INTRODUCTION
Sexually transmitted infections (STIs) are a major public health problem. In 2010, there were 1,307,893 cases of chlamydia infection, 309,341 cases of gonorrhea, and 45,834 cases of syphilis reported in the United States.1 The World Health Organization estimates that 500 million people are infected each year by a curable STI.2
The primary medical goals are identifying and treating STIs, but important secondary goals include preserving future health (including fertility), protection of any sexual contacts, preventive education, and provision of instructions for future screening. Lack of treatment can contribute to infertility, cancer, and urogenital complications. Failure of patients to follow up and adhere to a prescribed medical regimen complicates individual care and public health reduction efforts.
Multiple STIs frequently occur together. Once an STI is diagnosed, further testing for human immunodeficiency virus (HIV) infection and hepatitis B is warranted.3
Because of frequent changes in treatment guidelines and resistance patterns, we recommend that the reader access the Morbidity and Mortality Weekly Report (http://www.cdc.gov/mmwr) to check any modifications for treatment and also to obtain patient information in several languages.
GENERAL PRINCIPLES FOR DIAGNOSIS AND SCREENING
The signs and symptoms of an STI may be obvious, such as a genital lesion or vaginal discharge, or less specific, such as dysuria, lower abdominal pain, painful intercourse, or spotting and abnormal periods. Less specific signs lead to frequent ED STI underrecognition. Obtain a thorough sexual history in an objective, nonjudgmental manner to determine the risk of STI, HIV infection, or hepatitis. The young (13 to 24 years old), pregnant women, and homosexual men are all at higher risk of STI and subsequent morbidity. The Centers for Disease Control and Prevention have questions that providers can use when obtaining a sexual history and determining a patient’s risk for an STI (Table 149-1).
1. Partners
2. Prevention of pregnancy
3. Protection from STI
4. Practices
5. Past history of STI
|
Perform a pregnancy test in all females of childbearing potential, because pregnancy can affect treatment options. As appropriate, have chaperones present whenever breast, genital, or rectal examinations are performed. In women, perform a vaginal speculum examination, bimanual examination, and rectal examination. In males, retract the foreskin in uncircumcised patients to fully examine the area. Examine the areas between skinfolds, particularly in obese patients. Obtain directed site test specimens, which may include urine, vaginal, rectal, and urethral samples.
GENERAL RECOMMENDATIONS FOR TREATMENT AND FOLLOW-UP
Based on advice from the Centers for Disease Control and Prevention, we recommend the following3,5 (Table 149-2):
| Sexually Transmitted Infection | First-Line Treatment | Alternative(s) | Pregnancy/Lactation |
|---|---|---|---|
| Bacterial vaginosis | Metronidazole, 500 milligrams PO two times daily × 7 d | Tinidazole, 2 grams PO daily × 3 d | Metronidazole, 500 milligrams PO two times daily × 7 d |
| or | or | ||
| Metronidazole vaginal gel 0.75%, 5 grams intravaginally daily × 5 d | Tinidazole, 1 gram PO daily × 5 d | ||
| or | or | ||
| Clindamycin vaginal cream 2%, 5 grams intravaginally at bedtime × 7 d | Clindamycin, 300 milligrams PO twice daily × 7 d | ||
| or | |||
| Clindamycin ovule, 100 milligrams intravaginally at bedtime × 3 d | |||
| Chancroid | Azithromycin, 1 gram PO single dose | Azithromycin, 1 gram PO single dose | |
| or | or | ||
| Ceftriaxone, 250 milligrams IM single dose* | Ceftriaxone, 250 milligrams IM single dose* | ||
| or | |||
| Ciprofloxacin, 500 milligrams PO, two times daily × 3 d | |||
| or | |||
| Erythromycin base, 500 milligrams PO three times daily × 7 d | |||
| Chlamydia (treat for Neisseria gonorrhoeae concurrently) | Azithromycin, 1 gram PO single dose | Erythromycin base, 500 milligrams PO four times daily × 7 d | Azithromycin, 1 gram PO single dose |
| or | or | or | |
| Doxycycline, 100 milligrams PO two times daily × 7 d | Erythromycin ethylsuccinate, 800 milligrams PO four times daily × 7 d | Amoxicillin, 500 milligrams PO three times daily × 7 d | |
| or | or | ||
| Levofloxacin, 500 milligrams PO once daily × 7 d | Erythromycin base, 500 milligrams PO four times a day for 7 d | ||
| or | or | ||
| Ofloxacin, 300 milligrams PO twice daily × 7 d | Erythromycin base, 250 milligrams PO four times a day for 14 d | ||
| or | |||
| Erythromycin ethylsuccinate, 800 mg orally four times a day for 7 d | |||
| or | |||
| Erythromycin ethylsuccinate, 400 mg orally four times a day for 14 d | |||
| Gonorrhea (treat for Chlamydia trachomatis concurrently) | Ceftriaxone*, 250 milligrams IM single dose AND azithromycin, 1 gram PO single dose | Cefixime, 400 milligrams PO single dose AND azithromycin, 1 gram PO single dose | Ceftriaxone*, 250 milligrams IM single dose AND azithromycin, 1 gram PO single dose |
| or | or | or | |
| Ceftriaxone*, 250 milligrams IM single dose AND doxycycline, 100 milligrams PO twice a day for 7 d | Cefixime, 400 milligrams PO single dose AND doxycycline, 100 milligrams PO twice a day for 7 d | Cefixime, 400 milligrams PO single dose AND azithromycin, 1 gram PO single dose | |
| or | or | ||
| Azithromycin, 2 grams PO single dose AND test-of-cure in 1 week | Azithromycin, 2 grams PO single dose AND test-of-cure in 1 week | ||
| or | |||
| Spectinomycin 2 grams IM single dose | |||
| Granuloma inguinale (donovanosis) | Doxycycline, 100 milligrams PO two times daily for at least 3 weeks until lesions completely healed | Azithromycin, 1 gram PO weekly for at least 3 weeks until lesions completely healed | Erythromycin base, 500 milligrams PO four times daily for at least 3 weeks until lesions completely healed |
| or | or | ||
| Granuloma inguinale (donovanosis) (continued) | Ciprofloxacin, 750 milligrams PO two times daily for at least 3 weeks until lesions completely healed | Azithromycin, 1 gram PO weekly for at least 3 weeks until lesions completely healed | |
| or | or | ||
| Erythromycin base, 500 milligrams PO four times daily for at least 3 weeks until lesions completely healed | Gentamicin 1 milligram/kg IV every 8 hours (if the above therapy is ineffective) | ||
| or | |||
| Trimethoprim-sulfamethoxazole, double-strength (160/800 milligrams) PO two times daily for at least 3 weeks until lesions completely healed | |||
Herpes simplex First episode | Acyclovir, 400 milligrams PO three times daily × 7–10 d | Acyclovir, 400 milligrams PO three times daily × 7–10 d | |
| or | or | ||
| Acyclovir, 200 milligrams PO five times daily × 7–10 d | Acyclovir, 200 milligrams PO five times daily × 7–10 d | ||
| or | or | ||
| Famciclovir, 250 milligrams PO three times daily × 7–10 d | Valacyclovir, 1 gram PO two times daily × 7–10 d | ||
| or | |||
| Valacyclovir, 1 gram PO two times daily × 7–10 d | |||
| Recurrent or suppressive therapy for patients without HIV | Valacyclovir, 500 milligrams daily if >9 episodes/year | Acyclovir, 400 milligrams orally three times a day for 5 d | |
| or | or | ||
| Valacyclovir, 1 gram PO daily × 5 d | Valacyclovir 1 PO daily × 5d | ||
| Severe | Acyclovir, 5–10 milligrams/kg IV every 8 h × 2–7 d then oral meds for total treatment time of 10 d | Acyclovir, 5–10 milligrams/kg IV every 8 h × 2–7 d then oral meds for total treatment time of 10 d | |
| or | |||
| Valacyclovir, 500 milligrams PO once per day | |||
| Lymphogranuloma venereum | Doxycycline, 100 milligrams PO two times daily × 21 d | Erythromycin base, 500 milligrams PO four times daily × 21 d | Erythromycin base, 500 milligrams PO four times daily × 21 d |
Syphilis Primary, secondary, and early latent | Benzathine penicillin G, 2.4 million units IM single dose | Doxycycline, 100 milligrams PO two times daily × 14 d | Benzathine penicillin G, 2.4 million units IM single dose |
| or | |||
| Tetracycline, 500 milligrams PO four times daily × 28 d | |||
| or | |||
| Ceftriaxone, 250 milligrams IM or IV daily × 10–14 d (early syphilis) | |||
| or | |||
| Azithromycin, 1 gram PO single dose (early syphilis) | |||
| Latent | Benzathine penicillin G, 2.4 million units IM one time a week × 3 weeks | Doxycycline, 100 milligrams PO two times daily × 28 d | |
| or | |||
| Tetracycline, 500 milligrams PO four times daily × 28 d | |||
| Trichomoniasis | Metronidazole, 2 grams PO single dose | Metronidazole, 500 milligrams PO two times daily × 7 d | Metronidazole, 2 grams PO single dose (only if symptomatic) |
| or | or | ||
| Tinidazole, 2 grams PO single dose | If asymptomatic, deferral of treatment until after 37 weeks | ||
| Consider withholding breastfeeding until 12–24 h after last dose |
When an STI is suspected, especially for gonorrhea and chlamydia infection, treat the patient in the ED with single-dose antibiotic regimens.
Obtain a pregnancy test and consult or refer promptly if the patient is pregnant.
If one STI is suspected or diagnosed, screen for other STIs (HIV infection, syphilis, and hepatitis) in the ED or through follow-up.
Report any notifiable infections such as Chlamydia trachomatis, gonorrhea, HIV infection, and syphilis. This is often based on final laboratory testing and can be automated.
Counsel all patients with suspected STIs about prevention and co-infection risks (notably HIV and hepatitis) in the ED and ensure follow-up options. Although no method aside from abstinence is 100% effective for STI prevention, male latex condoms and female condoms are useful in preventing STIs.
Advise that the partner(s) must seek treatment before any reengagement in sex.
Arrange follow-up to ensure relief of symptoms, compliance, and STI cure.
Although the Centers for Disease Control and Prevention recommend that health care providers in all settings routinely screen for HIV infection in all patients aged 13 to 64 years, the ED remains an underused venue for HIV screening.6 Rapid HIV testing in the ED is not routine but is becoming more prevalent.7
SEXUALLY TRANSMITTED INFECTIONS PRESENTING WITH URETHRITIS, CERVICITIS, AND/OR DISCHARGE
In the United States and the United Kingdom, C. trachomatis infection is the most frequently reported STI. It is one of the causes of nongonococcal urethritis and commonly coexists with gonorrhea infections. It is most prevalent in people <25 years of age and is frequently asymptomatic, especially in women.7
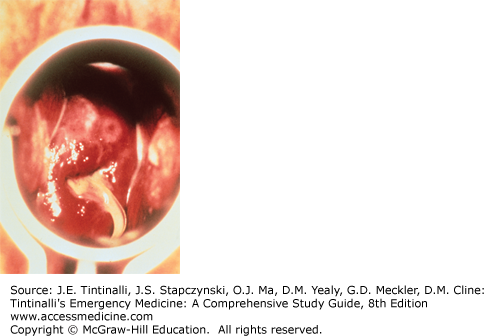
Chlamydial infections in men can cause urethritis, epididymitis, proctitis, or Reiter’s syndrome (urethritis, conjunctivitis, and rash). Women generally have asymptomatic cervicitis when infected with Chlamydia, although if present, symptoms include vaginal discharge, bleeding between menses, and dysuria. The discharge may be mucopurulent (Figure 149-1) when Neisseria gonorrhoeae is a co-infectant. Consider urethral chlamydial infection in the differential diagnosis of sterile pyuria. Complications in women include pelvic inflammatory disease, ectopic pregnancy, and infertility.
FIGURE 149-1.
Viscous, opaque discharge emanating from the cervical os, consistent with mucopurulent cervicitis. The string from an intrauterine device is seen descending through the os in this patient. [Reproduced with permission from Knoop KJ, Stack LB, Storrow AB, Thurman RJ: The Atlas of Emergency Medicine, 3rd ed. © 2009 by McGraw-Hill, Inc., New York.]
Nonculture methods of detection, such as direct immunofluorescence, enzyme-linked immunosorbent assays, nucleic acid hybridization tests, and nucleic acid amplification testing (NAAT), are preferred tests for diagnosis. NAAT has a high sensitivity (90%) and specificity (99%) for Chlamydia. NAAT is approved by the U.S. Food and Drug Administration for urine testing, and some tests are approved for use with vaginal specimens.
The Centers for Disease Control and Prevention recommend single-dose azithromycin or twice-a-day doxycycline for 7 days.9 Table 149-2 lists dosages and alternative treatment options.3 Azithromycin is safe for pregnant women, and pregnant women should undergo a test of cure 3 to 4 weeks after treatment. Amoxicillin is a safe alternative in pregnancy if azithromycin cannot be given.
Refer partners for testing and treatment if there was sexual contact in the last 60 days. Some providers choose to have the patient deliver treatment to their partners—endorsed by the Centers for Disease Control and Prevention—as a way of preventing the spread of this STI. Universal adoption of this method at this time is incomplete because of ethical issues and medicolegal consequences including some state prohibitions.10
Counsel patients to avoid sexual contact until 7 days have elapsed after completion of antibiotic treatment and their symptoms have resolved. Encourage women to be retested approximately 3 months after treatment because of the high incidence of recurrence.3
Gonorrhea is the second most commonly reported STI, caused by N. gonorrhoeae, a gram-negative diplococcus.
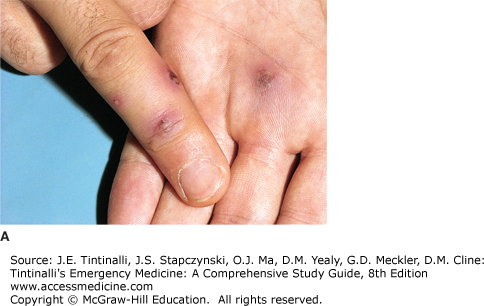
Most gonococcal infections in women are asymptomatic, and many coexist with chlamydial infection. Subclinical gonorrheal infections result in complications ranging from ectopic pregnancy to chronic pelvic pain to pelvic inflammatory disease.8,9 Women who are symptomatic from a gonoccal infection tend to present with nonspecific lower abdominal discomfort and mucopurulent cervicitis after a 7- to 14-day incubation period. Eighty percent to 90% of men develop symptoms within 2 weeks of exposure. In men, dysuria and profuse, purulent penile discharge (Figure 149-2) are the most common presenting symptoms, but symptoms of acute epididymitis and prostatitis may result in an ED visit. Rectal infection with mucopurulent anal discharge and pain occurs in 30% to 50% of women with gonococcal cervicitis, and the rectum can be the only site of infection in homosexual men. N. gonorrhoeae also can be isolated from the pharynx but rarely causes pharyngitis.
FIGURE 149-2.
Gonococcal urethritis in a male. Mucopurulent ureteral discharge is caused by infection with Neisseria gonorrhoeae. [Reproduced with permission from Goldsmith LA, Katz SI, Gilchrest BA, et al: Fitzpatrick’s Dermatology in General Medicine, 8th ed. © 2012 by McGraw-Hill Inc., New York.]
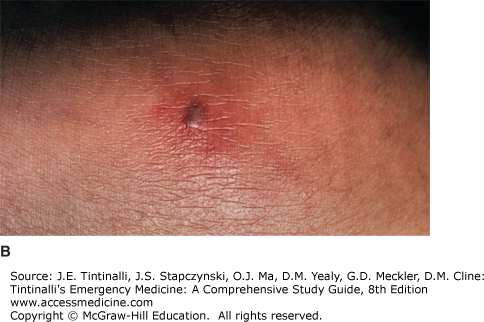
Signs and symptoms of disseminated gonococcemia are petechial or pustular acral skin lesions on an erythematous base (Figure 149-3), asymmetric arthralgias, tenosynovitis or septic arthritis, and fever or general malaise. Infection with N. gonorrhoeae and other STIs is associated with increased HIV shedding.11
The Centers for Disease Control and Prevention recommend that NAAT be performed on cervical, vaginal, urethral, or urine specimens. Specimens can be self-collected by the patient. Not all NAAT is the same; some tests can be used only on certain specimen types, so know what is available at your institution. Culture and nucleic acid hybridization tests require endocervical or urethral swab specimens.
In men, a Gram-stained specimen with the classic intracellular diplococci and polymorphonuclear leukocytes confirms the diagnosis. This diagnostic method is not recommended as a screening tool for asymptomatic men and is not sufficient for endocervical, pharyngeal, or rectal specimens. Diagnosis of disseminated gonococcal infection is difficult, with only 20% to 50% of cultures of blood, lesion, and joint specimens yielding positive results. Culture of cervical, rectal, and pharyngeal specimens may improve the chance of diagnosis.
Given emerging resistance patterns, the Centers for Disease Control and Prevention recommend dual therapy with ceftriaxone 250 milligrams IM or cefixime 400 milligrams PO plus either azithromycin 1 gram or doxycycline 100 milligrams PO twice a day for 7 days for the treatment of gonorrhea (Table 149-2
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree