INTRODUCTION AND EPIDEMIOLOGY
Unusual movements and changes in behavior in children often lead to an ED visit. Most seizure activity stops before the child is seen in an ED; therefore, history is key to the correct diagnosis. Although seizures account for many of these events, as many as 30% or more of paroxysmal events may be misdiagnosed as seizures.1
There are many different causes of pediatric seizures. The goal is to identify and treat the underlying cause. Some seizures require emergency management and extensive evaluation (e.g., status epilepticus, neonatal seizures), whereas others are common, benign, and need little or no ED evaluation (e.g., febrile seizures, first-time seizure in an otherwise well child). This chapter focuses on the diagnosis and management of ongoing seizures first, and the approach to febrile seizures, neonatal seizures, and seizures in special populations (e.g., children with epilepsy, neurologic shunts, and trauma) are discussed under Special Considerations/Populations.
The incidence of new-onset pediatric seizure in the United States is approximately 120,000 cases per year and is highest in children <2 years and in certain high-risk groups.2 Febrile seizures are the most common type of pediatric seizure, affecting 2% to 5% of all children between 6 months and 5 years of age.3 Epilepsy is diagnosed when a patient has one or more unprovoked seizures.4,5 Roughly 326,000 children <15 years have epilepsy, and 1% of the population can be expected to have epilepsy by the age of 20.2 The incidence of status epilepticus in developed countries is between 17 and 23 cases per 100,000 and is higher for younger children.6
PATHOPHYSIOLOGY
Seizures represent abnormal, excessive, paroxysmal neuronal activity in the brain, primarily the cortex. Glutamate released from firing neurons activates N-methyl-d-aspartic acid receptors that subsequently initiate and propagate seizure activity.7 Seizures are inhibited by gamma-aminobutyric-acid, and failure of this inhibition facilitates seizure spread.7 Incomplete myelination of the brain may limit secondary generalization of seizure activity in young infants, and a relative imbalance between glutamate and gamma-aminobutyric-acid with paradoxical excitation from gamma-aminobutyric-acid makes younger children more susceptible to seizure activity.
Seizures can be primary (intrinsic) or secondary (the result of another process). Primary seizures are often idiopathic or may be caused by congenital developmental abnormalities, in utero central nervous system insult (e.g., infection, infarct), or genetic factors. Secondary seizures may result from trauma or injury, infection, metabolic abnormalities (e.g., hypoglycemia, electrolyte abnormalities, inborn errors of metabolism), toxins, or systemic illness.
CLINICAL FEATURES
The clinical manifestation of seizures depends on the area(s) of the brain that are affected and whether the seizure activity is localized (focal) or widespread (generalized). Generalized seizures involve both hemispheres of the brain and lead to loss of consciousness, usually followed by a period of postictal drowsiness. In convulsive generalized seizures or grand mal seizures, rhythmic motor activity affects both sides of the body. Nonconvulsive generalized seizures produce loss of consciousness without motor activity and can only be recognized on electroencephalogram. In one study, nonconvulsive status epilepticus appeared in 51 of 117 critically ill patients, with 75% of these patients showing no clinical evidence of seizure activity.8 Other examples of generalized seizures in children include absence seizures (brief episode of staring without a postictal state), atonic seizures (sudden loss of muscle tone with a sudden “drop” to the floor), and myoclonic seizures.
Partial seizures represent focal neuronal activity, and clinical features correlate with the affected area. In simple partial seizures, the patient remains awake, whereas complex partial seizures are focal but produce alterations of consciousness. Partial seizures may secondarily spread and become generalized. Young children with new-onset focal seizures are at increased risk for structural anatomic abnormalities, and neuroimaging is more likely to be abnormal in these children.9
Although status epilepticus was originally defined as a seizure lasting longer than 30 minutes, today any “prolonged” seizure, or recurrent seizures lasting >5 minutes without return to full consciousness, is considered status epilepticus.10,11 Status epilepticus is a medical emergency, and rapid termination is important to prevent irreversible neuronal damage.7,12 Refractory status epilepticus is a prolonged seizure that cannot be controlled with two or more doses of standard treatment.7,12 Nonconvulsive status epilepticus may present as a prolonged postictal state8 and must be considered in any patient with altered mental status; morbidity and mortality increase when nonconvulsive status epilepticus is untreated, though less so than with untreated convulsive status epilepticus.8,13
Obtain a detailed history of the event from a reliable observer. Table 135-1 lists historical clues that may help identify a cause for seizures. Important details include the events surrounding the seizure (e.g., emotional upset and crying that may indicate breath holding in a toddler), the nature of the seizure activity (e.g., tonic stiffening, clonic jerks, generalized or focal characteristics), the duration of the event (often difficult for frightened parents to accurately report), and postictal observations and duration. Ask about recent illness, possible trauma, ingestions, and medications (both over-the-counter and prescribed). Inquire about past medical history (especially epilepsy) and recent changes or missed doses of medication. A developmental history is important, as children with underlying developmental delay are at increased risk for epilepsy. A family history of febrile seizures, epilepsy, or neurologic disease is also important for prognosis. Patient age alone is an important consideration in the potential cause of seizures, as depicted in Figure 135-1.
Age of child Seizure duration and description of seizure activity prior to arrival History of trauma History of possible ingestion History of fever History of associated illness (vomiting or diarrhea) Feeding problems (especially in an infant) Changes in behavior History of seizures and type of seizures History of developmental delay Other medical history Medications
Developmental history Family history of seizures |
Perform a complete head-to-toe examination with the patient undressed. The physical examination should be focused on whether the patient is actively seizing and identify potential causative factors (e.g., head trauma, rash indicative of infection, neurocutaneous lesions). Table 135-2 outlines a number of clinical signs and symptoms of seizures. Rhythmic repetitive movement, incontinence of bowel or bladder, postictal state after a seizure, and tongue biting are strong clues to a seizure. Lateral tongue biting was found to have a specificity of 100% and a sensitivity of 24% for the occurrence of a seizure.14
Head deviation Eye deviation Rhythmic or repetitive arm or leg movement
Change in breathing pattern Increase in heart rate Increase in blood pressure Cyanosis or apnea Eye dilatation Vomiting Lip smacking Tongue biting Incontinence of bowel or bladder Postictal or sleepy period after a seizure Mood or behavior changes before a seizure Subjective aura before seizure (noted in older patients) |
DIAGNOSIS
A number of benign conditions may masquerade as seizures, leading to an ED visit; up to 30% of new-onset paroxysmal events may be misdiagnosed as epileptic.1 Syncope is the most common condition that may be mistaken for seizures; however, there are many differentiating features. Syncope is commonly preceded by dizziness, weakness, tunnel vision, pallor, and diaphoresis (presyncopal aura). It is also associated with a brief loss of consciousness and a quick recovery with no postictal state. Seizures, on the other hand, may be preceded by an aura but usually do not have a provoking factor noted before the event. Seizures are associated with tongue biting, rhythmic motor activity, incontinence, and a slow recovery and postictal state. Table 135-3 lists nonepileptic causes of syncope and abnormal movements that can mimic seizures. In infants, myoclonic jerks, sleep myoclonus, shudder attacks, and Sandifer’s- syndrome (gastroesophageal reflux) are common. In toddlers, breath-holding spells become more prevalent. Self-stimulation and night terrors should be considered in preschool and young school-age children, whereas tic disorders typically begin in older children.
Syncope
Sandifer’s syndrome (gastroesophageal reflux) Acute life-threatening event Acute dystonic reactions/drug reactions (i.e., promethazine [Phenergan®]) Movement disorders
Night terrors, sleep walking Migraine variants Benign paroxysmal vertigo Nonepileptic paroxysmal event (pseudoseizures) |
Check bedside glucose on all seizing or postictal patients. Additional laboratory evaluation is directed by the history and is not routinely indicated for febrile seizures or first-time afebrile seizures that are nonfocal in a child with a normal examination (see Special Considerations/Populations, later). If indicated by the history and examination, labs that may be helpful include electrolytes (including calcium), serum antiepileptic medication levels, toxicologic testing, and spinal fluid for evaluation of possible central nervous system infection in the appropriate setting. Urine culture and analysis is indicated in the evaluation of febrile seizures in the child with fever and no identifiable source.
Similar to laboratory testing, imaging should be directed by the history and examination. Routine neuroimaging is rarely indicated or helpful. When trauma is suspected or in the setting of focal deficits, obtain a head CT. Todd’s paralysis is a temporary condition characterized by a focal deficit of unknown etiology that can last up to 36 hours after a seizure.15 The paralysis is usually unilateral and lasts on average 15 hours15; however, it can be bilateral and involve a patient’s speech or vision.13 It may be impossible to distinguish Todd’s paralysis from stroke or hemorrhage, and emergent imaging should be considered.15 Most first-time seizures in the well-appearing child with a normal examination are best evaluated with outpatient MRI, which avoids ionizing radiation and provides better anatomic detail.
Consider obtaining an electrocardiogram for evaluation of syncope with seizure activity to rule out arrhythmia. Emergent electroencephalogram monitoring may be required for patients with refractory status epilepticus (especially those requiring rapid sequence intubation with a paralytic) or concern for nonconvulsive status epilepticus; otherwise, outpatient electroencephalogram may help identify specific epilepsy syndromes and guide future treatment.
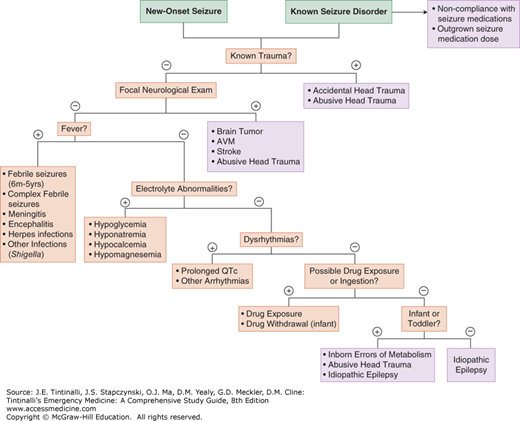
Figure 135-2 summarizes the approach to the evaluation of pediatric seizures.
TREATMENT
Children may have been treated at home or by EMS personnel. Take this into consideration when treating refractory status epilepticus.
Benzodiazepines (Table 135-4) are the first-line treatment for prolonged seizures because of their rapid onset and effectiveness; however, not all benzodiazepines or routes are available in the prehospital setting, and establishing IV access can be difficult in a child who is having a seizure.7,10,15 Benzodiazepines may be given by the intranasal, buccal, rectal, or intraosseous route when an IV is difficult to place.11,16–25
| Drug | Route | Dose* | Maximum | Onset of Action | Duration of Action |
|---|---|---|---|---|---|
| Lorazepam | IV, IO, IN IM | 0.1 milligram/kg 0.1 milligram/kg | 4 milligrams 4 milligrams | 1–5 min 15–30 min | 12–24 h 12–24 h |
| Diazepam | IV, IO PR | 0.1–0.3 milligram/kg 0.5 milligram/kg | 10 milligrams 20 milligrams | 1–5 min 3–5 min | 15–60 min 15–60 min |
| Midazolam | IV, IO IM IN Buccal | 0.1–0.2 milligram/kg 0.2 milligram/kg 0.2 milligram/kg 0.5 milligram/kg | 4 milligrams 10 milligrams 10 milligrams 10 milligrams | 1–5 min 5–15 min 1–5 min 3–5 min | 1–6 h 1–6 h 1–6 h 1–6 h |
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree