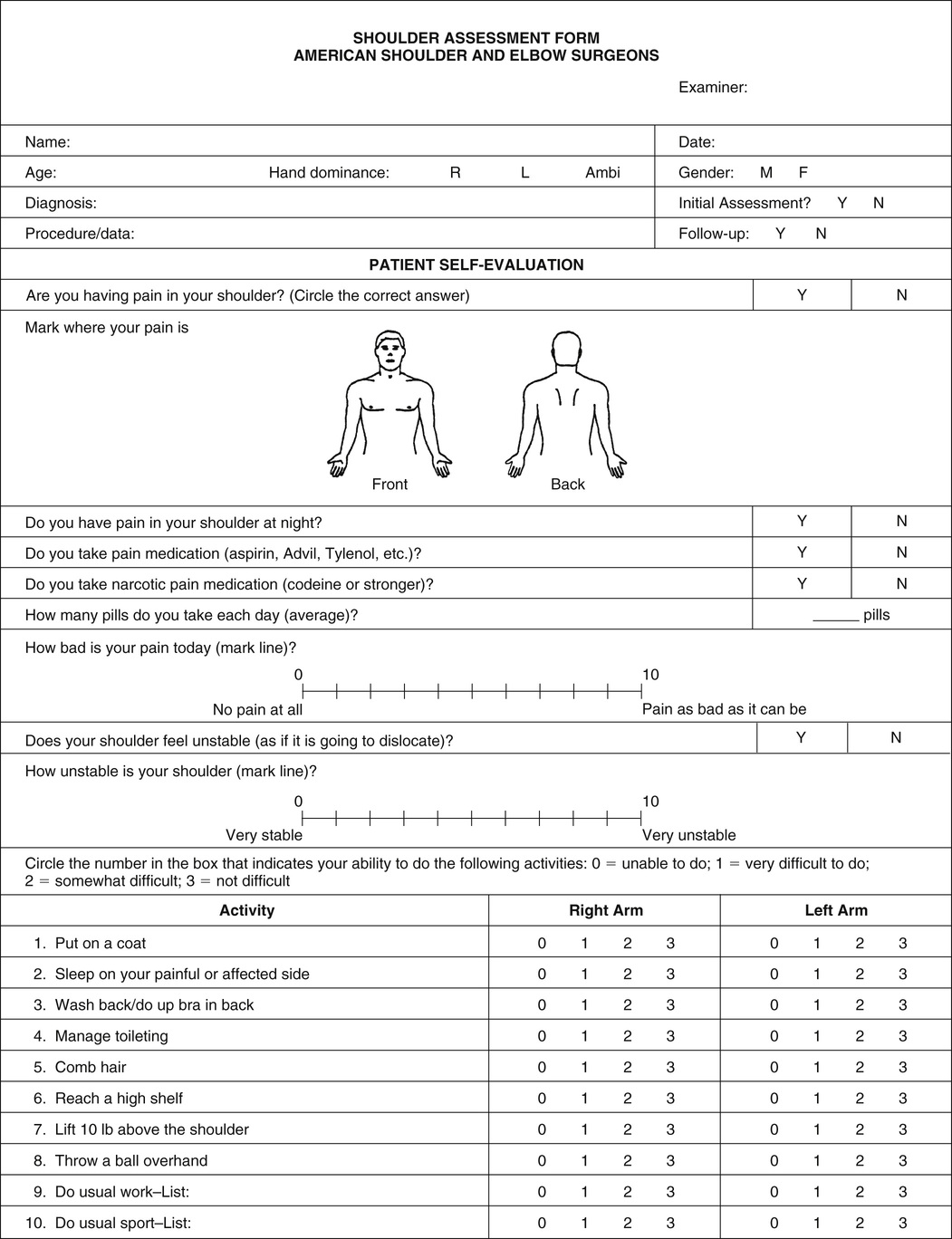
Kathy J. Fabiszewski Shoulder pain and dysfunction are among the most common musculoskeletal complaints encountered in primary and acute care settings, responsible for approximately 16% to 20% of all musculoskeletal encounters.1,2 Shoulder pain is second only to low back pain in patients seeking care for musculoskeletal symptoms in primary care,3 with approximately 1% of adults older than 45 years consulting a primary care provider for new shoulder pain annually.4 An estimated 20% of the population will have shoulder pain during their lifetime.3,4 Shoulder pain encompasses a diverse array of pathologies and can affect up to one fourth of the population, depending on age and risk factors.4 Shoulder pain is most often caused by an intrinsic disorder of the shoulder resulting from acute or chronic trauma, injury, and overuse or inflammation of the shoulder girdle and the surrounding articular surfaces, ligaments, tendons, and periarticular structures. Injury coupled with pain predisposes the individual to functional impairment or disability. The primary health care provider can, in most cases, diagnose and treat shoulder pain without specialty consultation. The shoulder is the most movable joint in the body and is composed of four separate joints or articulations that are made up of only three bones: the scapula, clavicle, and proximal humerus. The shoulder, or glenohumeral joint (the articulation of the humerus and the glenoid fossa of the scapula), is a closely fitted, shallow, complex ball-and-socket joint that is capable of a wide, almost global, range of motion. Adjacent to the glenohumeral joint are the acromioclavicular joint (the articulation between the acromion process and the clavicle) and the sternoclavicular joint (the articulation between the manubrium of the sternum and the clavicle), which form the shoulder girdle. At the scapulothoracic articulation, the scapula is suspended from the posterior thoracic wall by muscle attachments to the ribs and spine.5 Normal shoulder motion depends on the smooth, integrated movement of these four articulations. The primary movers of the glenohumeral joint are the pectoralis major and minor (adduct the shoulder), deltoid (abducts the shoulder), teres major, and latissimus dorsi.5 The trapezius muscles elevate and rotate the scapula. The shoulder joints are stabilized by the soft tissues of the shoulder girdle, including the joint capsule, glenoid labrum (a fibrocartilaginous ring attached to the outer rim of the glenoid that provides depth and stability), muscles of the rotator cuff, long head of the biceps, and scapular stabilizers. The shoulder socket (glenoid) is shallow and, because of the wide range of motion of the glenohumeral joint, inherently unstable; it is, in fact, the most unstable ball-and-socket joint in the human body. This anatomic arrangement provides for greater mobility but is accomplished by compromise of some stability (the maintenance of the humeral head properly positioned within the glenoid cavity), making the shoulder one of the most commonly dislocated joints in the body. The rotator cuff consists of the musculotendinous attachments of four muscles—the supraspinatus, infraspinatus, teres minor, and subscapularis muscles—that come together and form a cuff around the head of the humerus, attaching to the greater and lesser tuberosities. The rotator cuff compresses the humeral head in the glenoid fossa against the labrum and acts as the primary dynamic stabilizer to the glenohumeral joint. The chief function of the rotator cuff is the maintenance of stability during movements.6 The greater tuberosity of the humerus, the tendons of the rotator cuff muscles that elevate the arm, and the subacromial bursa move back and forth through a tight archway of bone and ligament known as the coracoacromial arch. When the arm is raised, the archway becomes smaller, causing these structures to impinge on one another and making them prone to inflammation and degeneration. Shoulder pain symptoms may be acute or chronic, specific or vague, persistent or recurrent. The patient with a shoulder problem typically reports shoulder pain that is aggravated by movement and is often accompanied by limitation of movement. There may or may not be a history of trauma or overuse. Surprisingly, many individuals fail to recollect an episode of trauma unless specifically asked. Patients younger than 40 years with a history of trauma are more likely to have shoulder dislocation or subluxation, whereas rotator cuff tear is more common after trauma in those older than 40 years.1 Patients often report difficulty with activities of daily living, such as bathing, combing their hair, or dressing, as well as with driving, carrying groceries, and exercising. Loss of range of motion is associated with adhesive capsulitis and glenohumeral arthritis.1 Other symptoms may include stiffness, crepitation, instability, and aching discomfort related to vigorous or sustained use. Most shoulder disorders hurt more when the shoulder is elevated, whereas many cervical radiculopathies feel better with the shoulder in an elevated position.6 Numbness, tingling, and pain radiating distal to the elbow suggest a cervical cause of the symptoms and are seldom indicative of shoulder disease.1 Weakness is associated with rotator cuff disorders and glenohumeral arthritis.1 Anterior-superior shoulder pain is associated with acromioclavicular joint disease.1 Diffuse shoulder pain is associated with rotator cuff disorders, adhesive capsulitis, or glenohumeral arthritis.1 Inquiry about hand dominance, occupational activities (e.g., lifting, chronic stress on joints, safety precautions), exercise and recreational activities (extent, type, and frequency), and self-care capacity facilitates identification of contributing factors, potential causes, and the functional impact of the symptoms. A history of collision sports (football, hockey) or weightlifting makes instability or acromioclavicular arthritis more likely, whereas overhead sports (baseball, softball, tennis) make rotator cuff disease more likely.1 Superior labral tears, including superior labrum anterior and posterior (SLAP) injury, may occur during a motor vehicle accident; a fall onto an outstretched arm; forceful pulling of the arm, such as when trying to catch a heavy object; or forceful movement of the arm when it is above shoulder level.7 Identification of any history of recent or remote trauma, including the details of injury, is vital. Determination of previous diagnostic studies, hospitalizations, surgeries, or therapies guides diagnostic evaluation. A detailed medical history is also important because adhesive capsulitis is associated with diabetes mellitus and thyroid disorders,1 and humeral fractures are a consideration in the older adult with osteoporosis or cancer. Because nonextrinsic shoulder pain may be caused by either intrinsic shoulder disorders or referred pain, it is also critical to ascertain the exact location and distribution of the pain. It is unusual for pain originating in the shoulder, for example, to radiate below the elbow.1 Vague, poorly localized pain is often extrinsic in origin. Pain involving other joints is suggestive of a generalized arthritic process. Characterization of the type, intensity, timing, and duration of pain as well as identification of ameliorating and exacerbating factors is also essential. The American Shoulder and Elbow Surgeons standardized form for assessment of the shoulder incorporates a synopsis of both patient self-evaluation data and physical examination parameters and is useful in organizing a primary care approach to shoulder pain (Fig. 186-1). Physical examination of the shoulder should be performed in a systemic manner beginning with careful visual inspection of the shoulder. Anterior and posterior examination for surgical scars, displacement of bone prominences, warmth, swelling, changes in skin color or texture, suprascapular or infrascapular muscle atrophy, and winging of the scapula is necessary. Asymmetry with the contralateral shoulder should be noted. Classically, there is focal tenderness that may or may not reproduce the presenting complaint. Before any shoulder movement is initiated, the examiner should palpate each shoulder for tenderness in the sternoclavicular joint, the acromioclavicular joint, and the shoulder itself. Palpation of both shoulders simultaneously allows the examiner to compare the affected shoulder with the unaffected shoulder. Palpation of bone landmarks is especially valuable in excluding a joint disorder; palpation of the muscle structures is useful in excluding spasm. A simple shoulder examination checklist is provided in Box 186-1. Active range of motion should be assessed first to determine the integrity of the rotator cuff and to ascertain the location of the pain. Active range of motion of each shoulder should be measured, including forward flexion (normal is 180 degrees), extension (normal is 70 degrees), external rotation (normal is 45 degrees), internal rotation (normal is 60 degrees), abduction (normal is 180 degrees), and adduction (normal is 180 degrees). Any clicks or crepitation suggestive of impingement should be noted. Passive range of motion should be compared with active range of motion and is particularly useful in determining whether adhesive capsulitis (frozen shoulder) is present. A person with adhesive capsulitis can typically still abduct the arm 60 degrees. Patients with a rotator cuff tear seldom lose passive shoulder motion.8 Strength testing of the individual rotator cuff muscles is then performed with use of resisted movements. An important component of the physical examination of the shoulder involves tests to detect pathology.9 Table 186-1 summarizes special tests of shoulder function and their associated disorders. Although many of these clinical tests have variable accuracy for elucidating the exact cause of shoulder pain,10 they may be used to confirm a suspected diagnosis, provide a differential diagnosis, or differentiate among various structures or to better understand the cause of unusual signs or symptoms. Complete neurovascular assessment of the associated shoulder structures should also be performed to identify other underlying sources of pain or dysfunction. Sensory, motor, deep tendon reflex, or circulatory impairment should be documented. The spine and peripheral joints are examined for evidence of coexisting joint disease. TABLE 186-1 Tests of Shoulder Function Evaluation of a painful shoulder is challenging because the problem is often dynamic, with pain occurring only with specific activity. It is necessary to determine whether the discomfort and immobility are articular (bone) or periarticular (soft tissue structure). With inflammatory bursitis, erythema or bulging in the anterior shoulder may be seen. With bursitis or adhesive capsulitis, both active and passive range of motion will be limited. Marked weakness in abduction and external rotation suggests rotator cuff tear.6 Diagnostic tests should be used judiciously to confirm or to refine suspected clinical diagnoses. It is unwise to base a diagnosis on a radiologic test alone because x-ray studies can be misleading or unrevealing. Findings on radiography and even magnetic resonance imaging (MRI) are often normal in soft tissue problems in the young athlete. Most conditions seen in primary care do not have specific radiographic findings.6 A thorough history and targeted musculoskeletal examinations are most critical in providing clues to the diagnosis. Radiographs are usually the initial imaging test performed for most suspected abnormalities in the shoulder and will often suffice to diagnose or exclude an abnormality, or will guide further imaging.11 Plain x-ray films may help diagnose massive rotator cuff tears, calcific tendinitis, shoulder instability, and shoulder arthritis. Shoulder films are recommended for a history of trauma, with reduced range of motion, or if arthritis or neoplastic disease is a consideration. With all significant trauma, it is imperative to obtain the appropriate x-ray studies, including standard anteroposterior views of the glenohumeral joint with the arm at 30 degrees of external rotation, axillary lateral views, and scapula Y views that detect dislocation not seen on standard views. On occasion, in atraumatic presentations, calcifications from previous or chronic injuries can be seen. In cases of recurrent rotator cuff tendinitis or subacromial bursitis, x-ray studies may be helpful in looking for spurring of the acromial process or inferior acromioclavicular osteophytes. Loss of articular cartilage between the humeral head and the glenoid may confirm suspected glenohumeral joint arthritis. Osteophytes consistent with osteoarthritis may also be seen. X-ray studies of the cervical spine are indicated if cervical radiculopathy is suspected. When the diagnosis of shoulder pain remains unclear or when the outcome would affect management, additional testing with the use of imaging techniques should be performed. MRI is the preferred imaging modality for evaluation of the soft tissue structures of the shoulder including the rotator cuff, biceps muscles, tendons, and bursa. MRI should be performed only for a valid medical reason and after careful consideration of alternative diagnostic techniques.11 In many cases of shoulder pain in the primary care setting, however, MRI findings are rarely helpful initially, with the exception of a significant trauma history, and are unlikely to alter management. In addition, the frequency of nonspecific MRI findings often found in asymptomatic individuals is such that unless the clinician knows of the specific abnormality to be corroborated by MRI, its ordering should probably be left to a specialist. Although MRI is one of the most sensitive diagnostic tests for detecting anatomic abnormalities of the shoulder, the findings may be misleading if not closely correlated with other imaging studies, the patient history, physical examination, and tests of shoulder function.11 Collaboration between the ordering clinician and the radiologist is often of benefit in interpreting radiologic findings in the context of the clinical picture. Diagnostic imaging studies, which also include ultrasonography and computed tomography (CT) scans as well as invasive studies such as MRI arthrography, are best ordered in consultation with a specialist, particularly when there may be a need for surgical intervention. Laboratory studies are seldom indicated. However, complete blood count (CBC), erythrocyte sedimentation rate (ESR), uric acid level, and serologic tests for rheumatologic diseases should be performed in accordance with the history and examination findings.
Shoulder Pain
Definition and Epidemiology
Pathophysiology
Clinical Presentation
Physical Examination
Test
Technique
Interpretation
Apprehension test
Abduct to 90 degrees and slowly externally rotate patient’s arm to a position where it might easily dislocate.
Impending dislocation or glenohumeral instability is signaled by noticeable look of apprehension on patient’s face, with patient resisting further motion.
Drop arm test
Have patient hold affected extremity in a fully abducted position, then ask patient to slowly lower arm to side.
Rotator cuff tearing or supraspinatus tearing is suggested if patient’s arm drops to side (as opposed to being slowly lowered to the side) from a position of 90 degrees of abduction.
Empty can test
Have patient hold out affected arm as if offering examiner a can of soda (abduction to 90 degrees), and then have patient turn arm to empty the contents (internal rotation).
Rotator cuff tendinitis or tear is suggested if pain is produced or weakness noted by maneuver of “emptying the can.”
Impingement test
Have patient elevate arm slowly into overhead position.
Rotator cuff strain, tendinitis, or tear is suggested if patient experiences sharp “catches” of pain or impingement with this maneuver.
Yergason test
Have patient fully flex elbow (90 degrees). Grasp the patient’s flexed elbow in one hand while holding patient’s wrist in other hand; to test stability of biceps tendon, externally rotate the patient’s arm as patient resists and, at same time, pull downward on patient’s elbow.
Pain with this maneuver suggests that the biceps tendon is unstable in the biceps groove; no pain is experienced with a stable tendon.
Modified dynamic labral shear test
Have patient stand with arm flexed 90 degrees at the elbow, abducted in the scapular plane more than 120 degrees, and externally rotated to tightness. Stand behind patient and guide the involved upper extremity into maximal horizontal abduction. Apply a shear load to the joint by maintaining external rotation and horizontal abduction and lowering arm from 120 degrees to 60 degrees of abduction.
Reproduction of pain and/or painful click or catch in the posterior joint line between 120 degrees and 90 degrees abduction suggests labral tear.10
Sulcus sign
Have patient stand with arm at the side. Apply traction through the patient’s arm in the inferior direction.
Indicates glenohumeral laxity or instability.
Hawkin test
Forward flex the shoulder and elbow to 90 degrees. Apply force to the forearm to internally rotate the shoulder.
Elicitation of subacromial pain indicates supraspinatus tendinitis.
Cross-body adduction
Elevate shoulder to 90 degrees. Horizontally adduct the shoulder and arm across the body.
Pain at the acromioclavicular joint suggests acromioclavicular joint arthritis.
Spurling test
Have patient flex cervical spine laterally toward the ipsilateral shoulder. Apply a downward axial force on the head.
Pain radiating toward the shoulder and arm may indicate nerve root compression, implicating the cervical spine as the source of shoulder pain.
Diagnostics
Shoulder Pain
Chapter 186