocation | |
| 3. Type IIA: vertical between C1 and C2 | |
| 4. Type III: posterior dislocation |
The most commonly used classification is that of Anderson and Montesano from 1988, based on the description of only six cases (Fig. 4.3; Table 4.5). A type I fracture is a comminuted impaction fracture resulting from axial loading, whereas type II is a condylar fracture with extension into the base of the skull. Type III is an avulsion-type fracture at the insertion of the alar ligament. Accordingly, Anderson and Montesano suggested that only the type III would be considered unstable. Tuli et al proposed in 1997 a new system of classification, because of the difficulty in predicting stability simply by the displacement of the occipital condylar fracture without confirmation by other means, such as magnetic resonance imaging (MRI), to establish whether there was a ligament injury. In this system, type I fractures are undisplaced and stable, and type II fractures are divided into subtypes A and B. Type IIA is a displaced fracture of the occipital condyle with stability at the occiput-C1-C2 levels. In type IIB fractures, there is instability at the occiput-C1-C2 levels as demonstrated by radiography.5
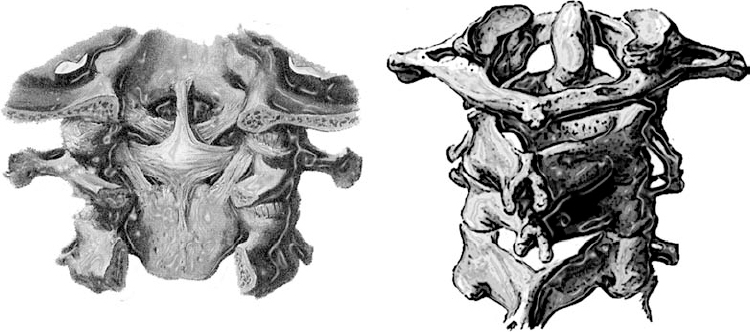
Fig. 4.2 The occipitocervical junction is formed by a special adaptation of the first two vertebrae and a strong network of ligaments.
Atlas (C1) Fractures
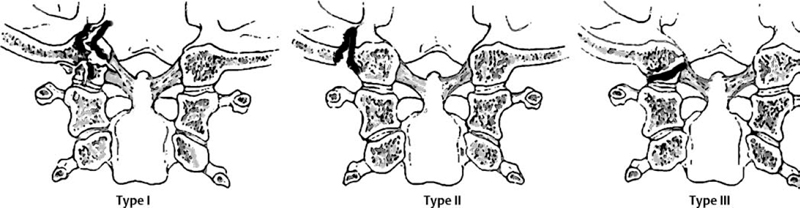
Fig. 4.3 Three basic types of condyle fractures.
Table 4.5 Occipital Condyle Fractures
| Anderson and Montesano classification | • Type I: comminuted impaction fracture resulting from axial loading |
| • Type II: condylar fracture with extension into base of skull | |
| • Type III: avulsion-type fracture at insertion of alar ligament; only one considered “unstable” | |
| Tuli et al classification | • Type I: fracture undisplaced and stable |
| • Type IIA: displaced fracture of occipital condyle with stability of the occiput-C1-C2 levels | |
| • Type IIB: instability at the occiput-C1-C2 levels demonstrated via radiography |
This is a relatively common injury constituting approximately 10% of cervical injuries (Table 4.6). In almost half of the cases they occur in combination with C2 fractures. Three common types are observed: posterior arch fractures, lateral mass fractures, and burst (Jefferson) fractures (Fig. 4.4). Theoretically, the integrity of the transverse ligament is crucial in the stability of the atlantoaxial complex.
Axis (C2) Fractures
Table 4.6 Fractures of Atlas and Axis
| Atlas (C1) | • Relatively common; approximately. 10% of cervical injuries |
| • Approximately 50% associated with C2 fractures | |
| • Three common types: | |
| 1. Posterior arch fractures | |
| 2. Lateral mass fractures | |
| 3. Burst (Jefferson) fractures | |
| • Integrity of transverse ligament crucial to stability | |
| Axis (C2) | • Anatomically vulnerable at two points: |
| 1. Odontoid process (dens): common fractures in osteoporotic spine | |
| 2. Isthmus: common spondylolisthesis of C2 (hangman’s fracture) | |
| Odontoid fracture | • 8 to 18% of cervical fractures |
| • Neurologic injury occurring in 10 to 20% of cases | |
| • Two peaks of incidence: | |
| 1. Childhood injury: hyperflexion | |
| 2. Elderly injury: hyperextension | |
| • Anderson and D’Alonzo classification system used: | |
| Type I: tip of dens; uncommon | |
| Type II: fracture at dens-axis junction; most common, with high rate of nonunion | |
| Type III: fracture through body of axis | |
| Hangman’s fracture | • Traumatic spondylolisthesis of axis |
| • Effendi classification used (modified by Levine and Edwards): | |
| Type 1: fracture through isthmus posterior to body; vertical fracture line | |
| Type 1A: “atypical hangman’s fracture”; fracture lines of left and right isthmus not parallel | |
| Type 2: significant angulation and more than 3 mm of translation; vertical fracture lines; caused by combination of hyperextension and axial loading, causing type 1 fracture, followed by flexion force | |
| Type 2A: uncommon; little or no translation but significant angulation; oblique fracture line, from anterior-inferior to posterior-superior; caused by flexion-distraction forces | |
| Type 3: multiple configurations: | |
| Type 1 fracture with bilateral dislocation of C2-C3 facet joints | |
| Unilateral facet dislocation and contralateral isthmus fracture |
Due to its special anatomy, the axis is exceptionally vulnerable at two points: the odontoid process and the isthmus. The odontoid process (dens) is the only vertebral body type (cancellous) structure in the spine, which must resist forces other than compression. This explains the high incidence of these fractures in the osteoporotic spine. Because the C1-C2 connection lacks a real facet joint, the C2 body is connected to the facet of C3 through an elongated pedicle-isthmus. The motion planes of the proximal and distal joints of C2 also make a sharp angle and have a considerable offset between them. The motion plane of C1-C2 joint is ventral, whereas the C2-C3 joint is dorsal to the spinal canal. This connection is further weakened by the vertebral artery penetrating the axis just at the base of the pedicles. This explains the common occurrence of the traumatic spondylolisthesis of the C2, which is also (erroneously) called the hangman’s fracture.
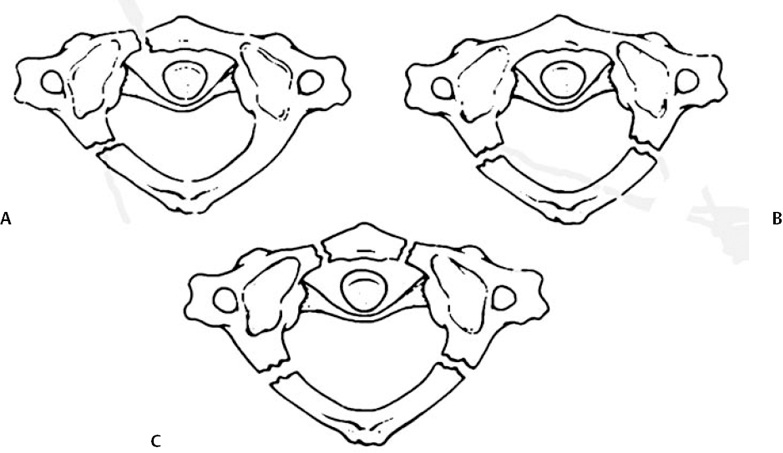
Fig. 4.4 The most common patterns of C1 fractures. (A) Lateral mass. (B) Posterior arch. (C) Burst (Jefferson).
Odontoid (Dens) Fractures
These fractures constitute 8 to 18% of the cervical fractures, with neurologic injuries occurring in 10 to 20% of the cases. There are two peaks of incidence with distinctive patterns: one in childhood injuries usually as a result of hyperflexion, and one in the elderly with hyperextension forces.6 The descriptive-anatomical classification of Anderson and D’Alonzo is the most commonly used system (Fig. 4.5):
- Type I: fractures at the tip of the dens. Although uncommon, they may be the result of an avulsion fracture of the alar ligaments as part of an occipitocervical dissociation.
- Type II: fractures occurring at the junction of the dens with the body of axis. These are the most common fractures and have a high rate of nonunion, especially if there is displacement or treatment delay.
- Type III: fractures through the body of axis.
Traumatic Spondylolisthesis of the Axis (Hangman’s Fracture)
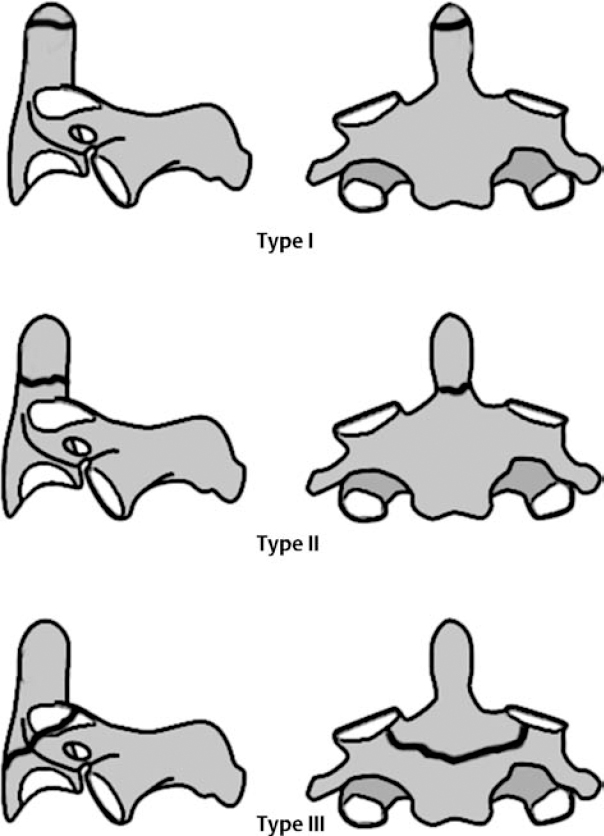
Fig. 4.5 The three basic types of odontoid fractures.
The most commonly used scheme is the Effendi classification modified by Levine and Edwards7 (Fig. 4.6). This scheme is based on the morphology, presumed mechanism of injury, and the measured amount of angulation and translation between C2 and C3:
- Type 1: the fracture is through the isthmus just posterior to the body, and the fracture line is predominantly vertical.
- Type 1A: also called “atypical hangman’s fracture.” The fracture lines of the left and right isthmus are not parallel; therefore, they may not be easily visible on radiograms.
- Type 2: these injuries show significant angulation and more than 3 mm of translation. The fracture lines are similar to type 1 and are predominantly vertical. It is generally believed that this type is caused by a combination of hyperextension and axial loading, leading to a type 1 injury followed by a flexion force. This flexion force in the presence of type 1 fracture causes the disruption of the disk where the anterior longitudinal ligament is stripped off together with a crushed anterosuperior corner of the C3 end plate.
- Type 2A: an uncommon but potentially confusing injury type. There is little or no translation but a significant angulation. The direction of the fracture line is oblique, running from anterior-inferior to posterior-superior. This injury is a result of flexion-distraction forces. The isthmus fails in tension as a result of hyperflexion forces, causing a rupture of the disk from posterior to anterior. There is no crushing of the C3 end plate, and the anterior longitudinal ligament (ALL) is intact.
- Type 3: may occur in several configurations. The most common form is a type 1 fracture in combination with bilateral dislocation of C2-C3 facet joints. Another potential pattern is a unilateral facet dislocation and contralateral isthmus fracture. The mechanism is unclear. It has been suggested that these result from a flexion injury causing the facet dislocation followed by a hyperextension force causing the fracture. The neural arch in this type of injury has become a free-floating fragment with disruption of the posterior ligamentary complex (PLC) between C2 and C3 as well as the bony connection to the body of the axis.

Fig. 4.6 Observed patterns of traumatic spondylolisthesis (hangman’s fracture) of C2.
Subaxial Cervical Injuries
Table 4.7 Subaxial Cervical Injuries
| Injury type | • Vary from minor sprain (“whiplash”) to fracture dislocations |
| • Anatomically predisposed highly unstable injury patterns | |
| Characteristics | • Common |
| • Approximately 55% of traumatic spinal cord injuries | |
| Allen and Ferguson classification | • Six phylogenies (according to inferred mode of failure): |
| 1. Flexion-compression | |
| 2. Vertical compression | |
| 3. Flexion-distraction | |
| 4. Extension-compression | |
| 5. Extension-distraction | |
| 6. Lateral flexion |
Due to the relatively big size of the human head and frequent human activities leading to acceleration-deceleration forces, these are common injuries varying from minor sprains (whiplash) to major fracture dislocations (Table 4.7).8 The anatomical adaptations in the C-spine allowing the highest degree of motion of the whole spinal column also predisposes it to highly unstable injury patterns. Cervical spine injuries are responsible for more than 55% of traumatic spinal cord injuries. Many of the concepts developed for the classification of thoracolumbar injuries have also been applied with modifications to the cervical spine.9 For a discussion of these concepts, see Thoracic and Lumbar Spine Fractures (next subsection). The most commonly used system in the C-spine is the mechanistic classification proposed by Ferguson and Allen.10 In this scheme the injuries are grouped into six phylogenies according to the inferred mode of failure of the C-spine:
- Flexion-compression
- Vertical compression
- Flexion-distraction
- Extension-compression
- Extension-distraction
- Lateral flexion
Within each phylogeny there is a series of stages based on the severity of anatomical disruption. This system is a highly complex combination of mechanistic classification at the phylogeny level and anatomical-descriptive categorization at the subphylogeny level. Because of its complexity, this scheme has not been used extensively in clinical practice, and no studies have been conducted on the validity and reproducibility of this scheme. More recent classification proposals are discussed later (see The Concept of Injury Severity Scores).
Thoracic and Lumbar Spine Fractures
Table 4.8 Thoracic and Lumbar Spine Fractures
| Böhler classification | • Based on five injury types: |
| 1. Compression fractures | |
| 2. Flexion-distraction injuries | |
| 3. Extension fractures | |
| 4. Shear fractures | |
| 5. Torsion injuries | |
| Watson-Jones and Nicoll classification | • Developed this scheme further by introducing concept of “instability” and the crucial role of ligamentous structures: |
| 1. Wedge compression fractures | |
| 2. Comminuted fractures | |
| 3. Fracture dislocations | |
| Holdsworth classification | • Abstracts the vertebral stability with an architectonic concept of two columns: |
| 1. Anterior column: vertebral body, intervertebral disks, and anterior and posterior ligaments | |
| 2. Posterior column: facet joints, laminae, and posterior ligaments | |
| • First to describe burst fracture as separate entity | |
| Kelly and Whitesides classification | • Further developed Holdsworth system: |
| 1. Anterior column: vertebral bodies | |
| 2. Posterior column: neural arches | |
| Roy-Camille classification | • Emphasized role of “segment moyen” (middle segment) |
| Louis classification | • Introduced three-column architecture: |
| 1. Anterior: vertebral bodies and disks | |
| 2 & 3. Posterior: facet joints, articular process, and isthmus | |
| • Three columns connected by tree arches: | |
| 1. Neural arch: two posteriors | |
| 2. Two pedicles: posterior with anterior | |
| • Quantified instability: (instability = score of 2 or more) | |
| 1. Each column = 1.0 point | |
| 2. Arches = 0.5 point | |
| 3. Other elements = 0.25 point |
There has been a great deal of controversy about the classification of fractures of the thoracolumbar spine since the first attempts by Böhler in 19291 (Table 4.8). Böhler’s descriptive scheme based on radiographic images identified five injury types:
- Compression fractures
- Flexion-distraction injuries
- Extension fractures
- Shear fractures
- Torsion injuries
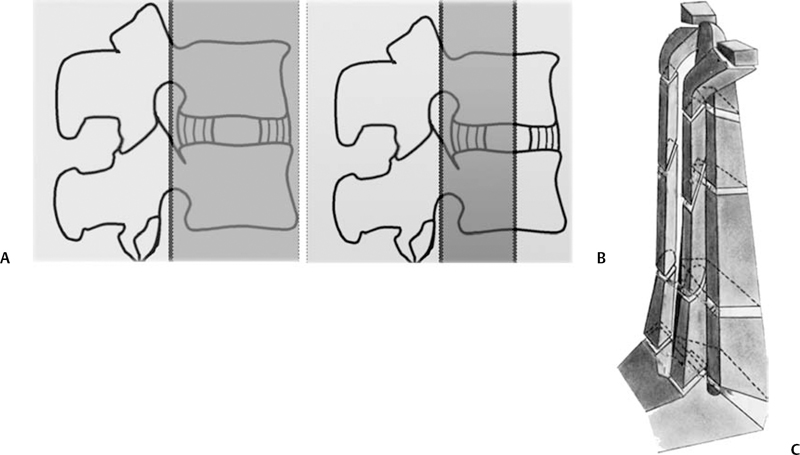
Watson-Jones and Nicoll further popularized and developed this descriptive scheme. Watson-Jones was the first who introduced the concept of instability and recognized the importance of ligamentary injuries for the mechanical stability of the spinal column. Based on three predominant injury categories-wedge compression fractures, comminuted fractures, and fracture-dislocations-he tried to define instability patterns so that the classification can be used as a predictive tool and a guide for treatment. Holdsworth tried to capture the problem of stability in a columnar spine concept in the 1960s. He tried to abstract the vertebral stability with an architectonic concept of two columns: (1) anterior column, consisting of the vertebral body, the intervertebral disks, and the anterior and posterior ligaments; and (2) posterior column, consisting of the facet joints, laminae, and posterior ligaments. This abstraction has been influential not only in the thoracolumbar but also in the cervical spine pathologies ever since (Fig. 4.7). Holdsworth was also the first author to describe the burst fracture as a separate entity. The columnar spine concept of Holdsworth was further developed by Kelly and Whitesides, with the anterior column represented by the vertebral bodies and the posterior column by the neural arches. Roy-Camille in the 1970s emphasized in that context the role of what he called the “segment moyen” (middle segment) formed by the posterior part of the disk, anulus fibrosus, and posterior longitudinal ligament, together with the pedicles and the facet joints. Louis tried to elaborate the spinal columns concept with the introduction of a three-column architecture of the spine. One column is the anterior, composed of the vertebral bodies and the disks; the other two columns are posterior, consisting of the facet joints, articular processes, and isthmus. These three columns are connected by three arches: the neural arch connecting the two posterior columns and the two pedicles connecting the posterior columns with the anterior column. Louis tried to quantify instability with this structure. Each column counts as 1, the arches as 1/2, and the other elements as 1/4. Instability is defined by a total score of 2 or more. Louis believed that this basic structure was maintained along the vertical column system, consisting of two columns at C1-C2 and three columns from C2 to the sacrum.