
Shoulder Injuries
Scott C. Sherman
The shoulder joint is composed of three bones (humerus, clavicle, and scapula) and three joints (sternoclavicular [SC], acromioclavicular [AC], and glenohumeral). Figure 38.1 demonstrates the essential osseous and ligamentous anatomy of the shoulder. The rotator cuff surrounds the glenohumeral joint and is composed of the teres minor, infraspinatus, and supraspinatus muscles, which insert on the greater tuberosity of the humerus; and the subscapularis muscle, which inserts on the lesser tuberosity of the humerus. Superficial to these muscles is the deltoid muscle.
The proximal humerus articulates with the glenoid, forming the glenohumeral joint. Because the articular surface ends at the anatomic neck, fractures located proximal to this location are considered articular surface fractures. The surgical neck is the narrow portion of the proximal humerus distal to the greater and lesser tuberosities.
The clavicle is anchored to the scapula by the AC and coracoclavicular ligaments. The SC and costoclavicular ligaments anchor the clavicle medially. The scapula lies over ribs 2 through 7 posteriorly. It is covered with thick muscles over its entire body and spine. The scapula is connected to the axial skeleton solely by the AC joint.
The glenohumeral joint and scapulothoracic articulation function as a unit in abducting the humerus. The ratio of scapular to glenohumeral movement is 1:2; therefore, for every 30 degrees of abduction of the arm, the scapula moves 10 degrees and the glenohumeral joint moves 20 degrees. If the glenohumeral joint is completely immobilized, the scapulothoracic articulation can provide 65 degrees of abduction.
DIFFERENTIAL DIAGNOSIS
The differential diagnosis of shoulder injuries includes tendonitis, rotator cuff tears, bursitis, fractures of the clavicle, proximal humerus and scapula, shoulder dislocations, and injuries to the AC and SC joints.
ED EVALUATION
The clinician should ask the patient about the mechanism of injury, as this frequently aids in diagnosis. In atraumatic conditions, inquire about overuse and activities that worsen pain. A history of prior shoulder injury or surgery is also useful. Finally, the clinician should consider the possibility that the source of pain is not due to shoulder pathology and may represent referred pain from a more severe underlying condition (e.g., myocardial ischemia, perforated viscus).
The examination of the shoulder should be systematic to avoid missing injuries. The examiner starts by inspecting and noting how the patient holds the shoulder and also the presence of any gross deformities or ecchymosis. Palpation begins at the SC joint immediately lateral to the suprasternal notch. The examiner then moves laterally along the clavicle, noting any areas of deformity or tenderness. The AC joint is palpated by pushing in a medial direction against the distal end of the clavicle as it protrudes above the flattened acromion process.
Next, the examiner palpates the proximal humerus. The greater tuberosity of the humerus lies lateral to the acromion process and can easily be felt by following the acromion process to its lateral edge and then sliding the fingers inferiorly. Absence of the proximal humerus in its typical location and a squared-off appearance of the shoulder are consistent with an anterior shoulder dislocation. The bicipital groove, which contains the biceps tendon, is located anterior and medial to the greater tuberosity and is bordered laterally by the greater tuberosity and medially by the lesser tuberosity. Tenderness in this location is consistent with bicipital tendonitis. External rotation places the groove in a more exposed position for palpation and permits the examiner to palpate the greater tuberosity first, then the bicipital groove, and finally the lesser tuberosity by moving from a lateral to a medial position. Lastly, the attachment of the supraspinatus tendon on the greater tuberosity is palpated. Tenderness in this location is seen in patients with supraspinatus tendonitis and subacromial bursitis.
As with any extremity injury, the clinician must consider injury to nerves and blood vessels and perform a thorough neurovascular examination. The subclavian vessels and the brachial plexus lie in close proximity to the clavicle, so displaced clavicle fractures can be associated with injuries to these structures, but this is rare. The brachial plexus, axillary nerve, and axillary artery lie in close proximity to the proximal humerus, and injuries to these structures may accompany proximal humerus fractures.
The examiner should test function of the associated muscles and range of motion of the shoulder joint. Inability to initiate abduction or hold the arm in a 90-degree position despite a slight pressure on the distal forearm suggests a significant tear to the rotator cuff muscles. Strength of abduction is proportional to the size of the tear. Inability to externally or internally rotate the shoulder suggests the possibility of a shoulder dislocation.
Radiographs are indicated in most traumatic situations. Routine shoulder radiographs consist of an anteroposterior (AP) view in internal and external rotation as well as a scapular “Y” view. The scapular “Y” view is obtained by placing the radiographic film along the lateral side of the humerus, with the beam projected along the length of the scapula. The “Y” consists of the scapular spine, body, and coracoid process, with the humeral head positioned at the junction of the “Y.” This radiograph is useful to identify dislocations of the glenohumeral joint and scapular fractures. When the location of the humeral head is in question, it is important to obtain an axillary view. The axillary view requires abduction of the shoulder and the beam is projected superiorly through the axilla with the plate on top of the shoulder.
Clavicle radiographs include an AP view of the upper thorax to define the structures. An AP view with the tube directed 45-degree cephalad (apical lordotic) is useful to detect medial-third fractures or SC joint dislocation (1). Multidetector CT will aid in diagnosing occult fractures or better delineate complex proximal humerus fractures, but is not routinely indicated in the ED (2).
KEY TESTING
• Routine shoulder radiographs that include AP views in internal and external rotation and a scapular “Y” view.
• An axillary view should be obtained when a dislocation is suspected on routine views.
• SC joint dislocation will be occult on routine views of the clavicle. Computed tomography (CT) scan or apical lordotic view should be ordered when clinically suspected.
ED MANAGEMENT
Clavicle Fractures
Clavicle fractures account for 5% of all fractures. They are the most common childhood fracture and may be encountered in newborns secondary to birth trauma. Two mechanisms are responsible: (i) Force applied directly to the clavicle and (ii) force applied to the outer end of the clavicle, which can push the shoulder inward toward the chest, causing a shearing force that fractures the clavicle. Most patients have swelling and tenderness over the fracture site. Frequently, the shoulder is held in downward and inward positions due to loss of support.
Middle-third clavicle fractures are most common, occurring in 80% of all clavicle fractures (eFig. 38.1). Nondisplaced middle-third fractures in adults have an intact periosteum. These heal well and require only a sling for support and ice to reduce swelling. For displaced fractures, a figure-of-eight harness can be used for reduction and maintenance of position, but it provides no more benefit in pain control or fracture reduction than a simple sling. Surgical fixation is frequently recommended in adults with displaced clavicle fractures, necessitating referral to an orthopedist. Complications of middle-third clavicle fractures include malunion; excess callus formation, resulting in cosmetic defect; and neurovascular compromise.
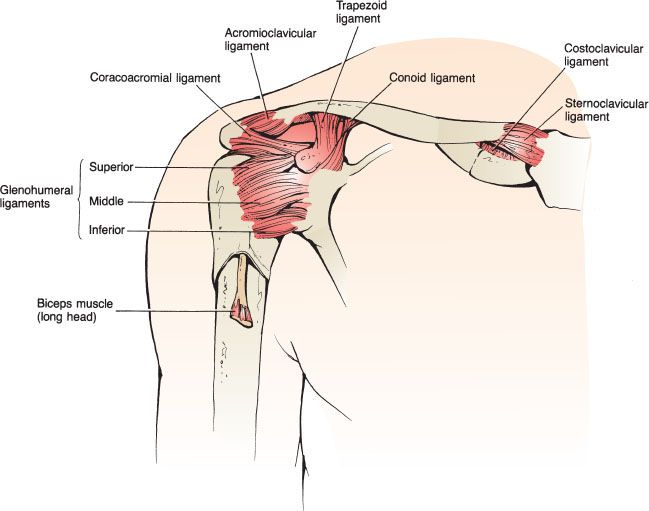
FIGURE 38.1 The ligamentous and bony anatomy of the shoulder.

eFIGURE 38.1 Clavicle fracture. The attachment of the sternocleidomastoid muscles pulls the medial segment superiorly.
Distal-third clavicle fractures account for 15% of all clavicle fractures. Nondisplaced fractures of the distal clavicle are splinted by the surrounding intact ligaments and muscles. They are usually treated symptomatically with ice, analgesics, a sling, and early motion. Displaced fractures of the distal clavicle may require surgical intervention because of rupture of the coracoclavicular ligament (3). Complications of displaced fractures treated conservatively include nonunion. Degenerative arthritis may occur when there is intra-articular involvement.
Medial-third clavicle fractures represent only 5% of all clavicle fractures. Considerable force is required to fracture the medial clavicle, so associated intrathoracic injuries should be considered. Management includes ice, analgesics, and a sling for support. Displaced fractures require orthopedic referral for reduction. Degenerative arthritis frequently complicates these fractures.
Proximal Humerus Fractures
Proximal humeral fractures account for approximately 2% to 3% of upper extremity fractures. They are most common in elderly osteoporotic women. Anatomically, proximal humeral fractures include all humeral fractures proximal to the surgical neck. Two mechanisms of injury are commonly responsible: (i) a direct blow on the lateral aspect of the arm and (ii) a fall on an outstretched arm. Patients present with pain and swelling over the upper arm and shoulder. Most commonly, the arm is held adducted.
The Neer classification system for proximal humerus fractures is widely used and has both prognostic and therapeutic implications. In this system, the proximal humerus is divided into four segments: greater tuberosity, lesser tuberosity, humeral head, and humeral shaft (4). Depending on the displacement and angulation of fractures of these four components, the injury is divided into one-, two-, three-, and four-part fractures (eFig. 38.2).
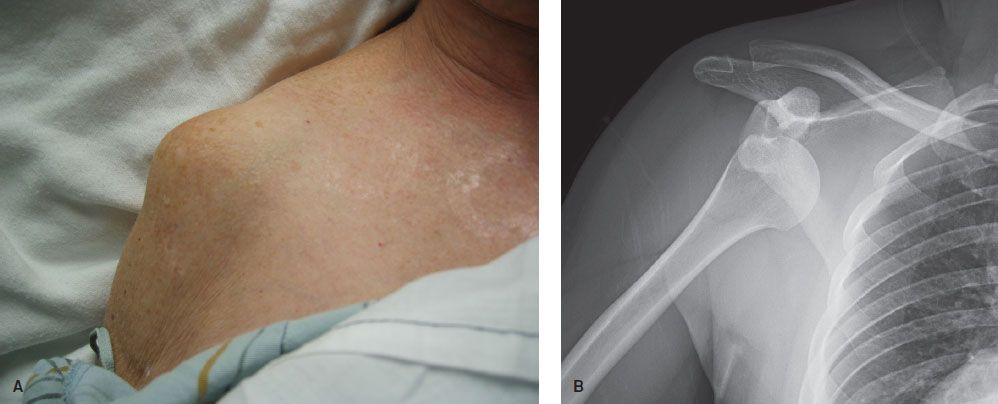
FIGURE 38.2 Anterior shoulder dislocation. A: A “rounded off” appearance of the affected shoulder is typical clinically. B: Characteristic radiographic appearance of a subcoracoid dislocation.
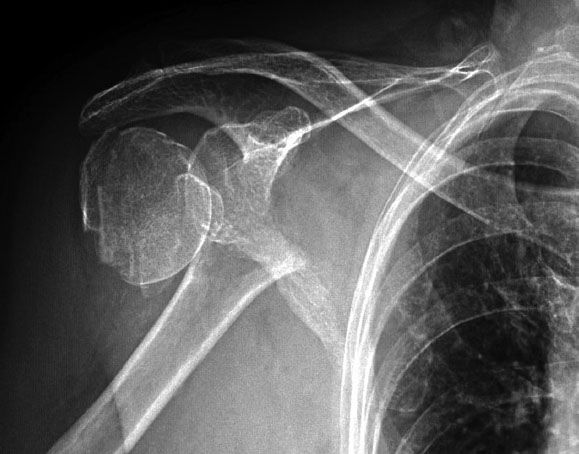
eFIGURE 38.2 Proximal humerus fracture. This image is of a surgical neck fracture with complete displacement. This is an example of a two-part fracture.
One-part fractures are nondisplaced (<1 cm) fractures without significant angulation (<45 degrees). These fractures are the most common type of proximal humerus fracture and represent more than 85% of cases. The humeral fragments are held in place by the periosteum, rotator cuff, and joint capsule. Therapy for one-part fractures includes immobilization in a sling and swathe and orthopedic referral within 4 to 5 days. Circumduction exercises should begin as soon as tolerated, and should be followed by passive exercise of the elbow and shoulder at 2 to 3 weeks. Shoulder motion exercises can usually be started within 3 to 4 weeks.
Two-part fractures have a fragment with more than 1 cm of displacement or over 45 degrees of angulation. These fractures require immobilization with a sling and swathe and orthopedic referral. Surgery is recommended for two-part fractures of the greater and lesser tuberosity, angulated surgical neck fractures, and in unstable surgical neck fractures in which there is disengagement of the shaft from the humeral head.
Three- and four-part fractures result from severe forces. Three-part fractures involve two fragments that are individually displaced from the humeral head. Four-part fractures involve three fragments individually displaced from the remaining humeral head. These fractures are associated with shoulder dislocations, rotator cuff injuries, and neurovascular compromise. Therapy includes sling immobilization and emergent orthopedic referral or admission. Virtually all of these fractures require surgical repair.
Scapular Fractures
Scapular fractures are rare and represent only 1% of all fractures and 5% of fractures involving the shoulder. Treatment, associated injuries, and complications depend on the portion of the scapula that is fractured.
Body or spine fractures are significant because a great deal of force is usually required to cause these fractures; therefore, they are sometimes associated with other more serious injuries to thoracic structures. Typically, there is little displacement, due to the support of the investing muscles and periosteum. Treatment includes sling and swathe immobilization, early limited exercise, and orthopedic referral.
Acromion fractures result from a direct downward blow to the shoulder. Due to the large amount of force required to produce these fractures, they are often accompanied by brachial plexus injuries, rotator cuff tears, and shoulder dislocations. Nondisplaced fractures are treated with sling immobilization in conjunction with an elastic circular dressing that pushes the elbow up and the lateral clavicle down. Displaced fractures require internal fixation.
Glenoid rim fractures are associated with two mechanisms of injury. A direct blow may result in a stellate fracture. An upward force, secondary to a fall on the flexed elbow, may cause a displaced glenoid rim fracture. Glenoid rim fractures also occur with shoulder dislocations and are referred to as Bankart lesions. Therapy for fractures with small fragments consists of sling immobilization, ice, and analgesia. Large or widely displaced fragments and stellate fractures require surgical fixation.
Coracoid process fractures occur from a direct blow to the superior part of the shoulder, or from violent contraction of one of the inserting muscles. The patient presents with tenderness to palpation over the coracoid process. Radiographs should include an axillary view for delineation of any displacement of the fragment. Coracoid fractures are usually treated symptomatically with a sling, ice, and analgesics.
Anterior Shoulder Dislocation
Anterior shoulder dislocation is one of the most common dislocations, accounting for half of all dislocations presenting to the ED. This injury occurs when a blow to an abducted, externally rotated arm disrupts the anterior capsule and the glenohumeral ligaments (5). Less commonly, a force to the posterior humerus or a fall on an outstretched arm is the cause.
The patient presents with the affected arm held to the side and resistant to all movements. The patient will be unable to touch the uninjured shoulder with the hand of the dislocated shoulder. In thin individuals, the acromion is prominent, and there is loss of the normal rounded contour of the shoulder (Fig. 38.2A). Upon palpation lateral to the acromion, there is a noticeable gap where the humeral head used to be positioned.
Axillary nerve injury is the most common associated neurologic injury in anterior shoulder dislocations. The axillary nerve is assessed by testing pinprick sensation over the lateral aspect of the deltoid in the “shoulder badge” distribution or deltoid muscle weakness. Unfortunately, sensory loss is not reliably present and an accurate motor examination is impractical in a patient with an acute dislocation. While nerve dysfunction is common, it is seen in up to 42% of patients, most patients recover without intervention.
On AP radiographs, the humeral head is in one of three locations: subclavicular, subcoracoid, or subglenoid (Fig. 38.2B). The physician should determine the position of the humeral head to ascertain if there are associated injuries. The typical position is subcoracoid. If the humeral head is in a subglenoid or subclavicular position, the patient has either a greater tuberosity fracture or a rotator cuff tear. The scapular Y view, true AP (Grashey view—beam directed at a 45-degree angle from a medial to lateral direction with the plate parallel to the scapular body), and axillary view are used in equivocal cases.
Clinically important fractures are seen in approximately 25% of cases and are more common in patients over age 40, first-time dislocations, and after a traumatic mechanism. In patients with none of these three factors present, a prereduction radiograph is unlikely to be beneficial when the diagnosis is obvious clinically (6,7). The most common associated fracture is an impaction fracture on the posterior lateral portion of the humeral head known as the Hill–Sachs deformity. It is present in 40% of dislocations. Other fractures include Bankart fractures of the anterior glenoid rim (5%) and greater tuberosity fractures (10%). A nondisplaced fracture of the surgical neck is a rare associated injury, but important to note, as attempts at closed reduction of the shoulder dislocation are contraindicated. Attempts at reduction may displace the fracture and worsen the prognosis.
Reduction should begin after obtaining informed consent. Procedural sedation is not necessary in all cases, especially in recurrent dislocators who present promptly. Patient preference should be considered. Reduction without procedural sedation is unlikely to be successful in a patient who is anxious, in pain, and unable to assist in the reduction by relaxing their musculature. Some have used intra-articular lidocaine with good results (8).
There are numerous reduction techniques described, but most techniques use or combine scapular movement, external rotation, shoulder abduction, and traction of the arm. The best technique is one that is quick, simple, associated with few complications, and requires the smallest amount of force. One method that meets these requirements is scapular manipulation with downward traction on the arm by an assistant. Success rates with this maneuver range from 80% to 100% (9–11). This technique is attempted without procedural sedation in most cases. If this is unsuccessful, the external rotation technique can be used, followed by traction–countertraction, if necessary. Other acceptable alternative techniques include the Milch, Stimson, Spaso, Fares, and Cunningham methods.
Scapular Manipulation Technique
The head of the stretcher is placed at 90 degrees. The patient sits upright with the unaffected shoulder leaning against the head of the stretcher and the legs hanging off the edge (no procedural sedation). The physician stands behind the patient and pushes the tip of the scapula medially and the superior aspect of the scapula laterally (11). This scapular rotation allows the humeral head to disengage from the glenoid. An assistant, standing in front of the patient, gently applies a downward force (Fig. 38.3A) (18).

FIGURE 38.3 Methods of reducing an anterior shoulder dislocation. A: Scapular manipulation with downward traction on the arm for anterior shoulder dislocation. B: External rotation technique for anterior shoulder dislocation. C: Traction–countertraction technique for reducing anterior shoulder dislocations.









