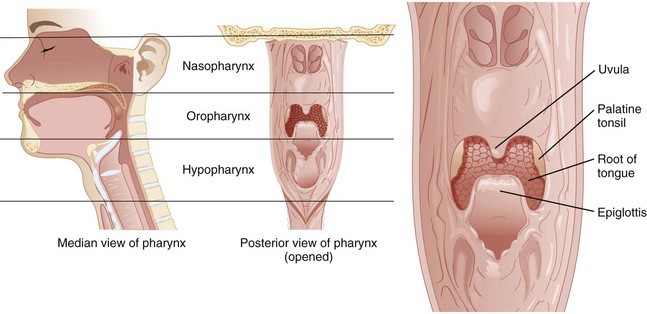
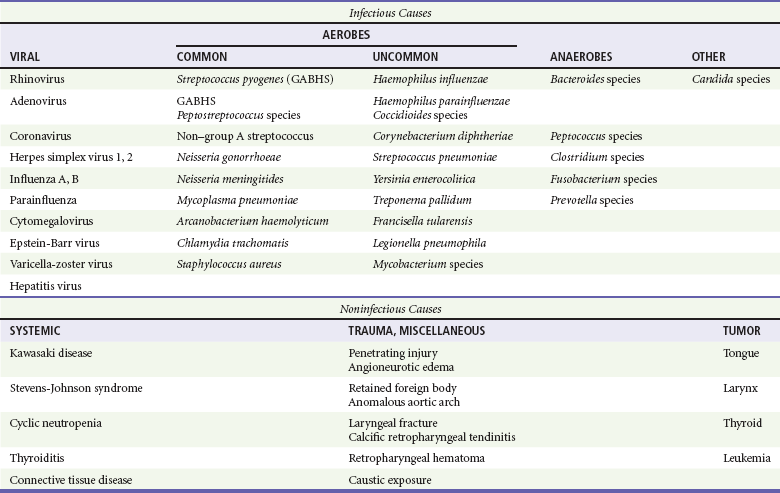
Chapter 23 In 2007 the National Hospital Ambulatory Medical Care Survey reported more than 2 million emergency department visits for sore throat and “throat-related” complaints.1 Thus sore throat remains among the most common presenting complaints in both emergency departments and outpatient care settings in the United States.1,2 Although some subtypes of pharyngitis and peripharyngeal disorders are more common in children and adolescents, individuals of all ages commonly develop sore throat. Sore throat, or pharyngitis, is generally caused by inflammation in the soft tissue of the pharynx. There are three anatomically distinct regions of the pharynx: the nasopharynx, oropharynx, and hypopharynx (Fig. 23-1). Pathology involving one site usually involves the others, but inflammation at any of these levels can manifest as a sore throat. The nasopharynx encompasses the area superior to the oral cavity, between the base of the skull and the soft palate. The eustachian tubes, connecting the middle ear and pharynx, open into this space. The oropharynx is the region directly visible on examination, lying behind the oral cavity, between the uvula and hyoid, including the vallecula and epiglottis. Laterally, it is defined by the tonsillar pillars. The hypopharynx is the most caudal aspect of the pharynx. It lies inferior to the epiglottis and terminates where the aerodigestive paths become distinct, at the esophagus and larynx; the vocal cords define the inferior pole. If one looks directly at a patient, this region is posterior and slightly superior to the thyroid cartilage. There are several important potential spaces surrounding the pharynx; disease in the retropharyngeal and submandibular spaces can manifest as not only pain but airway compromise. Airway Assessment and General Appearance The evaluation of sore throat begins with a simultaneous assessment of the airway and the patient’s general appearance. A history of rapidly progressive symptoms, difficulty breathing, or a sensation of tightness in the throat suggests potential threats to the airway. Examination begins with direct observation. Patients with airway compromise often sit upright or lean forward, with the neck extended and jaw thrust forward, and appear restless and distressed. Drooling may indicate an inability to swallow oral secretions and thus inflammation or pathology in the oropharynx or hypopharynx. Drooling is a sign of an advanced airway process, requiring prompt preparation for detailed evaluation and intervention. Presence of a muffled voice prompts consideration of a supraglottic threat to airway patency. The floor of the mouth should be visualized, and the submental region palpated as “brawny” induration or tenderness in this area is classically associated with Ludwig’s angina (Table 23-1). Stridor, a high-pitched noise heard on inspiration, indicates a process involving the glottic or infraglottic structures. Stridor indicates a true airway emergency, except when occurring in young children (<10 years old) with croup (see Chapter 168). Stridor is associated with ominous conditions such as epiglottitis, retropharyngeal abscess, and angioedema, and the severity and rate of onset and progression of symptoms indicates the urgency of the required intervention. General appearance is assessed with attention to hydration status and markers of systemic toxicity. Patients, particularly children, with significant pain from uncomplicated pharyngitis often have difficulty with oral intake and may become dehydrated. Fever and mild tachycardia are common vital sign derangements in those with viral or bacterial pharyngitis and do not typically indicate dangerous pathology. A prolonged fever (greater than 5-7 days) in children may be associated with Kawasaki disease.3 In the context of acute uncomplicated pharyngitis, considerable attention has been focused on differentiating between bacterial and viral infection through either bedside testing or clinical scoring. Various scoring systems, the most famous of which is the Centor criteria system, incorporate components of the history and physical examination to generate an estimate of group A streptococcus (GAS) infection.4 The four Centor criteria are history of fever, tonsillar exudates, tender anterior cervical adenopathy, and absence of cough. In a large prospective study including both children and adults that evaluated a modified Centor score (if age was greater than 45 years, 1 point subtracted), the prevalence of GAS increased with the number of criteria present. The prevalence of GAS was 1% with a score of −1 to 0, 10% with a score of 1, 17% with a score of 2, 35% with a score of 3, and 51% when the score was 4 or more. The distinction between viral and bacterial disease is, however, largely academic. With increasing emphasis on symptomatic relief and decreasing emphasis on eradication of the infecting agent, treatment, prognosis, and follow-up are virtually identical regardless of microbiologic cause5 (see Chapter 72). Although most patients with a sore throat have an uncomplicated infectious pharyngitis, certain components of the history are suggestive of more unusual pathology. Patients with human immunodeficiency virus (HIV) are at risk for oral candidiasis or thrush. In addition, primary HIV infection can manifest with upper respiratory infection (URI)–like symptoms, including acute pharyngitis in up to 75% of cases.6 Angiotensin-converting enzyme inhibitors predispose patients to angioedema, and although the lips and face are often visibly edematous, the process can be limited to the tongue, oropharynx, or hypopharynx. Nonimmunized children are at risk for epiglottitis and severe, life-threatening infections caused by Corynebacterium diphtheriae, and adults may have epiglottitis regardless of immunization status. Dental procedures, particularly involving the lower third molars, can be complicated by postoperative infections, the most potentially serious of which is Ludwig’s angina. Recent orogenital contact should broaden the differential diagnosis, as gonococcus and herpes simplex virus (HSV) can be pathogens in the pharynx. Pharyngitis in teenagers or young adults with significant cervical lymphadenopathy and fatigue suggests infectious mononucleosis caused by the Epstein-Barr virus. In one large case series of patients with head and neck cancers, hoarseness and sore throat were the two most common presenting complaints. In older patients, particularly men with a history of smoking, neoplastic causes should be considered.7
Sore Throat
Perspective
Pathophysiology
Diagnostic Approach
Viral versus Bacterial Pharyngitis
Special Considerations on History
![]()
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree