Chapter 106
Sleep Deprivation and Sleepiness in Medical Housestaff and Appropriate Countermeasures
Characteristics of Normal Sleep
By contrast, the typical sleep pattern of a resident on call is characterized by frequent sleep interruptions because of calls regarding patient care. Overall sleep time is reduced, with disproportionately greater time spent in stage N1 and less in stages N3 and REM sleep. A delayed sleep onset time and early rise time also disproportionately reduce REM sleep. This fragmented, REM-deprived sleep pattern can lead to significant deficits in memory acquisition and performance of newly learned tasks.
Determinants of Alertness
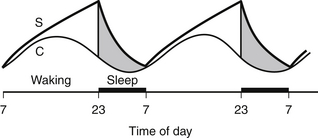
An individual’s level of alertness waxes and wanes throughout a 24-hour period. The greater the number of hours an individual spends awake, the greater the tendency toward sleepiness (Figure 106.1). This “sleep pressure,” which dissipates after sleep, is known as the homeostatic “Process S.” Process S is simultaneously counterbalanced by the circadian process, or Process C, which is driven by an internal clock residing in the suprachiasmatic nucleus. This wake-promoting internal clock operates with a periodicity of about 24.2 hours. A small circadian dip in alertness occurs in the late afternoon, and a larger nadir occurs at night, when the clock withdraws its wake-promoting signal. Because both Processes C and S favor sleepiness in the later evening and overnight, humans typically spend these hours sleeping.
Sleep-Related Determinants of Performance
Four characteristics of sleep determine performance: (1) nightly sleep duration; (2) number of hours awake; (3) perturbation of the circadian phase, as occurs when an individual works nightshifts, and (4) sleep inertia. The third correlates with a misalignment of Processes C and S, as mentioned previously. Sleep inertia refers to the decrement in performance in the first 15 to 30 minutes after waking, with impairments observed in short-term memory, counting, cognitive processing speed, and number fact and lexical retrieval. These skills are critical for ICU residents, who may be awakened for emergencies and asked to synthesize, sort, and integrate voluminous data and deliver urgent decisions. Sleep inertia increases with the depth of sleep that precedes waking; hence, longer naps lead to sleep inertia more often than shorter ones.
< div class='tao-gold-member'>