CHAPTER 57
Sialolithiasis
(Salivary Duct Stones)
Presentation
Patients of any age may develop salivary duct stones, although they are more common in men of age 30 to 60 years and less common in children. Most salivary stones occur in the Wharton duct from the submandibular gland. The patient is alarmed by the rapid swelling that suddenly appears beneath his jaw while he is eating. The swelling may be painful but is not hot or red and usually subsides within 2 hours. This swelling may only be intermittent and may not occur with every meal. Infection can occur and will be accompanied by increased pain, exquisite tenderness, erythema, and fever. Under these circumstances, pus can sometimes be expressed from the opening of the duct when the gland is pressed (Figure 57-1).
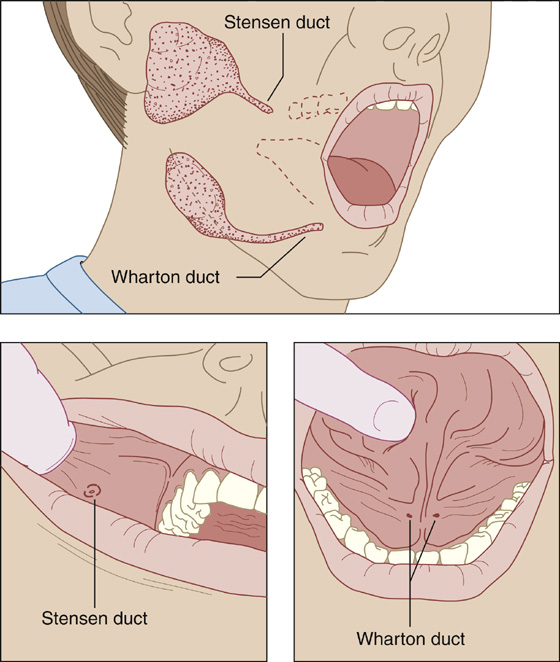
Figure 57-1 Most salivary duct stones occur in the Wharton duct.
What To Do:
 Conservative care is the mainstay of treatment for salivary duct stones. Patients should be advised to stay well hydrated, to apply warm compresses frequently while gently massaging the gland or “milking” the duct, and to suck on lemon drops or other hard tart candy (sialogogues, which promote ductal secretions) throughout the day as frequently as tolerated.
Conservative care is the mainstay of treatment for salivary duct stones. Patients should be advised to stay well hydrated, to apply warm compresses frequently while gently massaging the gland or “milking” the duct, and to suck on lemon drops or other hard tart candy (sialogogues, which promote ductal secretions) throughout the day as frequently as tolerated.
 If possible, discontinue anticholinergic medications that may inhibit ductal secretions, such as diphenhydramine or amitriptyline.
If possible, discontinue anticholinergic medications that may inhibit ductal secretions, such as diphenhydramine or amitriptyline.
 Control pain with nonsteroidal anti-inflammatory drugs (NSAIDs), or add narcotics if necessary.
Control pain with nonsteroidal anti-inflammatory drugs (NSAIDs), or add narcotics if necessary.
 Bimanually palpate the course of the salivary duct, feeling for stones. For the submandibular gland, palpate the floor of the mouth anterior to this gland in order to find a stone in the Wharton duct. For the parotid gland, palpate the buccal mucosa around the orifice to the Stensen duct and along the line from the earlobe to the jawline (see Figure 57-1).
Bimanually palpate the course of the salivary duct, feeling for stones. For the submandibular gland, palpate the floor of the mouth anterior to this gland in order to find a stone in the Wharton duct. For the parotid gland, palpate the buccal mucosa around the orifice to the Stensen duct and along the line from the earlobe to the jawline (see Figure 57-1).
 When a small superficial stone can be felt, anesthetize the tissue beneath the duct and its orifice with a small amount of lidocaine 1% with epinephrine. If available, a punctum dilator can be used to widen the orifice of the blocked duct. Milk the gland and duct with your fingers to express the stone or stones.
When a small superficial stone can be felt, anesthetize the tissue beneath the duct and its orifice with a small amount of lidocaine 1% with epinephrine. If available, a punctum dilator can be used to widen the orifice of the blocked duct. Milk the gland and duct with your fingers to express the stone or stones.
 If the stone cannot be palpated, try to locate it through radiographic examination. The imaging modality of choice for the evaluation of salivary stones is high-resolution non-contrast CT scanning. Fine cuts must be requested so that the stones are not missed. CT scans have a 10-fold greater sensitivity in detecting stones than do plain films and also provide the sensitivity to diagnose other pathology, such as a glandular mass. Standard radiographs may identify radiopaque stones with a sensitivity of 80% to 95% for submandibular stones, which tend to be larger, but only 60% for parotid stones, which tend to be smaller or not radiopaque. Dental radiographs shot at right angles to the floor of the mouth are much more likely to demonstrate small stones in the Wharton duct than standard radiograph studies. Ultrasonography is another good imaging option, identifying greater than 90% of stones that are 2 mm in diameter or larger, and it is better than sialography for describing the periglandular structures and is less invasive.
If the stone cannot be palpated, try to locate it through radiographic examination. The imaging modality of choice for the evaluation of salivary stones is high-resolution non-contrast CT scanning. Fine cuts must be requested so that the stones are not missed. CT scans have a 10-fold greater sensitivity in detecting stones than do plain films and also provide the sensitivity to diagnose other pathology, such as a glandular mass. Standard radiographs may identify radiopaque stones with a sensitivity of 80% to 95% for submandibular stones, which tend to be larger, but only 60% for parotid stones, which tend to be smaller or not radiopaque. Dental radiographs shot at right angles to the floor of the mouth are much more likely to demonstrate small stones in the Wharton duct than standard radiograph studies. Ultrasonography is another good imaging option, identifying greater than 90% of stones that are 2 mm in diameter or larger, and it is better than sialography for describing the periglandular structures and is less invasive.
 When a stone cannot be demonstrated or manually expressed, the patient should be referred for contrast sialography or surgical removal of the stone. Often, sialography, ultrasonography, CT scanning, or MRI will show whether an obstruction is due to stenosis, a stone, or a tumor.
When a stone cannot be demonstrated or manually expressed, the patient should be referred for contrast sialography or surgical removal of the stone. Often, sialography, ultrasonography, CT scanning, or MRI will show whether an obstruction is due to stenosis, a stone, or a tumor.
 If the patient has pain, swelling, erythema, and purulent discharge expressed from the gland and, possibly, systemic symptoms (fever/chills/tachycardia), suspect an associated infection, sialadenitis. Initiate treatment with amoxicillin/clavulanate (Augmentin), 875/125 mg bid, or clindamycin (Cleocin), 450 mg q6h, for 10 days after obtaining cultures. For the more severe infections (e.g., when there is fever, tachycardia, severe swelling, and pain), consider hospitalization for administration of IV antibiotics.
If the patient has pain, swelling, erythema, and purulent discharge expressed from the gland and, possibly, systemic symptoms (fever/chills/tachycardia), suspect an associated infection, sialadenitis. Initiate treatment with amoxicillin/clavulanate (Augmentin), 875/125 mg bid, or clindamycin (Cleocin), 450 mg q6h, for 10 days after obtaining cultures. For the more severe infections (e.g., when there is fever, tachycardia, severe swelling, and pain), consider hospitalization for administration of IV antibiotics.
What Not To Do:
 Do not attempt to dilate a salivary duct if the patient has a suspected case of mumps. Acute, persistent pain and swelling of the parotid gland along with inflammation of the papilla of the Stensen duct, fever, lymphocytosis, hyperamylasemia, and malaise should raise suspicion for mumps or other viruses that may cause sialadenitis.
Do not attempt to dilate a salivary duct if the patient has a suspected case of mumps. Acute, persistent pain and swelling of the parotid gland along with inflammation of the papilla of the Stensen duct, fever, lymphocytosis, hyperamylasemia, and malaise should raise suspicion for mumps or other viruses that may cause sialadenitis.
 Do not obtain sialography with acute infection. Injection of dye into an acutely inflamed gland may push the infection outside the gland capsule and into the surrounding soft tissues.
Do not obtain sialography with acute infection. Injection of dye into an acutely inflamed gland may push the infection outside the gland capsule and into the surrounding soft tissues.
Discussion
Sialolithiasis is the most common disorder of the salivary glands and may range from tiny particles to stones that are several centimeters in length. Salivary duct stones are generally composed of calcium phosphate and hydroxyapatite. Uric acid stones may form in patients with gout. Although the majority, approximately 92%, form in the Wharton duct (which arises from the medial surface of the submandibular glands) in the floor of the mouth, approximately 6% to 20% occur in the Stensen duct (which arises from the anterior border of the parotid gland) in the cheek, and 1% to 2% occur in the sublingual ducts. The exact cause of stone formation is unclear but it is felt to be secondary to secretion of saliva rich in calcium in the setting of partial obstruction of the duct caused by local inflammation or ductal injury, with consequent promotion of stone formation. Dehydration, anticholinergic medications and trauma may also contribute to the formation of salivary duct stones. Depending on the location and the size of the stone, the presenting symptoms vary. Although most salivary stones are asymptomatic or cause minimal discomfort, larger stones may interfere with the flow of saliva and may cause pain and swelling. As a rule, the onset of swelling is sudden and associated with salivation during a meal.
The differential diagnosis for sialolithiasis includes other disease processes that may affect the salivary gland: infections, inflammatory conditions, and neoplastic and nonneoplastic masses.
If left untreated, salivary stones can result in chronic sialadenitis and glandular atrophy. Conservative treatment may consist of oral analgesics and antibiotics. Surgical management may include salivary lithotripsy, basket retrieval, and sialendoscopy.
The presence of dry eyes and dry mouth with arthralgia or arthritis may suggest the diagnosis of Sjögren syndrome as the cause of chronic sialadenitis.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree


