Chapter 21 Sepsis
Sepsis is a progressive syndrome that leads to dysfunction and dysregulation of the body. Despite early identification, treatments, and aggressive interventions, mortality remains 20% to 50% for those patients who progress to severe sepsis or septic shock.1,2 Sepsis has no boundaries and can affect any age, gender, or race.3 Severe sepsis and septic shock are responsible for one in four deaths internationally and the incidence is increasing.1–7
Deaths resulting from sepsis exceed those from myocardial infarction, breast cancer, and stroke.8 Evidence-based studies indicate that early recognition, diagnosis, and treatment of sepsis in the emergency department (ED) will improve patient outcomes and decrease mortality. Early goal-directed therapy is a protocol that has been standard care in the intensive care setting. Research indicates that patients may benefit from starting this protocol when they present to the ED rather than waiting until they get to the intensive care unit (ICU).9,10 While not all patients with sepsis enter the hospital through the ED, timely initiation of care can have a positive impact on outcomes.
Definitions11
Through the years attempts have been made to define sepsis and sepsis-related terms to help understand the syndrome and accurately diagnose patients. However, efforts have not always been met with universal support.12 In 1991 the American College of Chest Physicians (ACCP) and the Society of Critical Care Medicine (SCCM) met with the goal of agreeing on sepsis definitions.13 In 2001 ACCP, SCCM, the European Society of Intensive Care Medicine (ESICM), the American Thoracic Society (ATS), and the Surgical Infection Society (SIS) revisited the 1991 definitions and found that they still had merit and should remain as described 10 years prior. The following list contains definitions of common terms used in the diagnosis and classification of sepsis13:
• Infection: Microbial phenomenon characterized by an inflammatory response to the presence of microorganisms or the invasion of normally sterile host tissue by those organisms.
• Bacteremia: Presence of viable bacteria in the blood.
• Systemic inflammatory response syndrome (SIRS): Systemic inflammatory response to a variety of severe clinical insults, manifested by two or more of the following conditions:
• Sepsis: Presence of infection or suspicion of infection, with two or more of the SIRS criteria.
• Severe sepsis: Sepsis associated with organ dysfunction, hypoperfusion, or hypotension. Hypoperfusion and perfusion abnormalities may include, but are not limited to, lactic acidosis, oliguria, or an acute alteration in mental status.
• Septic shock: Sepsis-induced shock with hypotension despite adequate crystalloid resuscitation, along with the presence of perfusion abnormalities that may include, but are not limited to, lactic acidosis, oliguria, or an acute alteration in mental status. Patients receiving inotropic or vasopressor agents may not be hypotensive at the time that perfusion abnormalities are measured.
• Sepsis-induced hypotension: A systolic blood pressure less than 90 mm Hg, mean arterial pressure (MAP) less than 65 mm Hg, or a reduction of 40 mm Hg from baseline in the absence of other causes for hypotension.
• Multiple organ dysfunction syndrome: Altered organ function in an acutely ill patient such that homeostasis cannot be maintained without intervention
Figure 21-1 shows the interrelationships among SIRS, sepsis, and infection.
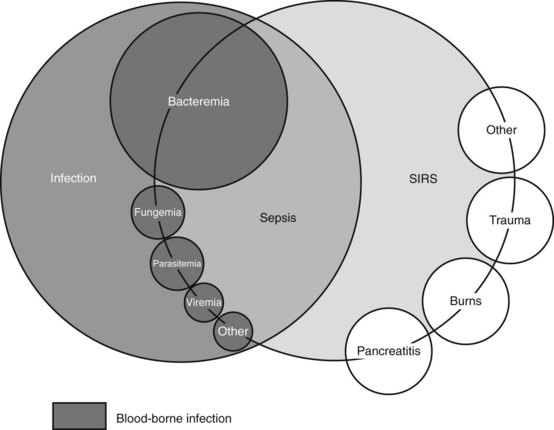
Fig. 21-1 Interrelationships among systemic inflammatory response syndrome (SIRS), sepsis, and infection.
(From American College of Chest Physicians & Society of Critical Care Medicine Consensus Conference Committee. [1992]. American College of Chest Physicians/Society of Critical Care Medicine Consensus Conference: Definitions for sepsis and organ failure and guidelines for the use of innovative therapies in sepsis. Critical Care Medicine, 20[6], 864–874.)
Identifying SIRS or Sepsis
The pathophysiology of sepsis is a complex set of events that involves innate immune response, inflammatory cascades, procoagulant and antifibrinolytic pathways, alterations in cellular metabolism and signaling, and acquired immune dysfunction.14
SIRS is a dynamic state that starts when a major insult to the body (Fig. 21-1) progresses to an overwhelming systemic inflammation. When infection is the cause of that insult, the systemic inflammatory response can quickly transition into severe sepsis or septic shock. Prompt identification of the patient with potential sepsis is crucial in the ED setting. While nearly 30% of all patients diagnosed with sepsis enter the hospital through the ED, it is also known that these patients may not fit neatly into the definitions described in the literature.11
General assessment of the patient during triage, coupled with a thorough history and physical assessment is crucial in identifying sepsis. Patients with sepsis may present with fever, chills, shortness of breath or tachypnea, tachycardia, rash, or confusion. These symptoms can mimic other disease processes making it difficult to diagnose sepsis in the early stages.15 In the triage process it is important to consider the age and history of the patient. The elderly, children, and infants have a higher incidence of sepsis than young adults.5 It is also essential to determine whether the patient is immune-compromised or if he or she has had any recent surgery, urinary tract infections, respiratory infections, skin infections, or invasive medical procedures. Medical history, such as diabetes, should also be factored into triage decisions.
• Fever higher than 38° C (100.8° F)
• Hypothermia: temperature less than 36° C (96.8° F)
• Tachycardia: heart rate greater than 90 beats per minute
• Tachypnea: respirations greater than 20 breaths per minute
• Acutely altered mental status
• Systolic blood pressure (SBP) less than 90 mm Hg or MAP less than 65 mm Hg
• SBP decrease greater than 40 mm Hg from baseline
• Creatinine greater than 2.0 mg/dL or urine output less than 0.5 mL/kg per hour for more than 2 hours
• Bilirubin greater than 2 mg/dL
• Platelet count less than 100,000/mm3
The Surviving Sepsis Campaign and the Institute for Healthcare Improvement recommend that facilities consider evaluating high-risk patients for sepsis or severe sepsis.16,17 These groups have developed a tool that can be implemented in the ED setting and provides an algorithm for decision making using SIRS criteria. This screening tool is shown in Figure 21-2.
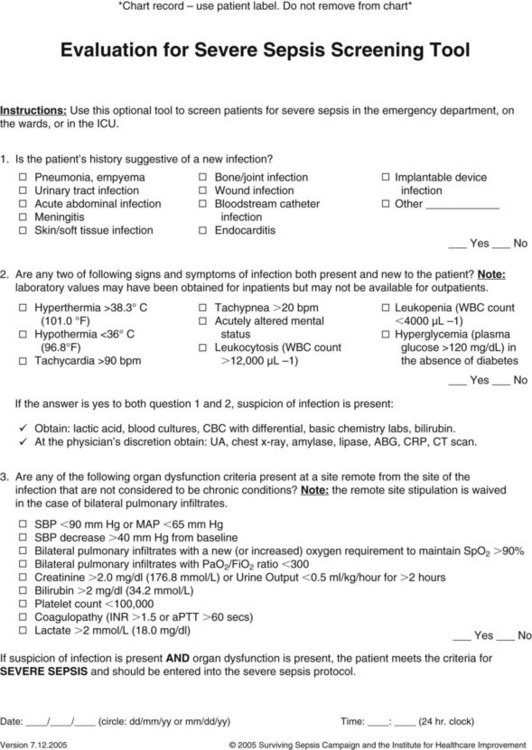
Fig. 21-2 Sample screening tool for severe sepsis.
(From Surviving Sepsis Campaign. [2005]. Individual chart measurement tool. Retrieved from http://ssc.sccm.org/files/Tools/individualchartmeasurementtool.pdf. Reproduced with permission. Copyright 2005. European Society of Intensive Care Medicine, International Sepsis Forum, and Society of Critical Care Medicine.)
According to the Surviving Sepsis Campaign, patients with SIRS and an identified source of infection are considered to have sepsis.16 If a patient presents with two or more of the SIRS criteria and new-onset organ dysfunction, the patient meets criteria for severe sepsis. Patients in septic shock present with severe sepsis along with hypoperfusion, which is recognized by a MAP of less than 65 mm Hg or a measured lactate level of greater than 4 mmoL/L.2 In septic shock, hypoperfusion will continue despite fluid resuscitation. The patient’s SBP will remain less than 90 mm Hg or the patient’s SBP will drop more than 40 mm Hg.18
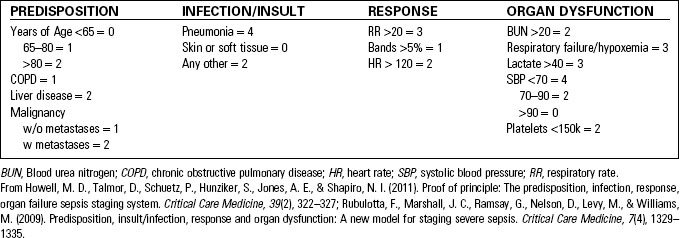
The PIRO model of sepsis identification uses predisposition, infection or insult, response, and organ dysfunction to stage sepsis and predict mortality (Table 21-1).19 A PIRO score can be calculated within each category:
• Predisposition includes such risk factors as age, history of malignancy, liver disease, or chronic obstructive pulmonary disease as well as residency in a nursing home.
• Infection or insult is measured based on the presence of pneumonia, skin infection, or other infection risk.
• Response is measured in terms of respiratory rate, heart rate, or presence of bands (immature cells) in the white blood cell count.
• Organ dysfunction is scored based on blood urea nitrogen, presence of hypoxemia, lactate levels, platelet count, and SBP.20
Another method of identifying potential sepsis patients is the Mortality in Emergency Department Sepsis (MEDS) score (Table 21-2). It takes into account some of the variables of PIRO. This score combines such variables as the patient’s age, mental status, tachypnea or hypoxemia, and platelet count along with risk factors such as being a nursing home resident or having a lower respiratory infection or terminal illness. There is evidence that this is a reliable means of risk stratification in SIRS or sepsis patients in the ED.21,22
TABLE 21-2 MEDS SCORING AND PREDICTED MORTALITY
| Meds Scoring | |
|---|---|
| CHARACTERISTIC | POINTS ASSIGNED |
| Predisposition | |
| Age >65 years | 3 |
| Nursing home resident | 2 |
| Rapidly terminal comorbid illness | 6 |
| Infection | |
| Lower respiratory infection | 2 |
| Response | |
| Bands >5% | 3 |
| Organ dysfunction | |
| Tachypnea or hypoxemia | 3 |
| Septic shock | 3 |
| Platelet count <150,000/mm3 | 3 |
| Altered mental status | 2 |
| Meds Predicted Mortality | ||
|---|---|---|
| POINT RANGE | MEDS GROUP | 28-DAY PREDICTED MORTALITY |
| 0–4 | Very low | 1.1% |
| 5–7 | Low | 4.4% |
| 8–12 | Moderate | 9.3% |
| 13–15 | High | 16.1% |
| >15 | Very high | 39.0% |
From Shapiro, N. I., Howell, M. D., Talmor, D., Donnino, M., Ngo, L., & Bates, D. W. (2007). Mortality in Emergency Department Sepsis (MEDS) score predicts 1-year mortality. Critical Care Medicine, 35(1), 192–198.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree