Chapter 20 Shock
No matter the cause, shock can be defined as a clinical syndrome resulting from inadequate tissue perfusion. Despite clinical advancements in diagnostic methods and treatment, mortality from shock remains high; as many as 115,000 deaths annually in the United States can be attributed to shock.1 Emergency nurses play an essential role in the early recognition, diagnosis, and timely delivery of interventions for patients presenting to the ED in shock.
Pathophysiology
Shock can be classified according to the cause of inadequate tissue perfusion:
• Hypovolemic shock: inadequate tissue perfusion resulting from inadequate circulating volume
• Cardiogenic shock: inadequate tissue perfusion resulting from pump failure
• Distributive shock: inadequate tissue perfusion resulting from abnormal distribution of blood
• Obstructive shock: inadequate tissue perfusion resulting from obstruction of blood flow
The cascade of physiologic events and the progression of clinical decline are remarkably similar in all types of shock. The imbalance between the body’s demand for oxygen and the actual delivery of oxygen to the tissues results in impaired metabolism at the cellular level. A deadly cascade ensues, resulting in the following1:
• Accumulation of toxins and waste products within the cells leading to cell injury, inflammation, and death.
• Anaerobic metabolism leading to the production of lactic acid and the production of only 8 molecules of adenosine triphosphate (ATP) (as opposed to the production of 30 molecules of ATP with aerobic metabolism).
• Microvascular thrombosis and depletion of clotting factors
The end result is multiple organ failure and inevitable death of the patient.
Stages of Shock
The physiologic progression of shock can be categorized into three stages: compensated, uncompensated (progressive), and irreversible (refractory) shock.1
Compensated Shock
In the compensated stage, the clinical presentation of shock reflects the sympathetic nervous system’s response to decreased tissue perfusion. These compensatory mechanisms are generally quite effective and the clinician may not recognize the development of shock. Table 20-1 describes the physiologic responses seen during the compensated stage of shock.
TABLE 20-1 PHYSIOLOGIC RESPONSES DURING COMPENSATED SHOCK
| PHYSIOLOGY | RESPONSE |
|---|---|
| Sympathetic nervous system (SNS) | |
| Renin-Angiotensin-Aldosterone System | |
| Antidiuretic Hormone (ADH) Release | |
| Intracellular Fluid Shift | |
Uncompensated Shock
When the compensatory mechanisms are no longer able to maintain adequate tissue perfusion, the patient’s clinical situation begins to deteriorate. Signs and symptoms demonstrate the failure of compensatory mechanisms and the progression of the shock state. These changes are described in Table 20-2.
TABLE 20-2 PHYSIOLOGIC RESPONSES DURING UNCOMPENSATED SHOCK
| PHYSIOLOGY | RESPONSE |
|---|---|
| Altered Capillary Permeability | |
| Respiratory Insufficiency | |
| Cardiac Depression | |
| Tissue hypoperfusion | |
| Neurological Response | |
Monitoring the Patient in Shock
• The initial interventions to stabilize the patient in shock focus on insuring adequate airway, breathing, and circulation.
• Identifying the etiology of the shock state will help determine the most appropriate course of treatment.
• Ongoing assessment of cardiac rhythm, pulse oximetry, respiratory rate, and arterial blood pressure is essential in all patients suspected of a shock diagnosis.
• Trending of vital signs is crucial and identifies early physiologic changes.
• Mean arterial pressure (MAP) may provide a better indication of perfusion than either systolic or diastolic pressures. In the shock state, the goal is to maintain the MAP above 60 mm Hg.2
• Insertion of an arterial line is often necessary to accurately track BP measurement; the nurse needs to initially correlate the intraarterial pressure with a cuff pressure.
• Urine output is a reliable indicator of vital organ perfusion in the ongoing assessment of the shock patient.3
• Skin perfusion is assessed through pulse quality, skin temperature and moisture, and capillary refill.
• Level of consciousness is continually monitored as an indicator of cerebral perfusion.
• Invasive hemodynamic monitoring may be initiated in the ED.
• Central venous pressure (CVP) gives an indication of right-sided preload; pulmonary artery pressures reflect left-sided preload.
• Additionally, mixed venous saturation levels, drawn from either a central line (ScvO2) or the pulmonary artery catheter (SvO2) can be obtained to assess the amount of oxygen extracted from the blood by the tissues—an SvO2 of less than 60% indicates hypoperfusion.
• Measurements of base deficit and a lactate level are also important parameters to monitor.
Types of Shock
Hypovolemic Shock
Etiology
The common causes of hypovolemic shock include the following:
Signs and Symptoms
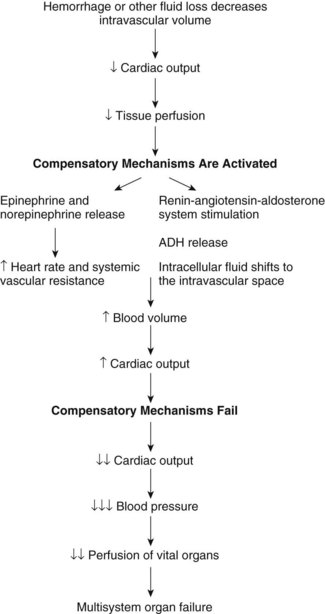
In hypovolemic shock, the size of the vascular compartment remains unchanged while the fluid volume diminishes. Reduced intravascular volume results in decreased venous return to the heart (preload) followed by a decrease in stroke volume and cardiac output. This series of events results in decreased tissue perfusion and impaired cellular metabolism. Figure 20-1 illustrates the pathway of hypovolemic shock development.
The body responds to acute hemorrhage by activating all major physiologic systems. The severity of clinical presentation and the interventions required are largely determined by the amount of fluid lost or shifted from the intravascular space because of injury. Fluid loss can be estimated by the type of injury. Table 20-3 lists estimated blood loss by site of injury.
TABLE 20-3 ESTIMATED BLOOD LOSS BY SITE OF INJURY
| INJURY | ESTIMATED BLOOD LOSS |
|---|---|
| Pelvis fracture | 3000 mL |
| Femur fracture | 1000 mL |
| Tibia fracture | 650 mL |
| Intra-abdominal injury | 2000 mL |
| Thoracic injury | 2000 mL |
Data from Emergency Nurses Association. (2009). Sheehy’s emergency nursing: Principles and practice (6th ed.). St. Louis, MO: Mosby.
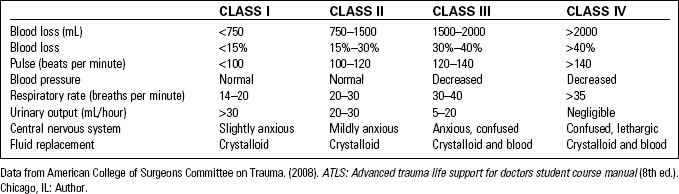
An estimation of volume loss and an assessment of vital signs, urine output, and mental status will assist the health care provider in determining the severity of hypovolemic shock. Age and preexisting medical conditions also play a role in the severity of the physiologic response to blood. Table 20-4 describes a classification of hypovolemic shock based on the amount of blood loss and the physiologic response.4
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree