SHOCK
FRAN BALAMUTH, MD, PhD, MSCE, JULIE FITZGERALD, MD, PhD, AND SCOTT L. WEISS, MD, MSCE
DEFINITION OF SHOCK
Normal circulatory function is maintained by a complex interplay between the central pump (heart) and blood flow at the regional level (microcirculation) for the purpose of delivering oxygen and nutrients to tissues and removing metabolic by-products (e.g., carbon dioxide). Shock can be defined as an acute syndrome of cardiovascular dysfunction in which the circulatory system fails to provide adequate oxygen and nutrients to meet the metabolic demands of vital organs. This definition recognizes that shock can and does exist without hypotension, especially in children. Furthermore, as knowledge of the pathophysiology of the shock state has evolved, it is now clear that inadequate cellular metabolism of oxygen and nutrients also contributes to the clinical manifestations and outcomes observed in patients with shock.
GOALS OF EMERGENCY THERAPY
All physicians who care for ill children will be faced with managing the clinical syndrome of shock. Many common childhood illnesses, such as trauma, gastroenteritis, infection, and accidental drug ingestions, can lead to shock. Ultimately, without timely medical intervention, the child in shock will follow a common pathway to multiorgan system failure and death. Early recognition and appropriate therapy are vital if we hope to reduce the morbidity and mortality associated with this serious syndrome.
The goals of emergency therapy in pediatric shock are threefold:
 Prompt recognition
Prompt recognition
 Shock reversal
Shock reversal
 Transfer to definitive care
Transfer to definitive care
This chapter is devoted to addressing each of these goals in turn. We begin with a discussion of clinical and pathophysiologic considerations in pediatric shock, followed by a description of different etiologic types of shock including hypovolemic, cardiogenic, obstructive, distributive (septic), and dissociative shock (Fig. 5.1). The remainder of the chapter is focused on pediatric shock recognition and clinical management including diagnostic testing, fluid resuscitation, vasoactive agent choice, source control, treatment of refractory shock, and transfer to definitive care. Because increasing evidence has accumulated indicating that care for patients with septic shock can be improved through the utilization of protocolized or bundled goal-directed therapy, we include a discussion on quality improvement initiatives utilizing a bundled approach for septic shock.
RELATED CHAPTERS
Resuscitation and Stabilization
• A General Approach to Ill and Injured Children: Chapter 1
Signs and Symptoms
• Septic Appearing Infant: Chapter 68
Clinical Pathways
• Fever in Infants: Chapter 87
Medical/Surgical/Trauma Emergencies
• Allergic Emergencies: Chapter 93
• Cardiac Emergencies: Chapter 94
• Infectious Disease Emergencies: Chapter 102
• Metabolic Emergencies: Chapter 103
• Toxicologic Emergencies: Chapter 110
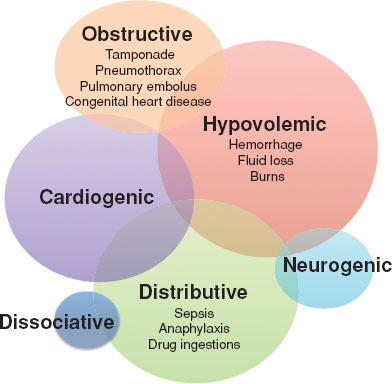
FIGURE 5.1 Etiologic types of shock. The size of each circle is proportional to the incidence of each shock type. Although distinct etiologies are evident, there is considerable overlap in the clinical presentation and underlying pathophysiology between categories.
CLINICAL AND PATHOPHYSIOLOGIC CONSIDERATIONS
Delivery of oxygen and nutrients is predominantly regulated by cardiac output and microvascular blood flow. Cardiac output is calculated by multiplying the stroke volume (volume of blood ejected by the left ventricle) by the heart rate (ejection cycles per minute). The stroke volume depends on the filling volume of the ventricle (preload), myocardial contractility and rhythm, and the systemic vascular resistance (SVR) against which the ventricle is pumping blood to the body (afterload). Heart rate, preload, contractility, rhythm, and afterload are regulated through a variety of neurohumoral and metabolic factors, including the sympathetic nervous system, endogenous catecholamine release, tissue pH and oxygen tension, nitric oxide, reactive oxygen species, and calcium homeostasis, that themselves respond to changes in blood volume, circulating inflammatory cytokines, and endothelial cell activation (Fig. 5.2). Infants require special consideration, as they have relatively little reserve myocardial contractility to increase stroke volume and thus depend almost exclusively on heart rate to increase cardiac output.
Blood pressure is determined by both cardiac output and SVR and is generally used as a clinical surrogate for tissue perfusion. While low blood pressure will reduce oxygen and nutrient delivery to tissues, the absence of hypotension in children should not be taken to mean that organ perfusion is adequate since efforts to compensate for changes in cardiac output and SVR may initially preserve blood pressure. Early signs of shock with a normal blood pressure, referred to as compensated shock, include tachycardia, mild tachypnea, slightly delayed capillary refill (more than 2 to 3 seconds), cool extremities, orthostatic changes in blood pressure or pulse, decreased urine output, and subtle changes in mental status (e.g., mild irritability or sleepiness). In some cases of distributive shock, such as sepsis or anaphylaxis, a fall in SVR due to peripheral vasodilation may lead to the findings of “bounding” pulses, flash capillary refill, and widened pulse pressure. In addition to these clinical signs, biochemical changes such as an increased base deficit or blood lactate level, may also signal diminished organ perfusion early in shock.
As shock continues, early compensatory mechanisms fail to maintain cardiac output and SVR and blood pressure falls. Shock with hypotension is referred to as uncompensated shock. In addition to hypotension, clinical signs include worsening tachycardia (or bradycardia in infants) and tachypnea, mottled skin, cold extremities, and markedly delayed capillary refill (>4 seconds). Tachypnea and respiratory distress may herald underlying pulmonary disease, but may also reflect an increase in minute ventilation (to decrease PaCO2) to compensate for an increasing metabolic acidosis. Signs of organ dysfunction are typically evident, including further alterations in mental status (agitation, confusion, lethargy, stupor), gastrointestinal ileus, azotemia, coagulopathy, thrombocytopenia, and hyperbilirubinemia.
All types of shock encompass some degree of absolute or functional hypovolemia. Absolute hypovolemia exists in cases of dehydration from fluid losses (e.g., diarrhea, severe emesis, hyperthermia), hemorrhage, and “third spacing” of fluid due to increased vascular permeability, as in sepsis. Functional hypovolemia exists when vascular capacity increases, as in septic shock, spinal cord injury, anaphylaxis, or certain medication effects. In addition to volume loss, microcirculatory dysfunction is characterized by a maldistribution of capillary blood flow and is common to all types of shock. Even with reestablishment of global circulation, the activation of inflammatory cytokines in response to pathogen-associated molecular patterns (PAMPs) from invading microorganisms in sepsis and danger-associated molecular patterns (DAMPs) from cell injury in trauma, as well as endothelial cell activation and microthrombi formation, leads to regional changes in blood flow within and across organ systems. This contributes to local tissue ischemia that fuels a vicious cycle of tissue injury and inflammation that can result in the multiorgan dysfunction syndrome (MODS). Furthermore, a second wave of reperfusion injury may occur due to an increase in oxidant and nitrogenous stress even after the primary insult of decreased tissue perfusion in shock is corrected.
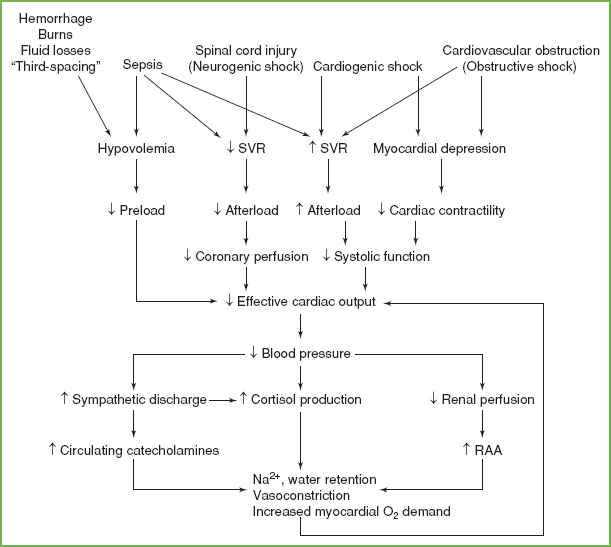
FIGURE 5.2 Sequence of cardiovascular derangements in shock states. Alterations in cardiac preload, afterload, and contractility decrease effective cardiac output, leading to several neurohumoral responses that attempt to restore organ perfusion. As the shock state progresses, these compensatory mechanisms fail to maintain effective cardiac output and clinical deterioration from compensated to uncompensated shock becomes evident.
The inability of cells to efficiently utilize oxygen to produce energy in the form of ATP has been termed “cytopathic hypoxia” and is largely attributable to mitochondrial bioenergetic dysfunction. The inability of mitochondria to use oxygen to sustain ATP production results in an energy deficit that can impair cellular metabolism and, ultimately, organ function. Mitochondrial dysfunction has been postulated to explain the increasingly recognized paradox of progressive organ injury following shock (particularly in sepsis and after trauma) despite minimal cell death even after restoration of tissue oxygen delivery.
TYPES OF SHOCK
Table 5.1 compares clinical findings by type of shock including some common examples.
Hypovolemic shock. Hypovolemia (decreased circulating blood volume) is the most common cause of shock in children. Volume losses from vomiting and diarrhea secondary to gastrointestinal infections are most prevalent etiology of hypovolemic shock worldwide. Other causes of hypovolemic shock include hemorrhage (trauma, postsurgical, gastrointestinal), plasma losses (burns, hypoproteinemia, pancreatitis), and extragastrointestinal water losses (glycosuric diuresis, heat stroke). Acute hypovolemia results in decreased cardiac output due to a fall in preload with a compensatory increase in heart rate and SVR. A fall in blood pressure detected within the baroreceptors of the carotid sinus leads to an increase in the sympathetic nervous system activity, stimulating cardiac chronotropy and vascular smooth muscle constriction as well as epinephrine release from the adrenal medulla. Upregulation of the renin–angiotensin–aldosterone (RAA) system and release of antidiuretic hormone (ADH) from the posterior pituitary gland promote sodium and water retention by the kidneys. Angiotensin II is also a direct vasoconstrictor, contributing to the observed increase in SVR.
Cardiogenic shock. The term cardiogenic shock is generally reserved for a decrease in cardiac output resulting from a decrease in myocardial contractility. Shock due to obstruction of blood flow from certain types of congenital heart lesions is better classified as obstructive shock (see below). Although myocardial depression can occur in all forms of shock, primary deficits in myocardial contractility leading to cardiogenic shock are caused by viral myocarditis, anomalous left coronary artery arising from the pulmonary artery (ALCAPA), incessant arrhythmias, drug ingestions (e.g., cocaine), metabolic derangements (e.g., hypoglycemia), and postoperative complications of cardiac surgery. Characteristic signs of cardiogenic shock are congestive heart failure, including pulmonary rales, a gallop cardiac rhythm, hepatomegaly, jugular venous distention, pitting peripheral edema, and cardiomegaly on chest radiograph. Laboratory findings of elevated creatine kinase, troponin, or brain natriuretic protein (BNP) levels may herald myocardial dysfunction, but are not universally present. As in hypovolemic shock, upregulation of the sympathetic nervous system, RAA system, and ADH, as well as the natriuretic peptides (BNP and atrial natriuretic peptide) raise SVR to compensate for a low cardiac output. Unlike hypervolemia, however, the volume deficit is functional (decreased effective circulating blood volume) rather than absolute (see Chapter 94 Cardiac Emergencies).
TABLE 5.1
CLINICAL CHARACTERISTICS BY TYPE OF SHOCK
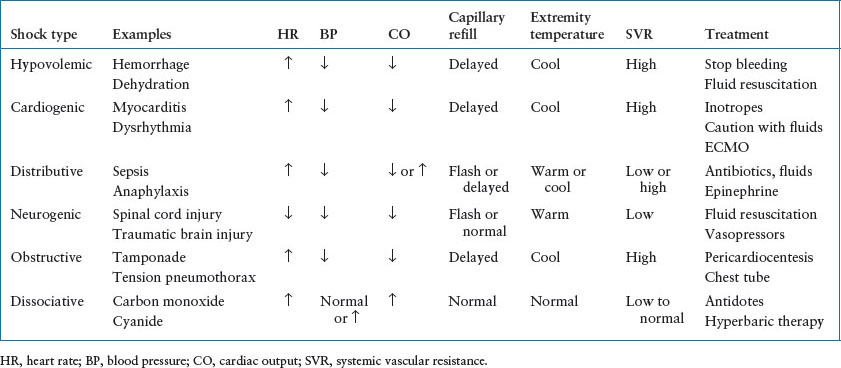
Obstructive shock. An acute mechanical obstruction to ventricular outflow can result in obstructive shock. Causes include proximal pulmonary embolus, cardiac tamponade, tension pneumothorax, and obstructive lesions of the left side of heart (hypertrophic left heart syndrome, aortic coarctation, interrupted aortic arch, and critical aortic valve stenosis). An acute increase in SVR results from a sudden decrease in cardiac output and functional hypovolemia. Rapid recognition of the cause of obstructive shock is critical in order to implement the correct therapy. Congenital heart lesions typically present at 1 to 3 weeks postnatal age, following closure of the ductus arteriosus.
Distributive shock. Distributive shock results from inappropriate vasodilation and pooling of blood in the peripheral vasculature. Common causes in children are sepsis, anaphylaxis, and drug ingestions (e.g., atypical antipsychotics). Rarely is distributive shock present without other types of shock, most notably hypovolemic shock.
Pediatric sepsis is defined as the systemic inflammatory response syndrome (SIRS), which includes either an abnormal temperature or leukocyte count along with tachycardia/bradycardia and/or tachypnea, in the presence of a confirmed or suspected invasive infection. Severe sepsis is defined as sepsis plus (1) cardiovascular dysfunction, (2) acute respiratory distress syndrome, or (3) ≥2 organ system dysfunctions. Septic shock refers to the subset of patients with cardiovascular dysfunction. In 2005, approximately 75,000 children were hospitalized with severe sepsis in the United States at $4.8 billion in healthcare costs and an estimated mortality of 8.9%. Although many patients who appear to have sepsis, severe sepsis, or septic shock have negative cultures, exposure to microbial components (e.g., endotoxin, lipoteichoic acid, viral proteins) is believed to trigger a cascade of inflammatory, coagulation, and vascular mediators that result in severe capillary leak (causing hypovolemia), myocardial depression, and vasomotor instability. Although classic septic shock results in hyperdynamic cardiac function and low SVR that manifest as “warm” shock, more than half of children with septic shock exhibit low cardiac output and elevated SVR, or “cold” shock.
In anaphylaxis, the sudden release of preformed histamine, proteases (tryptase, chymase), and proteoglycans (heparin) in mast cells followed by prostaglandins and leukotrienes leads to the classic symptoms of the skin and respiratory tract, as well as a profound vasodilatory response resulting in a low SVR state along with capillary leak causing hypovolemia. The resulting neurohumoral response leads to an increase in heart rate and contractility that raise cardiac output (see Chapter 93 Allergic Emergencies).
Neurogenic shock. Neurogenic shock is a special cause of distributive shock resulting from the sudden disruption of sympathetic nerve stimulation to the vascular smooth vessel leading to a profound decrease in SVR. Unlike other types of shock, the unopposed vagal activity classically results in bradycardia or, at least, absence of the usual tachycardic response to hypotension. Neurogenic shock can be seen following severe traumatic brain or cervical spine injury (see Chapter 120 Neck Trauma).
Dissociative shock. Dissociative shock is a special category of shock that occurs as a consequence to a toxic metabolite or drug that severely impairs cellular oxygen delivery or utilization despite sustained or supranormal tissue perfusion. Examples include severe anemia, methemoglobinemia, and carbon monoxide poisoning (see Chapter 110 Toxicologic Emergencies).
CLINICAL CONSIDERATIONS IN SHOCK RECOGNITION
An ongoing clinical challenge is the early recognition of children with compensated shock. We include here a detailed discussion about early septic shock recognition, but the principles discussed can be applied to multiple shock types. Because hypotension is a late finding in pediatric shock, children often present with tachycardia alone. Although adults have often used vital sign criteria based on the SIRS to identify patients with compensated shock, the high prevalence of SIRS in the pediatric emergency setting in patients without sepsis, as well as the overall rarity of sepsis in children with infectious illness, precludes using these vital sign–based criteria alone to recognize sepsis.
Vital Signs
Despite the challenges of identifying the pediatric patient with compensated septic shock, which is often described as “finding a needle in a haystack,” there is increasing interest from hospitals, professional medical societies, and legislative bodies to put systems in place to improve sepsis recognition. Vital sign–based sepsis alert systems that are embedded in the electronic medical record are one such mechanism. Although there is evidence that such alerts can improve the sensitivity of sepsis recognition, the use of such alerts must be accompanied by a detailed physician evaluation at the bedside. In addition, the impact of vital sign–based electronic alerts on sepsis overidentification, antibiotic overuse, and other balancing measures in the emergency department, remains to be fully evaluated.
History and Physical Examination Findings
In addition to vital signs, there are elements of history and physical examination that should be assessed to recognize compensated and decompensated shock.
Hypovolemic Shock
Hemorrhagic Shock. Determine by history whether there was possible trauma, and if so whether it was blunt or penetrating. The provider should also determine whether any source of bleeding was recognized prior to arrival (e.g., hematemesis, hemoptysis, vaginal bleeding, hematochezia). The emergency provider also needs to have a high index of suspicion for nonaccidental trauma in a child presenting in shock with no other preceding symptoms.
 Trauma or suspected trauma patients should undergo a full trauma evaluation including the primary and secondary surveys as detailed in Chapter 2 Approach to the Injured Child.
Trauma or suspected trauma patients should undergo a full trauma evaluation including the primary and secondary surveys as detailed in Chapter 2 Approach to the Injured Child.
 Careful evaluation for evidence of bleeding including assessment of open fontanelles, all orifices, and thorough abdominal examination.
Careful evaluation for evidence of bleeding including assessment of open fontanelles, all orifices, and thorough abdominal examination.
Dehydration. Determine if volume loss may be due to decreased intake or increased output (vomiting, diarrhea). On physical examination, one should assess the following:
 Mental status/level of activity
Mental status/level of activity
 Sunken fontanelle and/or eyes
Sunken fontanelle and/or eyes
 Skin turgor
Skin turgor
 Capillary refill
Capillary refill
 Urine output
Urine output
Cardiogenic shock. Cardiogenic shock is often difficult to distinguish from other shock states, as a prolonged history of worsening symptoms is less common in children as compared to adult heart failure. Historical information should be obtained regarding chest pain, syncope, known cardiac abnormalities, and cardiac medications. On physical examination, one should assess the following:
 Neck: Jugular venous distention
Neck: Jugular venous distention
 Cardiac: Murmur, gallop, perfusion abnormalities including delayed capillary refill, diminished or bounding pulses
Cardiac: Murmur, gallop, perfusion abnormalities including delayed capillary refill, diminished or bounding pulses
 Respiratory: Respiratory distress, rales to suggest pulmonary edema
Respiratory: Respiratory distress, rales to suggest pulmonary edema
 Abdomen: Hepatomegaly
Abdomen: Hepatomegaly
 Extremities: Peripheral edema, delayed capillary refill
Extremities: Peripheral edema, delayed capillary refill
Obstructive shock. On physical examination, one should assess the following:
 Neck: Jugular venous distention
Neck: Jugular venous distention
 Cardiac: Murmur, gallop
Cardiac: Murmur, gallop
 Respiratory: Unilateral decreased breath sounds suspicious for tension pneumothorax
Respiratory: Unilateral decreased breath sounds suspicious for tension pneumothorax
 Abdomen: Hepatomegaly
Abdomen: Hepatomegaly
 Extremities/skin: Poor perfusion, cyanosis in unrepaired congenital heart disease including differential perfusion, and cyanosis between the upper and lower extremities to indicate interrupted aortic arch or critical aortic coarctation
Extremities/skin: Poor perfusion, cyanosis in unrepaired congenital heart disease including differential perfusion, and cyanosis between the upper and lower extremities to indicate interrupted aortic arch or critical aortic coarctation
 Beck triad in cardiac tamponade: Distended neck veins, hypotension, diminished heart sounds
Beck triad in cardiac tamponade: Distended neck veins, hypotension, diminished heart sounds
Distributive Shock
Septic Shock.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree







