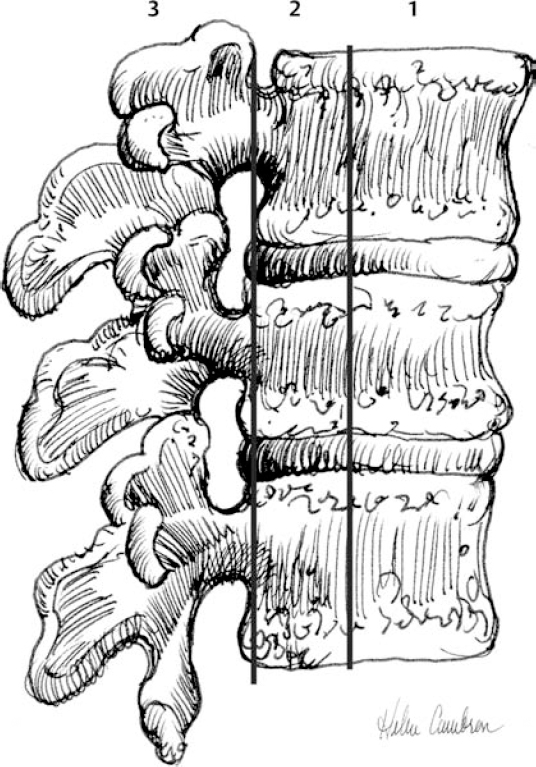
10 Classification, Diagnosis, and Management of Thoracolumbar Spinal Injuries Steven C. Zeiller, Eli M. Baron, Neel Anand, Alan S. Hilibrand, and Alexander R. Vaccaro The diagnosis and treatment of patients with thoracolumbar spine fractures has evolved over the last two decades. Advances have been made in the transportation of these patients from the field, as well as in imaging of the spine, diagnosis, classification, and nonoperative and operative techniques. At the same time, significant controversy has persisted regarding the most appropriate treatment of the most common of these fractures, the thoracolumbar burst fracture. However, regardless of the type of intervention employed, the fundamental principles that govern treatment include restoration of the mechanical stability of the spine with correction of deformity and protection of the neural elements. These principles apply whether the patient undergoes nonoperative or operative intervention. This chapter reviews the critical factors that apply to the evaluation of patients with thoracolumbar fractures and discusses the management of these injuries. Thoracolumbar fractures can result from a variety of different mechanisms acting on the spine. The most common is an axial load combined with varying degrees of flexion resulting in a burst fracture. Motor vehicle accidents are the source of the vast majority of these injuries.1 Other common etiologies include falls from a height, sports injuries, and penetrating trauma. This type of injury is most commonly seen in young males between the ages of 15 and 29.2,3 The geriatric population also is affected, due to the high incidence of osteoporosis among the elderly. Burst fractures in the elderly population are increasing, and they usually result from low-energy trauma. Thoracolumbar fractures in the osteoporotic spine present their own unique challenges with regard to treatment. Bracing is typically poorly tolerated in the elderly population. Additionally, surgical stabilization in patients with osteoporotic bone presents its own challenges due to limited internal fixation stability. The thoracolumbar spine is particularly vulnerable to traumatic injury due to its unique anatomy. The thoracolumbar junction serves as the transition between the more rigid, less mobile kyphotic thoracic spine and the less rigid, more mobile lordotic lumbar spine. The thoracic spine has narrow disk spaces and coronally oriented facets, which limit motion, especially in the sagittal plane. Additional stability is provided by the ribs articulating with the spine and sternum. By comparison, the lumbar spine has larger disks with sagittally oriented facets, which promote mobility of the spine in flexion and extension. Consequently, high-energy injuries are transmitted through the thoracic spine and dissipated at the thoracolumbar junction, resulting in characteristic fracture types. There have been several classification systems for thoracolumbar fractures proposed over the last several decades. The classification systems to date have been a variety of morphologic, anatomical, and mechanistic descriptions of the identified injury. The primary objective of most of these classification systems was to define a specific fracture pattern that would prognostically identify the stability of the spinal column. However, the definition of “clinical instability” has remained a source of controversy regarding the treatment of these patients. One of the earlier classification systems proposed was by Nicoll4 in 1949. Nicoll studied 166 fractures and fracture-dislocations in a population of 152 coal miners. The most common mechanism was compression with varying degrees of flexion. Stability in the neurologically intact patients was based on the integrity of the posterior ligamentous complex (PLC). Patients without a PLC injury (stable group) received functional treatment, which consisted of bed rest for 3 to 4 weeks until the patient could participate in physical therapy. In the unstable patients with PLC injury, treatment consisted of casting with prolonged bed rest until bony consolidation was complete. In terms of the work capacity in the group treated with casting, 27% returned to the coal face, 10% performed light work underground, and 63% performed light work on the surface. In the group treated “functionally,” 55% returned to the coal face, 27% performed light work underground, and 18% performed light work on the surface. Anatomical classification systems that divide the spine into columns were first popularized by Holdsworth’s5 “two column” theory in 1963. Holdsworth defined the anterior and posterior columns of bone and soft tissue based on their location relative to the neural elements. The anterior column included the vertebral body and disks as well as the anterior longitudinal ligament (ALL) and the posterior longitudinal ligament (PLL). The posterior column consisted of the posterior elements and the PLC. This was later modified by Denis6 some 20 years later with the advent of cross-sectional imaging. Denis divided the spine into three columns, introducing the middle column. According to Denis’s system, the anterior column consisted of the ALL and the anterior half of the vertebral body. He defined a third, “middle” column, consisting of the posterior half of the vertebral body, the annulus, and the PLL. As per Holdsworth’s classification system, the posterior column consisted of the posterior spinal elements. The key factor that Denis proposed that contradicted Holdsworth’s theory was that isolated rupture of the posterior column was insufficient to establish instability. Injury to the PLL and posterior annulus was necessary to impart instability of the spinal column. As a result, Denis proposed that spinal instability required disruption of at least two of the three columns. This classification system has arguably been the most popular system employed by North American spine surgeons to date. Denis6 identified four types of fractures based on the three-column theory (Fig. 10.1): compression fractures, which consist of compression failure of the anterior column; burst fractures involving both anterior and middle columns; seat belt injuries, which consist of distraction failure of the posterior and middle columns; and fracture dislocations involving all three columns. Within Denis’s classification system, four types of fractures (and more than 20 subtypes) were described. Denis also described varying degrees of instability, including first degree, which was mechanical instability with a possibility of progressive deformity developing; second degree or neurologic instability, in which an injury may predispose to neurologic compromise; and third degree, which included combined mechanical and neurologic disability. Denis’s classification was closely followed by the classification system of McAfee et al,7 which divided thoracolumbar fractures into six types based on examination of the computed tomography (CT) scans of 100 patients (Table 10.1 and Fig. 10.2). In the McAfee system, the status of the middle column was most important for subclassification. The six subtypes were as follows: (1) wedge compression fracture (an isolated anterior column injury); (2) stable burst fracture (an injury to both the anterior and middle columns but not to the posterior column); (3) unstable burst fracture (compression injury to the anterior and middle column as well as injury to the posterior ligamentous complex); (4) flexion-distraction injury (compression injury to the anterior column, tension injury of the middle column, and tension injury of the posterior column, where the mechanism of injury involved an anterior column fulcrum); (5) Chance-type fracture, where the anterior, middle, and posterior columns were all disrupted in tension via a flexion fulcrum anterior to the vertebral column, which differed from a flexion distraction injury, where the anterior column was disrupted via compression; and (6) translational injury, where shear forces were responsible for disruption of all three columns. Fig. 10.1 Illustration of the Denis three-column theory. The anterior column includes the anterior longitudinal ligament, anulus fi-brosus, and anterior one third of the vertebral body. The middle column includes the posterior two thirds of the vertebral body, posterior longitudinal ligament, and posterior anulus fibrosus. The posterior column includes the lamina, spinous processes, and all posterior elements in addition to the posterior ligamentous complex. (Courtesy of Helen Cambron, RN.) McCormack et al8 subsequently devised a scoring mechanism that assisted in determining the need for adjunctive anterior column support following posterior short segment fixation of surgically treated thoracolumbar burst fractures. This scoring system addressed whether thoracolumbar fractures treated posteriorly alone via short segment fixation would be successfully treated in the long term or go on to instrumentation failure and spinal kyphosis. The scale consisted of three components: an assessment of the degree of fracture comminution, the degree of fracture fragment displacement, and the degree of required kyphosis correction. Table 10.1 McAfee Classification System of Thoracolumbar Fractures
 Etiology
Etiology
 Classification Systems
Classification Systems
| Wedge compression fracture | Isolated compression deformity of anterior vertebral body |
| Stable burst fracture | An isolated injury of anterior and posterior vertebral body |
| Unstable burst fracture | Injury to both anterior and posterior vertebral body but also to posterior elements |
| Flexion distraction injury | Anterior column compression, middle and posterior vertebral column disrupted in tension (anterior vertebral body served as a fulcrum for injury) |
| Chance-type fracture | Anterior and posterior vertebral body disrupted in tension, posterior elements disrupted in tension; the fulcrum here is anterior to the spinal column |
| Translational injury | Shear injury where all three columns of the spine are disrupted |
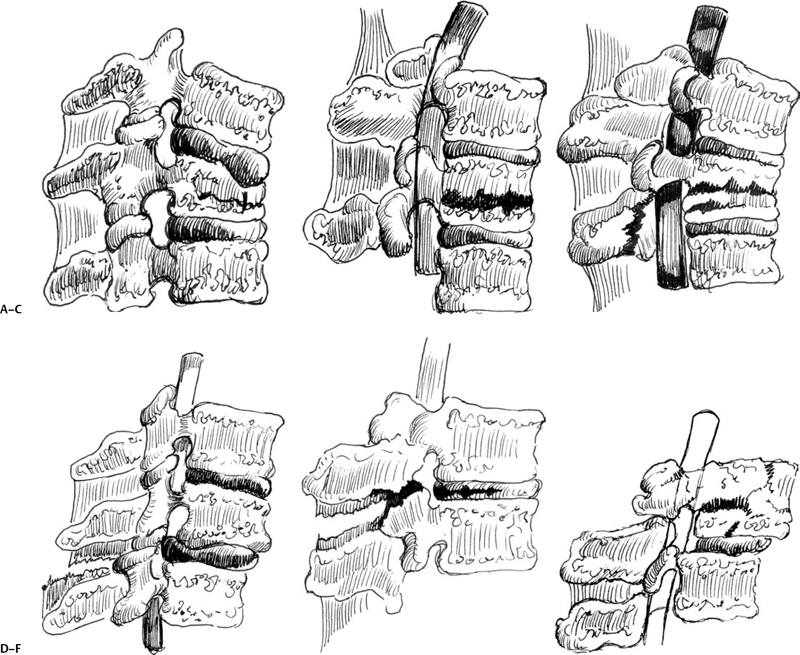
Fig. 10.2 McAfee classification system identifying six subtypes of fractures: (A) wedge compression fracture, (B) stable burst fracture, (C) unstable burst fracture, (D) flexion-distraction injury, (E) Chance fracture, and (F) translational injury. (Courtesy of Helen Cambron, RN.)
Magerl et al9 proposed the Arbeitsgemeinschaft für Osteosynthesefragen (Association for the Study of Internal Fixation) (AO) classification system in 1994. This system was comprehensive in nature and employed both mechanistic and morphologic characteristics. The major categories of the system were based on the mechanism of injury (compression, distraction, translation). Within each major grouping, fracture subtypes were further categorized. This system is excellent for research purposes because it accounts for every fracture permutation, but due to its cumbersome nature (accounting for more than fracture subtypes), it has not been widely used clinically.
More recently, Vaccaro et al10,11 proposed the Thoracolumbar Injury Classification and Injury Severity Score (TLICS). This system assesses three primary variables that dictate treatment of patients with thoracolumbar spine fractures: the morphology of the injury, the neurologic status of the patient, and the integrity of the PLC. Points in the scoring system are then assigned for each of the primary variables and their subtypes, creating a point total, the TLICS (Table 10.2). The total score is then used to dictate treatment based on a point scale. Injuries with 3 points or less are treated nonoperatively, whereas injuries with 5 points or more are treated operatively. Patients with 4 points may be treated in either fashion, based on other clinical parameters. To effectively use this scoring system, a few guidelines need to be followed. First, if there are multiple fractures present, the most severe injury is the only one that is scored. Fractures occurring at different spinal levels are not to be added together to determine the injury severity score. Second, only the morphology with the greatest point value is used. For instance, if a patient had a burst injury (2 points for the burst component) and a translational injury (3 points), only the points for translation would be counted because it has a higher value. The key to this system is that it provides a systematic approach to evaluate patients with thoracolumbar fractures using clinically relevant information.
Table 10.2 Thoracolumbar Injury Classification and Severity Score (TLICS) System
| Score is total of three components: injury morphology, neurologic status, and posterior ligamentary complex (PLC) disruption; a score of 3 or below suggests nonoperative treatment, 4 suggests operative or nonoperative treatment, and 5 or above suggests operative treatment. | ||
| 1. Description | Points | |
| a. Compression fracture | 1 | |
| b. Burst fracture | 2 | |
| c. Translational/rotational | 3 | |
| d. Distraction | 4 | |
| 2. PLC | Points | |
| a. Intact | 0 | |
| b. Suspected/indeterminate | 2 | |
| c. Injured | 3 | |
| 3. Neurologic Status | ||
| Involvement | Qualifier | Points |
| 0 | ||
| Nerve root | 2 | |
| Cord, conus medullaris | Incomplete | 3 |
| Complete | 2 | |
| Cauda equina | 3 | |
Source: Adapted from Lee JY, Vaccaro AR, Lim MR, et al. Thoracolumbar injury classification and severity score: a new paradigm for the treatment of thoracolumbar spine trauma. J Orthop Sci 2005;10(6):671–675.
 Patient Evaluation
Patient Evaluation
Initial Evaluation
Traumatized patients who have a sufficient mechanism should be treated as if they have a spinal fracture until proven otherwise. The patient should be collected in the field and transported while maintaining full spine precautions (use of cervical collar, log rolling, and transportation on a spine board). During the initial phase of the work-up in the emergency room, the patient should be managed according to the advanced trauma life support protocol. Once the patient’s airway and hemodynamics have been stabilized, a more detailed examination can be performed. In the lucid patient a thorough neurologic examination (motor, sensory, rectal) can be performed. In addition, the spinal column can be palpated for pain and deformity. A detailed neurologic examination is crucial because the detection of a spinal cord injury or root injury (cauda equina) can have a major impact on the type and timing of the treatment of the patient. The neurologic status of the patient is one of the most important factors in determining whether the patient requires nonoperative or operative treatment. During the initial phase of the work-up of patients with suspected spinal trauma, it is important to keep track of how long the patient has been on the spine board. The patient should be taken off the board as soon as it is safe to do so, to ensure that there is no skin breakdown.
Radiographic Evaluation
The radiographic work-up of a patient suspected of having a spinal fracture typically begins with plain radiographs taken in the anteroposterior (AP) and lateral planes. The AP and lateral radiographs should be inspected for characteristic findings consistent with fractures in this region, including widened interpedicular distance and loss of vertebral body height. It is also critical to scrutinize the plain radiographs for evidence of any interspinous widening, thus implying a distraction mechanism. The fracture pattern should be analyzed to determine the morphology of injury (e.g., compression, distraction, translation). The determination of the fracture pattern provides a key piece of information regarding the amount of energy that caused the fracture and the resulting potential for instability. This also helps to stratify the patient with regard to treatment. Once a fracture is identified in the spinal column, it is mandatory to radiographically rule out contiguous and noncontiguous spinal fractures.
Plain films provide not only a useful method for screening for spinal fractures but also an assessment of both coronal and sagittal deformity in patients who have sustained thoracolumbar fractures. Traditionally, the kyphotic deformity that has warranted surgery was based on information obtained with the patient in the supine position with the spine in an unloaded position. Recently, the use of weight-bearing films in the subacute setting has been evaluated to see if they would alter management due to increased deformity in the loaded position. Mehta et al12 performed a prospective study evaluating the use of weight-bearing films in patients with thoracolumbar fractures to see if they influenced management. Twenty-eight patients without neurologic deficits were evaluated. The mean Cobb angle in the supine position was 11 degrees, which increased to a mean of 18 degrees on weight-bearing films (either sitting or standing). The mean anterior vertebral body height compression changed from 36 to 46% when taken with the patient in the supine position and in the weight-bearing position, respectively. The authors of this study operated on patients with vertebral body collapse of 50% or more, the presence of a neurologic deficit or fracture-dislocation, or kyphosis of > 20 degrees. Based on their findings with regard to vertebral body collapse and kyphotic angle found on weight-bearing films, seven patients underwent operative stabilization who were initially going to be treated conservatively based on supine measurements. The authors concluded that in some patients a weight-bearing film might demonstrate a more significant injury that may have been missed using only supine plain film surveillance.
Computed tomography has played an integral role in the diagnostic work-up of patients with thoracolumbar fractures. The images generated in the axial plane when combined with the sagittal and coronal reconstructions allow the surgeon to clearly identify the fracture pattern. There are several factors that should be evaluated on CT images. First, is there disruption of the posterior vertebral body with retropulsed bone into the canal? This is the fundamental difference between a “compression” fracture, which rarely requires operative management, and a “burst” fracture, which is more likely to be associated with instability and a neurologic deficit. Second, is there a fracture of the lamina at these levels? If so, a posterior approach to address nerve root entrapment may be needed. In addition, if operative treatment is indicated, the axial images provide information to allow the surgeon to determine if uninjured levels can accommodate pedicular fixation. Finally, the facet joints should be evaluated for any signs of subluxation suggesting a possible capsular or PLC injury. Injury to the PLC is an important finding because loss of this tension band places the patient at risk for developing a kyphotic deformity.
The use of CT in the polytraumatized patient as a screening tool has been studied. Hauser et al13 evaluated 221 consecutive patients sustaining high-risk trauma that warranted plain films of the thoracolumbar spine. The accuracy of plain radiographs in diagnosing an injury was compared with CT of the chest, abdomen, and pelvis. The accuracy of CT for fractures in the thoracolumbar spine was 99% compared with 87% for plain films. Another important finding in the study was the time to spinal clearance. CT examination as a screening tool to clear the thoracolumbar spine took on average approximately 1 hour compared with 295 minutes for plain radiographs. Brandt et al14 hypothesized that the data acquired from the thoracic and abdominal CT images were sufficient to screen for spinal fractures. They evaluated 207 polytraumatized patients in a retrospective fashion; 24% of patients had a spinal fracture on CT not recognized on plain films. Most of the missed fractures were transverse process fractures. The authors reported the average time required to perform a CT of the chest, abdomen, and pelvis was 55 minutes ± 32 minutes compared with 113 minutes ± 113 minutes for plain film screening for spinal fracture. The authors also noted that if only CT of the chest, abdomen, and pelvis had been ordered to screen for thoracolumbar fracture as opposed to plain films and a dedicated spinal CT, the cost savings would have been over $800 per patient.
The role of magnetic resonance imaging (MRI) in the evaluation of patients with thoracolumbar trauma is evolving. Although many clinicians reserve this imaging modality for patients with neurologic injury, valuable information can be obtained with regard to neural compression and edema patterns in both bony and soft tissue structures. Probably one of the most important roles in MRI is in evaluating the integrity of the PLC. Edema, denoted by hyperintensity of the posterior ligamentous structures on fat-suppressed T2-weighted images, is highly suggestive of a PLC injury (Fig. 10.3).
Lee et al15 prospectively evaluated 34 patients with thoracolumbar fractures with MRI to compare its sensitivity, specificity, and reliability with physical examination, plain radiographs, and intraoperative findings when evaluating the integrity of the PLC. The sensitivity of detecting a PLC injury on physical examination (palpation of the spine) was 52.0%, specificity was 66.7%, and accuracy was 53.6%. The sensitivity, specificity, and accuracy of plain films were 66.7%. The sensitivity of MRI in evaluation of the supraspinous ligament was 92.9%, specificity was 80.0%, and accuracy was 90.9%. The sensitivity of MRI in evaluation of the interspinous ligament was 100%, specificity was 75%, and accuracy was 97%. The authors found a statistically significant relationship between MRI and intraoperative findings. The authors concluded that a fat-suppressed T2 was a highly sensitive, specific, and accurate method of evaluating the integrity of the PLC.





