STERNOCLAVICULAR SPRAINS AND DISLOCATIONS
The sternoclavicular joint contains an intra-articular fibrocartilaginous disc and has the least amount of bony stability of any major joint because less than half of the medial end of the clavicle articulates with the upper sternum. However, it is remarkably stable, due to the strong surrounding ligaments, and as a result, most injuries are simple sprains, while dislocations and fractures are uncommon.1,2,3
The medial clavicular epiphysis is the last epiphysis of the body to appear radiographically (age 18 years old) and the last to close (age 22 to 25 years old). An apparent sternoclavicular joint dislocation in children and young adults is typically a Salter-Harris type I or II fracture, with either anterior or posterior displacement of the clavicular metaphysis that requires orthopedic consultation and follow-up for optimal healing and remodeling.1,4
A posterior dislocation results from a direct blow or from an indirect force to the shoulder, causing the shoulder to roll forward at the time of impact. An anterior dislocation may result from a similar indirect force if the shoulder is rolled backward at the moment of impact.
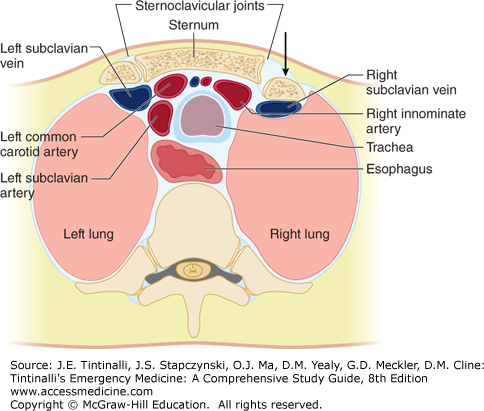
The major symptom is severe pain, exacerbated by arm motion and lying supine. The shoulder may appear shortened and rolled forward. On examination, anterior dislocations have a prominent medial clavicle end that is visible and palpable anterior to the sternum, although swelling and tenderness may impede diagnosis. In posterior dislocations, the medial clavicle end is less visible and often not palpable, and the patient may have signs and symptoms of impingement of the superior mediastinal contents, such as stridor, dysphagia, and shortness of breath (Figure 271-1).3 Minor trauma, on the other hand, may result in a sprain to the sternoclavicular joint with only pain and swelling localized to the joint.
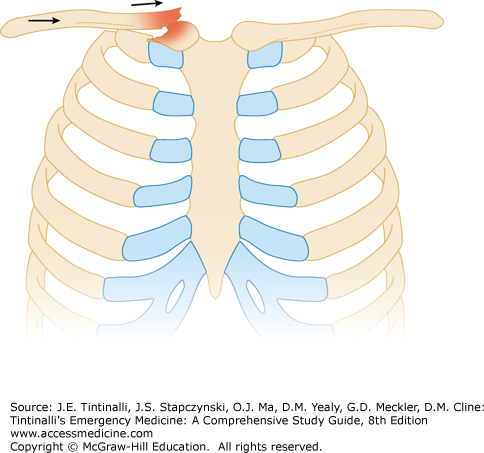
Routine radiographs have a low sensitivity for the detection of dislocation, but immediate chest x-ray is needed to exclude a pneumothorax, pneumomediastinum, and hemopneumothorax. Special views and comparison with the other clavicle may be helpful.1 CT is the imaging procedure of choice (Figure 271-2) and is recommended in any posterior dislocation with concern for injury to the mediastinal structures. IV contrast may be administered to further delineate injury. US can identify sternoclavicular joint effusions.
Sprains of the sternoclavicular joint are treated with ice, sling, and analgesics. In a nontrauma patient, pain at the sternoclavicular joint should raise suspicion for septic arthritis, especially in injection drug users. US can detect effusion and aid in joint aspiration.
Patients with uncomplicated anterior dislocations may be discharged without an attempted reduction, because this injury has little or no impact on function. Clavicular splinting, ice, analgesics, sling, and orthopedic referral are required.
For closed reduction, which can be performed within 10 days of the injury, the patient is placed supine with a towel roll or similar between the scapulae. The arm is abducted to 90 degrees, longitudinal traction is applied with slight extension by moving the arm toward the ground, and pressure is placed over the medial end of the clavicle.5 Even with reduction, the joint is usually unsTable and redislocates (50%) when pressure is released.
Posterior dislocations may be associated with life-threatening injuries to adjacent structures, including pneumothorax or compression or laceration of surrounding great vessels, trachea, or esophagus.1,2 Orthopedic consultation is necessary for closed or open reduction. Open reduction should be performed in the operating room with trauma or vascular surgery available.1,3,5
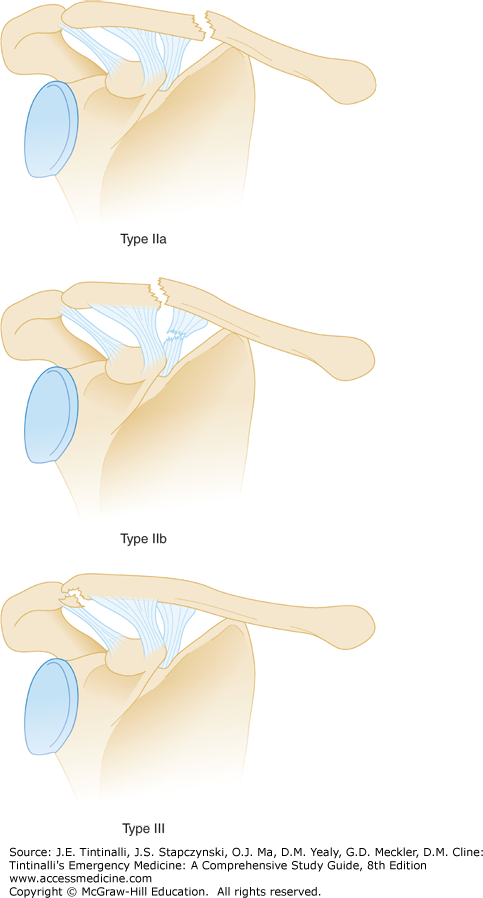
CLAVICLE FRACTURES
The clavicle provides support and mobility for upper extremity tasks by functioning as a strut that connects the shoulder girdle to the trunk. It articulates with the sternum proximally and the acromion distally. In addition, the clavicle protects the adjacent lung, brachial plexus, and subclavian and brachial blood vessels. The clavicle is S-shaped, and the mid-portion of the clavicle is the thinnest, having no accompanying ligamentous or muscular attachments. Fracture results from a direct blow to the shoulder, buckling the clavicle.
Clinical signs are swelling, deformity, and tenderness overlying the clavicle. The arm is slumped inward and downward, and range of motion is limited. The fracture can often be palpated, and crepitus may be present.
Most clavicle fractures can be diagnosed on standard shoulder and clavicle x-rays. Occasionally, routine clavicle radiographs may miss some fractures, particularly at either end of the bone, due to overlap of surrounding structures. If a fracture is clinically suspected but not initially diagnosed with standard radiographs, a 45-degree cephalad tilt view may be used for further assessment. Definitive diagnosis may require CT.
Obtain emergent orthopedic consultation for open fractures, fractures with neurovascular injuries, and fractures with persistent skin tenting.
Fractures of the middle third of the clavicle are most common. Although midclavicular fractures are often managed nonoperatively, operative fixation may result in improved functional outcome and a lower rate of malunion and nonunion.6,7,8 Some fractures (Table 271-1), including severely comminuted or displaced fractures, benefit from referral and possible operative intervention.9,10 Additional considerations for orthopedic referral include athletes, professional impact, and cosmetic concerns. Referral to an orthopedist within a few days of injury should be considered in the above instances. In cases where the patient does not want surgery or is a poor surgical candidate, conservative treatment is an appropriate strategy. Initial treatment of midclavicle fractures includes immobilization with either a sling or figure-of-eight brace. The length of immobilization is typically 4 to 8 weeks, until the fracture is no longer painful. Initial primary care or orthopedic follow-up should be in 1 to 2 weeks after injury in conservative treatment. The patient may use the arm as pain permits but should avoid repeat injury from direct contact. Encourage daily range of motion of the elbow immediately and of the shoulder as soon as pain allows (3 to 5 days).
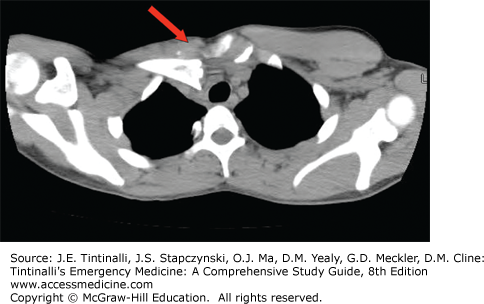
Distal clavicle fractures are divided into three subtypes. In type I fractures, the fracture is distal to the coracoclavicular ligaments, with the ligaments remaining intact. In type II fractures, the location of the fracture is the same as in type I; however, the coracoclavicular ligaments are disrupted (Figure 271-3). This results in an upward displacement of the proximal aspect of the clavicle. Type II distal clavicle fractures may require operative intervention to avoid nonunion.11 Type III fractures are intra-articular fractures through the acromioclavicular (AC) joint. Type I and III fractures can be managed conservatively with sling immobilization and primary care follow-up in 1 to 2 weeks.12
Proximal third clavicle fractures are often high-mechanism injuries and can be associated with intrathoracic trauma. CT can diagnosis the fracture and identify additional injuries. Emergent referral is required when posteriorly displaced fragments compromise mediastinal structures. Refer all other proximal third fractures to orthopedics within 1 to 2 weeks. Initial management includes sling immobilization.
SCAPULA FRACTURES
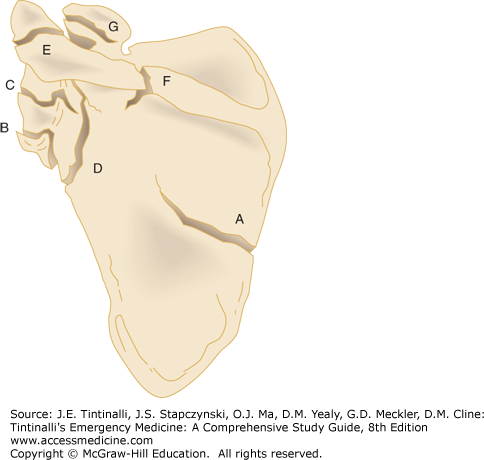
The scapula is a triangularly shaped, flat bone that links the axial skeleton to the upper extremity and stabilizes motion of the arm. It serves as the site of origin of the rotator cuff and muscles about the shoulder. The mechanism of injury usually is from high-energy trauma to the shoulder area or from a fall on an outstretched hand. Scapular fractures are classified by their anatomic location (Figure 271-4),13 with fractures of the body (Figure 271-5) and glenoid neck being most common.
Patients with isolated scapular fractures typically present with localized tenderness over the scapula and the arm held in adduction. Arm movement exacerbates pain. Due to the high energy typically required to fracture this protected bone, there is a high association of injuries to the ipsilateral lung, thoracic cage, and shoulder girdle, with fractures of the ribs being most common. Carefully determine the mechanism of injury to assist in diagnosis and raise suspicion for concurrent injuries. Assess the spine and pelvis, because scapular injuries often occur with high-impact trauma.13,14 The indirect axial load transmitted by a fall on an outstretched arm may result in a scapular neck fracture or glenoid fracture through shoulder impaction or dislocation.
Overlying structures may obscure a scapular fracture on a single trauma anteroposterior chest radiograph. A dedicated scapular series, including anteroposterior, lateral, and axillary scapular views, will identify most fractures and will guide the need for a CT scan (Figure 271-4). Scapular fractures are often associated with other significant injuries, and hence, diagnosis may be delayed or initially missed entirely. CT scan of the chest can identify both scapular and associated pathology, and a dedicated CT of the scapula can also be obtained.
Most scapular fractures are treated nonsurgically, with sling, ice, analgesics, and early range-of-motion exercises. Surgery may be necessary for significant or displaced articular fractures of the glenoid, angulated glenoid neck fractures, acromial fractures associated with a rotator cuff tear, and some coracoid fractures.13,15 Disability is more likely to be associated with fractures of the glenoid, acromion, or coracoid. Isolated scapular fractures should be referred to an orthopedic surgeon.
Traumatic dislocation of the scapula from the thoracic wall results from severe massive traction force applied to the ipsilateral upper extremity and shoulder girdle. Associated disruption of the subclavian or axillary arteries and brachial plexus makes proper identification and treatment critical.16,17
Chest x-ray demonstrates significant lateral displacement of the scapula.16,17 Associated radiographic abnormalities include distracted clavicle fracture, AC separation, and sternoclavicular dislocation. Perform a CT scan to identify intrathoracic injuries.
ACROMIOCLAVICULAR (AC) JOINT INJURIES
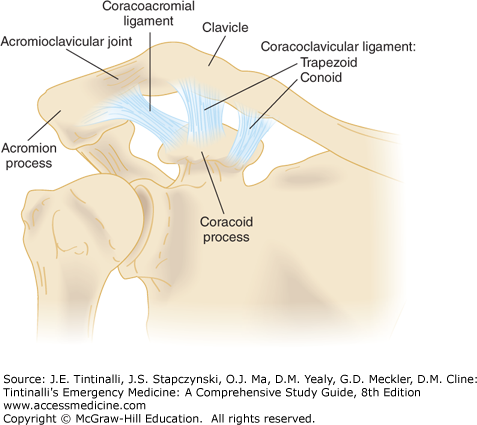
The AC joint is a diarthrodial joint that, together with the sternoclavicular joint, connects the upper extremity to the axial skeleton (Figure 271-6).
Support of the AC joint is through the AC and coracoclavicular ligaments and the attachment of the trapezius and deltoid muscles. Surrounding the AC joint is a thin capsule, which is reinforced by the AC ligaments. The AC ligaments provide horizontal stability to the joint. The strong coracoclavicular ligaments consist of two parts, the more lateral trapezoid and the medial conoid, and attach the distal inferior clavicle to the coracoid process of the scapula. The coracoclavicular ligament is the major suspensory ligament of the upper extremity and provides vertical stability to the AC joint.
AC joint injuries range from mild sprain to complete disruption of the ligaments that link the scapula and clavicle. The mechanism of injury is usually direct trauma to the joint from a fall with the arm adducted. The result is that the scapula and shoulder girdle are driven inferiorly while the clavicle remains in its normal position. An indirect mechanism is a fall on the outstretched hand with transmission of force to the AC joint.
The diagnosis of AC joint injuries is clinical. The mechanism of injury and tenderness and deformity at the AC joint, especially when compared with the contralateral AC joint, are confirmatory. Range of motion may be limited, depending on the severity of injury. Cross-arm abduction testing is often painful.
Radiographs are useful for identifying other fractures and determining the severity of injury. AC radiographs should specifically be ordered because they require only one-third to one-half of the penetration of standard shoulder films. Shoulder radiographs may overpenetrate the AC joint, and small fractures can be missed. Although standard AC radiographs are generally sufficient, an axillary view is required to identify posterior clavicular dislocation (type IV). Stress radiographs are no longer routinely obtained.18
Obtain emergency orthopedic consultation for open fractures, fractures with neurovascular injuries, and fractures with persistent skin tenting. Table 271-2 describes specific AC joint injuries. Treatment of type I and II injuries consists of rest, ice, analgesics, and immobilization, followed by early range-of-motion exercises (7 to 14 days).19
| Type | Injury | Mechanism | Radiograph/Exam |
|---|---|---|---|
| I | Sprained acromioclavicular ligaments |  | Radiograph: Normal Exam: Tenderness over acromioclavicular joint |
| II | Acromioclavicular ligaments ruptured; coracoclavicular ligaments sprained | 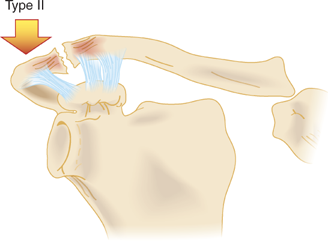 | Radiograph: Slight widening of acromioclavicular joint; clavicle elevated 25%–50% above acromion; may be slight widening of the coracoclavicular interspace Exam: Tenderness and mild step-off deformity of acromioclavicular joint |
| III | Acromioclavicular ligaments ruptured; coracoclavicular ligaments ruptured; deltoid and trapezius muscles detached | 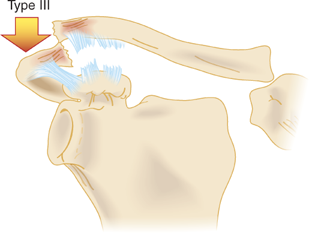 | Clavicle elevated 100% above acromion; coracoclavicular interspace widened 25%–100% Exam: Distal end of clavicle prominent; shoulder droops |
| IV | Rupture of all supporting structures; clavicle displaced posteriorly in or through the trapezius | 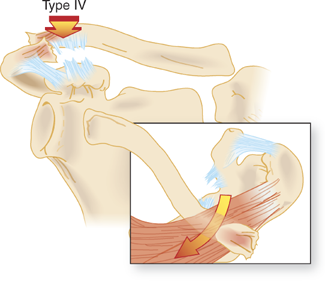 | Radiograph: May appear similar to type II and III; axillary radiograph required to visualize posterior dislocation Exam: Possible posterior displacement of clavicle |
| V | Rupture of all supporting structures (more severe form of type III injury) | 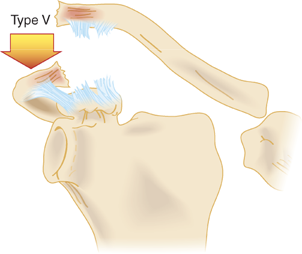 | Radiograph: Acromioclavicular joint dislocated; generally 200%–300% disparity of coracoclavicular interspace compared to normal shoulder Exam: More pain; gross deformity of clavicle |
| VI | Acromioclavicular ligaments disrupted; coracoclavicular ligaments may be disrupted; deltoid and trapezius muscles disrupted | 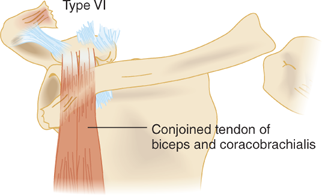 | Radiograph: Acromioclavicular joint dislocated; clavicle displaced inferiorly Exam: Severe swelling; multiple associated injuries |
A simple sling is the most convenient and effective initial treatment. Prognosis for type I and II injuries is excellent, with only a small percentage of patients developing late symptoms requiring excision of the distal clavicle.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree