SHOCK
FRAN BALAMUTH, MD, PhD, MSCE, DEBRA A. POTTS, MSN, RN, CPEN, CEN, MARY KATE FUNARI, MSN, RN, CPEN AND JANE LAVELLE, MD
BACKGROUND (EPIDEMIOLOGY, EVIDENCE)
Pediatric sepsis syndrome is a leading source of morbidity, mortality, and healthcare costs in infants and children in the United States. In the United States, there are approximately 21,000 cases of severe sepsis requiring hospitalization annually with estimated mortality estimates from 5% to 20%. Timely antimicrobial therapy and fluid resuscitation is essential in the treatment of severe sepsis and septic shock. The Surviving Sepsis Campaign recommends antibiotic administration within 1 hour of recognition of septic shock, as well as prompt fluid resuscitation in both adults and children. In addition, timely sepsis care has been identified as a quality metric. Several pediatric institutions have successfully implemented protocol-based sepsis care and have demonstrated associated improvements in the timeliness of care delivery. These improvements have been associated with improved ICU and hospital length of stay. Recognizing which patient requires these intensive severe sepsis therapies remains a challenge. Ideally, sepsis recognition tools should be built with high sensitivity such that no patients with sepsis are missed, they should also have high specificity to avoid unnecessary antibiotic use and resource utilization. Because of the time-sensitive nature of sepsis interventions, implementing pediatric sepsis protocols in the emergency department settings requires strong teamwork and strong interdisciplinary collaboration.
PATHWAY GOALS AND MEASUREMENTS
Goals
 Improved identification of patients with severe sepsis
Improved identification of patients with severe sepsis
 Timely antibiotic therapy
Timely antibiotic therapy
 Timely fluid resuscitation
Timely fluid resuscitation
 Decrease patients in whom sepsis is diagnosed within 24 hours of admission
Decrease patients in whom sepsis is diagnosed within 24 hours of admission
Measurements
 Time to fluid management (40 mL per kg, 60 mL per kg)
Time to fluid management (40 mL per kg, 60 mL per kg)
 Time to first appropriate antibiotics, percent in <1 hour
Time to first appropriate antibiotics, percent in <1 hour
 Multisystem organ failure at 0, 24, 48 hours
Multisystem organ failure at 0, 24, 48 hours
Algorithm and Key Hyperlinks
 See Figure 91.1 (http://www.chop.edu/clinical-pathway/severe-sepsis-clinical-pathway-infants-28-days-age-and-children)
See Figure 91.1 (http://www.chop.edu/clinical-pathway/severe-sepsis-clinical-pathway-infants-28-days-age-and-children)
 See Tables 91.1 and 91.2
See Tables 91.1 and 91.2

FIGURE 91.1 Pathway for evaluation and treatment of infants >28 days of age and children with severe sepsis. Pathway Authors: F Balamuth, MD; MK Funari, RN; H Scott, MD; E Alpern, MD; D Davis, MD; M Mittal, MD; C Jacobstein, MD; J Gerber, MD; T Metjian, PharmD; J Lavelle, MD.
TABLE 91.1
PATIENT POPULATION/STRATIFYING PATIENT RISKS
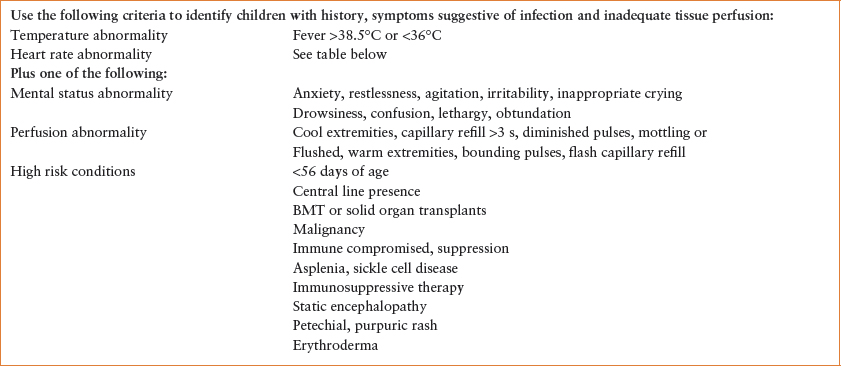
TABLE 91.2
VITAL SIGN TARGETS
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree







