INTRODUCTION
INFLUENZA
Human influenza is caused by a large, single-stranded RNA virus from the orthomyxovirus family. Influenza A and Influenza B cause the majority of human infections, with influenza A typically being more serious. Other viruses can cause similar febrile respiratory syndromes, including the coronaviruses linked to severe acute respiratory syndrome and Middle Eastern respiratory syndrome, both emanating from limited geographic areas and associated with high mortality.
Influenza is highly infectious and is transmitted via aerosolized respiratory secretions, large droplets, or fomites. Seasonal influenza has varying severity, typically striking in the winter months of temperate climates. Seasonal disease causes 250,000 to 500,000 annual deaths worldwide and between 5000 and 50,000 deaths in the United States. Outbreaks spread quickly throughout a community, largely among school-age children. Mortality occurs mostly among the elderly and young infants.
New strains occasionally emerge that can lead to pandemics. The 1918 influenza pandemic killed between 50 and 100 million people worldwide, and the potential for devastation by a novel influenza virus drives anxiety among clinicians and public health personnel. Unlike seasonal influenza, mortality during pandemics occurs mostly among healthy adults. In 2009, a pandemic H1N1 strain emerged in Mexico and followed this pattern, reminding us about the potential danger. A highly pathogenic avian strain of influenza emerged in 1997 in China, which was transmitted from infected chickens to humans. A variety of other animal strains of influenza have since been detected. These remain primarily bird viruses that have not developed the ability for efficient human-to-human transmission.
Influenza is transmitted by respiratory secretions, usually by sneezing or coughing, and via touching hands. The incubation period is typically 1 to 4 days. Influenza viruses undergo minor variations (antigenic drift) in their surface antigens that allow the virus to reinfect individuals and reemerge each winter. Occasionally, there are major antigenic changes (antigenic shift) that increase population susceptibility and lead to a pandemic.
Patients with influenza typically present with an abrupt onset of fevers and respiratory symptoms. Most cases are self-limited; however, some patients, particularly the elderly, the very young, and those with comorbid conditions, require hospitalization or die from complications of influenza. Additionally, influenza can lead to exacerbations of chronic medical conditions, such as congestive heart failure or chronic obstructive lung disease. Delirium is common in the elderly.
Pneumonia complicates some influenza infections. Primary influenza pneumonia develops quickly and progresses to acute respiratory distress syndrome, often within 24 hours. Bacterial super-infections also occur. Classically, influenza is associated with secondary Staphylococcus aureus pneumonia and, more recently, with community-acquired methicillin-resistant S. aureus.
Most cases of influenza are diagnosed clinically when a patient presents with fever, aches, and cough with influenza virus circulating in the community. However, clinical features of influenza overlap with other respiratory infections; laboratory confirmation can occasionally be helpful in patient care and infection control, especially before influenza has been documented in the community.
Rapid antigen assays identify the surface proteins in influenza A and B. These tests are simple to perform and give results within 15 minutes. However, they can have a low sensitivity, with ranges between 10% and 80% reported in clinical use. Specificity of these tests is between 90% and 95%, so a positive test indicates high likelihood of influenza, especially during an outbreak.
Molecular diagnostic tests, such as polymerase chain reaction for nucleic acids, are available and are more sensitive and specific than antigen tests. They are recommended for patients hospitalized with influenza.1 Several rapid polymerase chain reaction–based tests return results within the time frame of an ED visit, although they are more costly than rapid antigen tests.
The majority of patients will have a self-limited, uncomplicated illness requiring only symptomatic care. Patients with more severe influenza may benefit from IV fluids, respiratory support, and occasionally vasopressors. Those with pneumonia should be treated with antibiotics, targeting methicillin-resistant S. aureus if severe pneumonia exists.
The benefits of neuraminidase inhibitors for otherwise healthy adults and children are debated;2 the Centers for Disease Control and Prevention recommend treating higher risk populations. Studies of neuraminidase inhibitors for influenza in uncomplicated cases note benefits limited to patients treated within 48 hours of symptom onset. Antiviral treatment can also benefit patients hospitalized with influenza or bacterial complications of influenza, even if started after 48 hours of illness. Consider empiric antiviral treatment for patients with severe or progressive illness and those with higher risk of complications (Table 153-1). Oseltamivir is the most widely used neuraminidase inhibitor (75 milligrams twice daily for 5 days), with longer treatment for critically ill patients. Extracorporeal membrane oxygenation aids those with severe cardiorespiratory dysfunction, especially in pandemic settings where younger patients are afflicted.
Children younger than age 2 years Adults age 65 years and older Patients with comorbid conditions Immunosuppressed Pregnant patients Patients younger than 19 years receiving long-term aspirin American Indians/Alaskan natives Morbidly obese patients Residents of nursing homes and long-term care facilities |
HERPES SIMPLEX VIRUS INFECTIONS
Herpes simplex virus type 1 (HSV-1) and herpes simplex virus type 2 (HSV-2) are related double-stranded DNA viruses that cause oral and genital infections; rarely, these create devastating CNS disease. Herpes simplex infections are treatable with antiviral drugs, making early recognition of serious infection important.
HSV is common throughout the world. Transmission occurs when a susceptible individual is exposed to the virus. HSV-1 is usually acquired during childhood through nonsexual contact; HSV-2 is almost always sexually transmitted (see chapter 149, “Sexually Transmitted Infections”). HSV-1 seroprevalence varies by socioeconomic status, age, and geographic location. More than 50% of the U.S. population is seropositive for HSV-1, and 15.7% is seropositive for HSV-2.4 Rates are higher in developing countries. HSV-1 is one of the most common viral causes of encephalitis in the United States. It occurs most commonly in patients <20 years and >50 years of age.5 The mortality rate for untreated disease is >70%.
Neonates with HSV infection have a high frequency of both visceral involvement and CNS disease. Encephalitis in neonates is most often caused by HSV-2, which is acquired from the maternal genital tract at the time of delivery. The risk is highest when the mother acquires the infection in the third trimester.
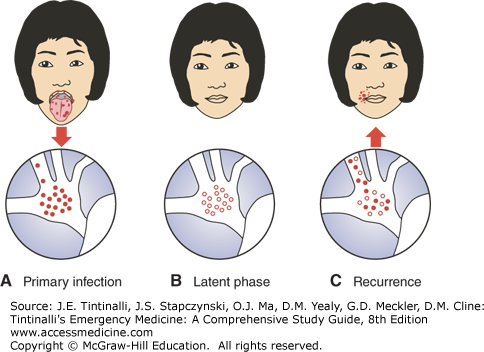
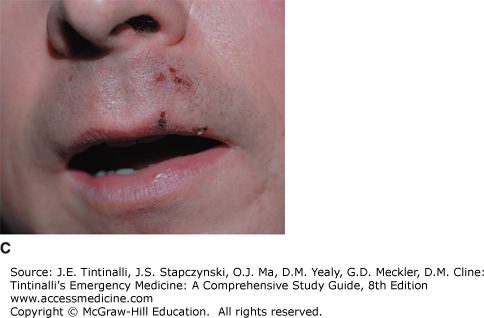
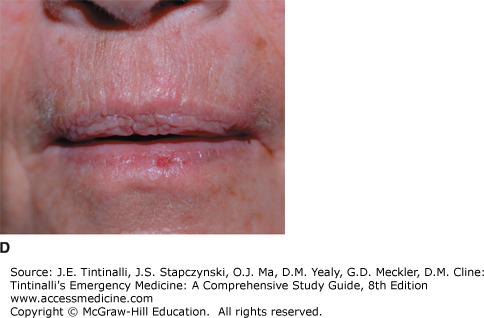
HSVs are transmitted through contact with persons with ulcerative lesions or by those who are shedding the virus by the exchange of saliva, vesicle fluid, semen, and cervical fluid. The virus must come in contact with a mucosal surface or abraded skin, where it replicates and causes localized symptoms before becoming latent in the sensory ganglia. HSV-1 typically resides in the trigeminal ganglia, and HSV-2 is found in the sacral ganglia. Reactivated virus travels to the cutaneous surface and results in localized vesicular eruptions (Figure 153-1).
In herpes simplex encephalitis, the virus is thought to gain access to the brain by the olfactory or the trigeminal nerve, with a predilection for the medial and inferior temporal lobes of the brain.
Most healthy hosts are able to control the virus and limit its replication to mucosal surfaces. Rarely during primary infection, the virus can spread beyond the local dorsal root ganglia and cause more widespread involvement. Multiorgan disease is much more common in the immunosuppressed and in neonates.
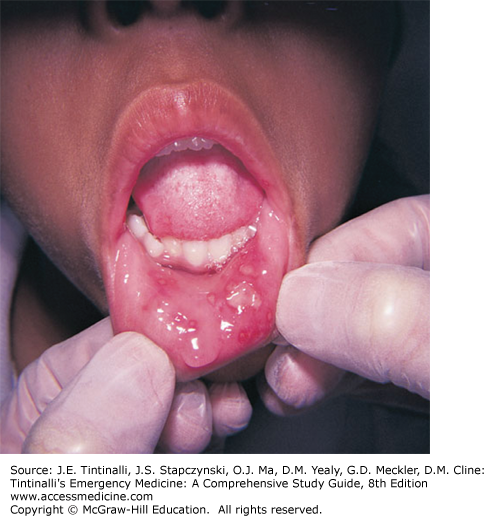
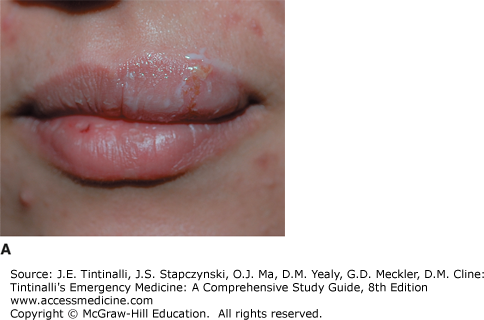
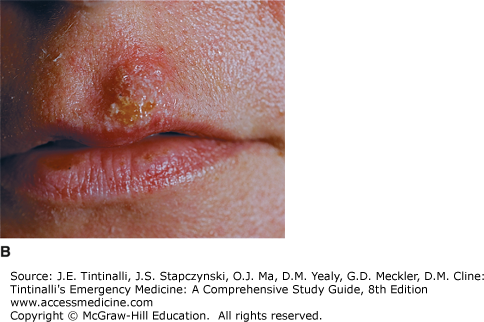
HSV infections occur year round. Symptoms of HSV depend on multiple factors, including the anatomic site involved, the immune status of the host, virus type, and whether the infection is primary or recurrent. Most HSV infections are subclinical. Symptomatic HSV-1 infection most commonly results in recurrent orolabial lesions, whereas HSV-2 is most often implicated in genital herpes. Primary infections typically produce more extensive lesions involving mucosal and extramucosal sites, often accompanied by systemic signs and symptoms. Gingivostomatitis and pharyngitis are typical manifestations of primary HSV-1 infection (Figure 153-2), and recurrence presents as herpes labialis (Figure 153-3). Less common skin manifestations include herpetic whitlow and herpes gladiatorum (skin). Eczema herpeticum (see Figure 251-14) can occur in patients with atopic dermatitis. Bell’s palsy may result from latent HSV-1 in the geniculate ganglia (see chapter 172, “Acute Peripheral Neurologic Disorders”). Herpetic keratitis presents as a painful, red eye, and can be identified by characteristic dendritic lesions on fluorescein slit lamp exam. HSV-1 and HSV-2 can cause identical genital lesions. Genital HSV-2 is more common and has a higher relapse rate, but the proportion of genital disease caused by HSV-1 is increasing.4 Primary genital infections can present with aseptic meningitis, which is a complication more common in women.
The hallmark of HSV encephalitis is acute onset of fever and neurologic symptoms. Patients can present with hemiparesis, cranial nerve abnormalities, ataxia, focal seizures, and altered mental status or behavioral abnormalities. It can be difficult clinically to distinguish HSV encephalitis from other types of meningoencephalitis. Meningitis occurs in up to 25% of females with primary HSV-2 infections. HSV-2 meningitis, unlike encephalitis, has a benign course, and patients recover uneventfully. Some patients develop recurrent lymphocytic meningitis (Mollaret’s syndrome).
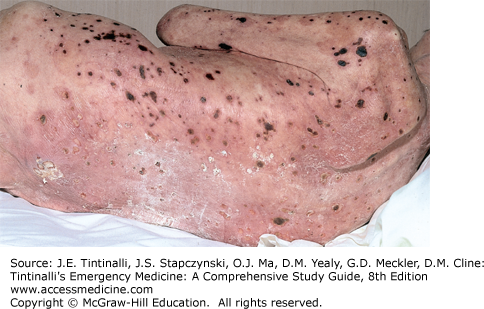
HSV infections in immunocompromised hosts can lead to widespread dissemination with multiorgan involvement (Figure 153-4). Organ transplant patients may develop esophagitis, hepatitis, colitis, and pneumonia (see chapter 297, “The Transplant Patient”). Severely burned patients are also prone to potentially fatal disease. HSV infections can also cause immune-mediated manifestations such as erythema multiforme, hemolytic anemia, and thrombocytopenia.
FIGURE 153-4.
Disseminated herpes simplex in an immunocompromised host. The rash of disseminated herpes simplex begins as vesicular lesions on an erythematous base, which may umbilicate and may blister and crust over as seen here. [Reproduced with permission from Wolff K, Johnson RA: Fitzpatrick’s Color Atlas and Synopsis of Clinical Dermatology, 5th ed., © 2005 by McGraw-Hill, Inc., New York.]
The preferred diagnostic test for confirmation of suspected HSV infection depends on the presentation. Because mucocutaneous infection is lifelong, we recommend laboratory confirmation of the clinical diagnosis. A specimen for viral culture can be obtained from the fluid of an unroofed vesicle. The sensitivity of culture is highest in the early stages and in primary disease. Polymerase chain reaction testing or a direct fluorescent antibody test can be performed on swabbed tissue. A Tzanck test is generally not useful.
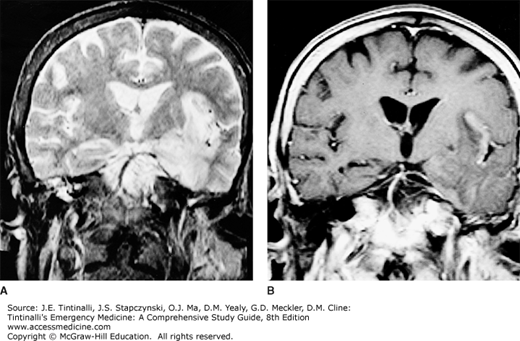
Identification of temporal lobe lesions on CT scan or MRI is strongly suggestive of HSV encephalitis (Figure 153-5). An electroencephalogram shows typical intermittent, high-amplitude slow waves localized to the temporal lobes.
FIGURE 153-5.
MRI scans showing hyperintensity involving the left temporal lobe and insular cortex in herpes simplex encephalitis. A. T2-weighted coronal MRI scan in the axial plane, taken during the acute stage of the illness. There is increased signal from practically all of the inferior and deep temporal lobe and the insular cortex. B. T1-weighted image after gadolinium infusion showing enhancement of the left insular and temporal cortices and early involvement of the right temporal lobe. [Reproduced with permission from Ropper AH, Samuels MA: Adams and Victor’s Principles of Neurology, 9th ed., © 2009 by McGraw-Hill Inc., New York.]
Cerebrospinal fluid analysis typically shows a lymphocytic pleocytosis with the presence of red blood cells. However, some patients can have normal cerebrospinal fluid parameters. Polymerase chain reaction testing of the cerebrospinal fluid is the testing modality of choice for HSV meningoencephalitis, with high sensitivity and specificity.5 Viral DNA can be detected within the first 24 hours, and results remain positive for a week or longer. To perform this test, most laboratories need an additional 0.5 to 1.0 mL of fluid beyond that required for standard analysis. Brain biopsy is reserved for difficult cases and for investigation of alternative diagnoses.
Treatment depends on the severity of the disease and the immune status of the patient (see chapter 149, “Sexually Transmitted Infections”). IV acyclovir is the drug of choice in patients with HSV encephalitis or disseminated disease and in immunocompromised patients with severe mucocutaneous disease (Table 153-2). Valacyclovir is a prodrug of acyclovir with higher bioavailability. Famciclovir and valacyclovir require fewer doses per day.
| Infection | Drug | Dosage | Duration |
|---|---|---|---|
| Mucocutaneous HSV infections in immunocompromised patients | Acyclovir | 5 milligrams/kg IV every 8 h | 7–14 d |
| Valacyclovir | 500 milligrams–1 gram PO twice per day | ||
| Famciclovir | 500 milligrams PO twice per day | ||
| Herpes simplex encephalitis | Acyclovir | 10–15 milligrams/kg IV every 8 h | 14–21 d |