Study objective
The study objective was to determine whether intravenous contrast administration for computed tomography (CT) is independently associated with increased risk for acute kidney injury and adverse clinical outcomes.
Methods
This single-center retrospective cohort analysis was performed in a large, urban, academic emergency department with an average census of 62,179 visits per year; 17,934 ED visits for patients who underwent contrast-enhanced, unenhanced, or no CT during a 5-year period (2009 to 2014) were included. The intervention was CT scan with or without intravenous contrast administration. The primary outcome was incidence of acute kidney injury. Secondary outcomes included new chronic kidney disease, dialysis, and renal transplantation at 6 months. Logistic regression modeling and between-groups odds ratios with and without propensity-score matching were used to test for an independent association between contrast administration and primary and secondary outcomes. Treatment decisions, including administration of contrast and intravenous fluids, were examined.
Results
Rates of acute kidney injury were similar among all groups. Contrast administration was not associated with increased incidence of acute kidney injury (contrast-induced nephropathy criteria odds ratio=0.96, 95% confidence interval 0.85 to 1.08; and Acute Kidney Injury Network/Kidney Disease Improving Global Outcomes criteria odds ratio=1.00, 95% confidence interval 0.87 to 1.16). This was true in all subgroup analyses regardless of baseline renal function and whether comparisons were made directly or after propensity matching. Contrast administration was not associated with increased incidence of chronic kidney disease, dialysis, or renal transplant at 6 months. Clinicians were less likely to prescribe contrast to patients with decreased renal function and more likely to prescribe intravenous fluids if contrast was administered.
Conclusion
In the largest well-controlled study of acute kidney injury following contrast administration in the ED to date, intravenous contrast was not associated with an increased frequency of acute kidney injury.
Introduction
Background
Intravenous iodinated contrast media are routinely used to improve the diagnostic accuracy of computed tomography (CT). Although more than 80 million doses of intravenous contrast media are administered annually, clinical decisionmaking in regard to their use is complicated by concerns related to their potential for precipitating renal dysfunction. Indeed, contrast media administration is cited as the third most common cause of iatrogenic acute kidney injury and has been linked to increased risk of major adverse events, including initiation of dialysis, renal failure, stroke, myocardial infarction, and death. Recent studies performed in the emergency department (ED), where intravenous administration of contrast media for enhancement of CT imaging is often necessary to diagnose acute critical conditions, have reported an incidence of contrast-induced nephropathy as high as 14% and linked contrast-induced nephropathy to a 2-fold increased risk of major adverse events within 1 year. Although these reports are concerning, the causal relationship between administration of intravenous contrast media and the development of acute kidney injury has recently been challenged.
What is already known on this topic
Many providers defer intravenous contrast enhancement with computed tomography (CT) because of concerns about acute kidney injury.
What question this study addressed
How often does acute kidney injury occur after enhanced and nonenhanced emergency department (ED) CT?
What this study adds to our knowledge
Using a propensity-matched case-control design at one site, the frequency of later acute kidney injury in 7,201 patients undergoing contrast-enhanced CT, 5,499 undergoing unenhanced CT, and 5,234 with no imaging did not differ (10.2% to 10.9%).
How this is relevant to clinical practice
This study suggests fear of triggering acute kidney injury after intravenous contrast during ED CT is disproportionate to objective data. A randomized trial is needed to confirm this finding.
Importance
Current understanding of contrast-induced nephropathy is complicated by studies that predate widespread use of low- and iso-osmolar contrast media and extrapolation of findings from arterial angiographic studies to the use of intravenous contrast media. Additionally, the majority of studies examining acute kidney injury after contrast media administration, including those performed in ED patients, were performed without control populations that did not receive contrast media. Indeed, serum creatinine level fluctuations meeting criteria for contrast-induced nephropathy occur in patients undergoing unenhanced CT at rates similar to those published after contrast-enhanced CT, and systematic reviews and meta-analyses of the few existing studies analyzing intravenous contrast media administration with adequate controls found no increased risk of acute kidney injury associated with contrast media.
Historically, randomized controlled trials designed to elucidate the true incidence of contrast-induced nephropathy have been perceived as unethical because of the presumption that contrast media administration is a direct cause of acute kidney injury. To date, all controlled studies of contrast-induced nephropathy have been observational, and conclusions from these studies are severely limited by selection bias associated with the clinical decision to administer contrast media. Two research groups have recently used propensity-score analysis to control for this bias, approximating randomization by matching nonrandomized populations from large single-center databases according to their probability of treatment assignment. These investigators, however, reached opposite conclusions. McDonald et al found no increased risk of acute kidney injury, emergency dialysis, or mortality after contrast media administration in any patient group regardless of baseline renal function, whereas Davenport et al reported an increased risk of acute kidney injury after contrast media administration in patients with preexisting renal dysfunction. Potential explanations for these discrepant results include different strategies for propensity matching, variances in institutional contrast-enhanced CT protocols, and widely discordant subgroup sample sizes, especially at the lowest baseline renal function.
Goals of This Investigation
In this study, we sought to clarify the incidence of acute kidney injury attributable to intravenous contrast media administration by testing the hypothesis that such injury occurs at higher rates in patients undergoing contrast-enhanced CT than in those not receiving contrast media. To minimize biases associated with comparison of nonrandomized populations, we used 2 distinct control populations that did not receive contrast media, used propensity-score analysis to minimize bias associated with treatment assignment, and analyzed large numbers of patients in all subgroups of baseline renal function. We also examined selected clinician practice patterns that may affect the incidence of acute kidney injury after contrast media administration.
Materials and Methods
Study Design and Setting
This was a single-center retrospective cohort study conducted in a large urban academic ED. During the study period, our mean annual ED census was 62,179 total visits (range 55,955 to 69,249), with a mean annual admission rate of 23.4% (range 22.2% to 25.1%). This study was approved by our university institutional review board.
An experienced data user (E.Y.K.) extracted all clinical information from a relational database that underlies the electronic medical record of our ED. Queries using structured query language were performed separately for patients who did and did not undergo CT. For patients who underwent CT, data were extracted for all encounters that had both an order and result interpretation for at least one CT scan during the study period. Two authors (J.S.H. and M.R.E.) not involved in data extraction classified CT studies as enhanced or unenhanced based on specific and standardized order and result interpretation identifiers. When order and result interpretation identifiers differed (which occurred in cases in which the radiology team, in consultation with the ordering ED clinician, performed a study that differed from the original order), result interpretation identifiers were used. Any discrepancies were resolved through consensus. For patients who did not undergo CT, data were extracted for all encounters that lacked an order or result for a CT study. All data relating to vital signs, medication administration, and preexisting diagnoses entered in the ED, as well as laboratory results and new procedure or diagnostic codes entered from any point in our hospital system, were extracted with the same structured query language for every patient. Medical diagnoses and procedures were identified with International Classification of Diseases, Ninth Edition, Clinical Modification ( ICD-9-CM ) diagnostic and procedure codes.
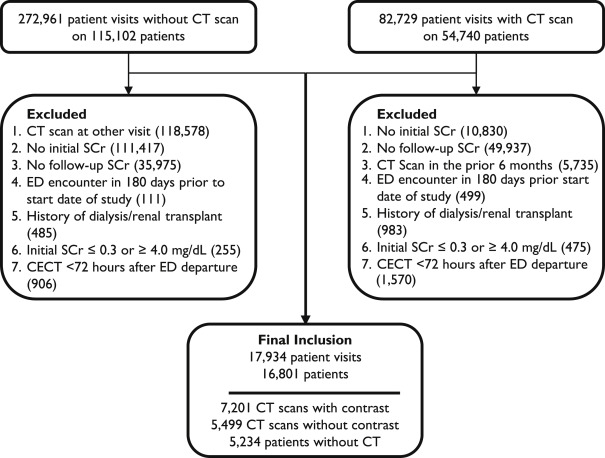
Selection of Participants
Patients aged 18 years and older who received a CT with or without contrast enhancement in the ED between January 1, 2009, and June 30, 2014, and had both an initial serum creatinine level measured in the 8 hours before CT and a second level measured 48 to 72 hours after CT were included. To minimize bias associated with the decision to obtain imaging, we included a second control group of contrast media-unexposed ED patients aged 18 years and older and treated during the study period who did not undergo CT imaging, and had both an initial serum creatinine level measured in the ED and a second level measured 48 to 72 hours later. Exclusion criteria included initial serum creatinine level less than 0.4 mg/dL (to minimize inclusion of random laboratory error as cases of acute kidney injury) or equal to or greater than 4.0 mg/dL (already meeting partial criteria for severe acute kidney injury), insufficient serum creatinine level data, a history of renal transplant or ongoing or previous dialysis, an ED visit in the 6 months before the study start date, a CT scan performed in the 6 months preceding the index ED visit, and contrast-enhanced CT performed within 72 hours of ED departure. We chose the antecedent 6-month window to minimize potential confounding residual effects of previously administered contrast media and the subsequent 72-hour window to minimize potential group crossover of patients undergoing CT scan after ED departure within the period defined by contrast-induced nephropathy criteria. CT scans were classified as contrast enhanced or unenhanced. Consecutive CT acquisitions at different anatomic locations were treated as a single-scan event, and those performed with and without contrast media were treated as a single contrast-enhanced CT. All eligible patients during a 5-year period were included, resulting in a sample size powered to detect a difference in incidence of acute kidney injury between populations as low as 1.5%.
The primary variable of interest was administration of intravenous contrast media. Control variables included age, sex, race, initial serum creatinine level, initial estimated glomerular filtration rate, and chronic comorbidities and acute illness severity indicators previously shown to predispose to the development of contrast-associated acute kidney injury. Chronic comorbidities included diabetes mellitus, hypertension, HIV/AIDS, congestive heart failure, chronic kidney disease, and history of renal transplantation (all identified by ICD-9-CM codes ). Acute illness severity indicators included hypotension (systolic blood pressure <80 mm Hg), designation by an ED attending physician as a patient requiring critical care, anemia (hematocrit level <39% or <36% for men and women, respectively), and hypoalbuminemia (<3.5 g/dL) during the index ED visit. Additional control variables included ED administration of nephrotoxic or nephroprotective medications (see Figure E1 , available online at http://www.annemergmed.com , for full list) and ED administration of intravenous crystalloid fluids in any amount.
All contrast media administration was performed according to institutional protocols, available online at http://www.ctisus.com/protocols . Patients who underwent contrast-enhanced CT were administered either iohexol or iodixanol intravenously, as dictated by radiologic study-specific protocol, and volumes of administration ranged from 80 to 120 mL. According to institutional policy, patients provided consent before administration of intravenous contrast, and for patients with serum creatinine level greater than 1.7 mg/dL, treating clinicians cosigned consent for contrast-enhanced CT.
Outcome Measures
The primary outcome variable was incidence of acute kidney injury. The clinical definition of acute kidney injury has undergone multiple revisions, with published studies of contrast-induced nephropathy using varied equations to calculate its incidence. We estimated the incidence of acute kidney injury for all study participants by using both the most frequently published criteria for contrast-induced nephropathy (absolute increase in serum creatinine level ≥0.5 mg/dL or ≥25% increase over baseline serum creatinine level at 48 to 72 hours after imaging or, for non-CT patients, after initial serum creatinine level measurement) and for acute kidney injury as defined by the Acute Kidney Injury Network/Kidney Disease Improving Global Outcomes guidelines. By Acute Kidney Injury Network/Kidney Disease Improving Global Outcomes creatinine-based criteria, acute kidney injury is staged (stage 1: absolute increase in serum creatinine level ≥0.3 mg/dL or a 1.5- to 1.9-fold increase over baseline serum creatinine level; stage 2: 2.0- to 2.9-fold increase over baseline serum creatinine level; stage 3: 3-fold increase over baseline serum creatinine level, increase to serum creatinine level ≥4.0 mg/dL, or initiation of dialysis). We classified any patient meeting Acute Kidney Injury Network/Kidney Disease Improving Global Outcomes stage 1 criteria as having acute kidney injury and performed subanalyses to compare patients meeting criteria for stages 2 and 3. Patient-centered outcomes were assessed, including newly diagnosed chronic kidney disease, initiation of dialysis, and renal transplantation (each assessed by ICD-9-CM or procedure code documentation in our institutional electronic medical record) within 6 months of the index ED visit.
Primary Data Analysis
Dichotomous variables are displayed as percentages, categorical data as relative frequencies (in percentages), and continuous data as medians with interquartile ranges. A multivariable logistic regression model was used to ascertain how contrast media administration was associated with the risk of acute kidney injury in the entire study population after controlling for demographic variables and medical conditions previously reported to increase risk for developing such injury. Incidence of acute kidney injury was calculated as the percentage of visits with occurrence of acute kidney injury.
The association between contrast media and acute kidney injury was first assessed with the test of proportions to compare incidence of acute kidney injury in patients who underwent contrast-enhanced CT with those who underwent unenhanced CT and with all patients who did not receive contrast media. To reduce potential selection bias inherent to administration of contrast media, we also used propensity-score matching to estimate the effect of contrast media on acute kidney injury. The clinical decision to administer contrast media is guided by patient pathology and conditional patient-related factors that might contraindicate contrast media administration. The conditional patient factors included in the estimation of the propensity scores were sex, age, race, initial serum creatinine level or estimated glomerular filtration rate, crystalloid fluid administration, nephrotoxic medication administration, chronic comorbidities (as noted above), and whether the patient was designated as requiring critical care. Propensity-score matching was performed with default parameters (nearest neighbor of one, no caliper restriction, and sampling with replacement), and the average treatment effect was calculated. All comparisons were made for the entire study population and for subgroups stratified by initial serum creatinine level and estimated glomerular filtration rate. Matching for propensity score was performed by group for subgroup analyses. Results are presented as odds ratios (ORs). All analysis, including propensity-score matching, was conducted in Stata (version 14.1; StataCorp, College Station, TX).
Materials and Methods
Study Design and Setting
This was a single-center retrospective cohort study conducted in a large urban academic ED. During the study period, our mean annual ED census was 62,179 total visits (range 55,955 to 69,249), with a mean annual admission rate of 23.4% (range 22.2% to 25.1%). This study was approved by our university institutional review board.
An experienced data user (E.Y.K.) extracted all clinical information from a relational database that underlies the electronic medical record of our ED. Queries using structured query language were performed separately for patients who did and did not undergo CT. For patients who underwent CT, data were extracted for all encounters that had both an order and result interpretation for at least one CT scan during the study period. Two authors (J.S.H. and M.R.E.) not involved in data extraction classified CT studies as enhanced or unenhanced based on specific and standardized order and result interpretation identifiers. When order and result interpretation identifiers differed (which occurred in cases in which the radiology team, in consultation with the ordering ED clinician, performed a study that differed from the original order), result interpretation identifiers were used. Any discrepancies were resolved through consensus. For patients who did not undergo CT, data were extracted for all encounters that lacked an order or result for a CT study. All data relating to vital signs, medication administration, and preexisting diagnoses entered in the ED, as well as laboratory results and new procedure or diagnostic codes entered from any point in our hospital system, were extracted with the same structured query language for every patient. Medical diagnoses and procedures were identified with International Classification of Diseases, Ninth Edition, Clinical Modification ( ICD-9-CM ) diagnostic and procedure codes.
Selection of Participants
Patients aged 18 years and older who received a CT with or without contrast enhancement in the ED between January 1, 2009, and June 30, 2014, and had both an initial serum creatinine level measured in the 8 hours before CT and a second level measured 48 to 72 hours after CT were included. To minimize bias associated with the decision to obtain imaging, we included a second control group of contrast media-unexposed ED patients aged 18 years and older and treated during the study period who did not undergo CT imaging, and had both an initial serum creatinine level measured in the ED and a second level measured 48 to 72 hours later. Exclusion criteria included initial serum creatinine level less than 0.4 mg/dL (to minimize inclusion of random laboratory error as cases of acute kidney injury) or equal to or greater than 4.0 mg/dL (already meeting partial criteria for severe acute kidney injury), insufficient serum creatinine level data, a history of renal transplant or ongoing or previous dialysis, an ED visit in the 6 months before the study start date, a CT scan performed in the 6 months preceding the index ED visit, and contrast-enhanced CT performed within 72 hours of ED departure. We chose the antecedent 6-month window to minimize potential confounding residual effects of previously administered contrast media and the subsequent 72-hour window to minimize potential group crossover of patients undergoing CT scan after ED departure within the period defined by contrast-induced nephropathy criteria. CT scans were classified as contrast enhanced or unenhanced. Consecutive CT acquisitions at different anatomic locations were treated as a single-scan event, and those performed with and without contrast media were treated as a single contrast-enhanced CT. All eligible patients during a 5-year period were included, resulting in a sample size powered to detect a difference in incidence of acute kidney injury between populations as low as 1.5%.
The primary variable of interest was administration of intravenous contrast media. Control variables included age, sex, race, initial serum creatinine level, initial estimated glomerular filtration rate, and chronic comorbidities and acute illness severity indicators previously shown to predispose to the development of contrast-associated acute kidney injury. Chronic comorbidities included diabetes mellitus, hypertension, HIV/AIDS, congestive heart failure, chronic kidney disease, and history of renal transplantation (all identified by ICD-9-CM codes ). Acute illness severity indicators included hypotension (systolic blood pressure <80 mm Hg), designation by an ED attending physician as a patient requiring critical care, anemia (hematocrit level <39% or <36% for men and women, respectively), and hypoalbuminemia (<3.5 g/dL) during the index ED visit. Additional control variables included ED administration of nephrotoxic or nephroprotective medications (see Figure E1 , available online at http://www.annemergmed.com , for full list) and ED administration of intravenous crystalloid fluids in any amount.
All contrast media administration was performed according to institutional protocols, available online at http://www.ctisus.com/protocols . Patients who underwent contrast-enhanced CT were administered either iohexol or iodixanol intravenously, as dictated by radiologic study-specific protocol, and volumes of administration ranged from 80 to 120 mL. According to institutional policy, patients provided consent before administration of intravenous contrast, and for patients with serum creatinine level greater than 1.7 mg/dL, treating clinicians cosigned consent for contrast-enhanced CT.
Outcome Measures
The primary outcome variable was incidence of acute kidney injury. The clinical definition of acute kidney injury has undergone multiple revisions, with published studies of contrast-induced nephropathy using varied equations to calculate its incidence. We estimated the incidence of acute kidney injury for all study participants by using both the most frequently published criteria for contrast-induced nephropathy (absolute increase in serum creatinine level ≥0.5 mg/dL or ≥25% increase over baseline serum creatinine level at 48 to 72 hours after imaging or, for non-CT patients, after initial serum creatinine level measurement) and for acute kidney injury as defined by the Acute Kidney Injury Network/Kidney Disease Improving Global Outcomes guidelines. By Acute Kidney Injury Network/Kidney Disease Improving Global Outcomes creatinine-based criteria, acute kidney injury is staged (stage 1: absolute increase in serum creatinine level ≥0.3 mg/dL or a 1.5- to 1.9-fold increase over baseline serum creatinine level; stage 2: 2.0- to 2.9-fold increase over baseline serum creatinine level; stage 3: 3-fold increase over baseline serum creatinine level, increase to serum creatinine level ≥4.0 mg/dL, or initiation of dialysis). We classified any patient meeting Acute Kidney Injury Network/Kidney Disease Improving Global Outcomes stage 1 criteria as having acute kidney injury and performed subanalyses to compare patients meeting criteria for stages 2 and 3. Patient-centered outcomes were assessed, including newly diagnosed chronic kidney disease, initiation of dialysis, and renal transplantation (each assessed by ICD-9-CM or procedure code documentation in our institutional electronic medical record) within 6 months of the index ED visit.
Primary Data Analysis
Dichotomous variables are displayed as percentages, categorical data as relative frequencies (in percentages), and continuous data as medians with interquartile ranges. A multivariable logistic regression model was used to ascertain how contrast media administration was associated with the risk of acute kidney injury in the entire study population after controlling for demographic variables and medical conditions previously reported to increase risk for developing such injury. Incidence of acute kidney injury was calculated as the percentage of visits with occurrence of acute kidney injury.
The association between contrast media and acute kidney injury was first assessed with the test of proportions to compare incidence of acute kidney injury in patients who underwent contrast-enhanced CT with those who underwent unenhanced CT and with all patients who did not receive contrast media. To reduce potential selection bias inherent to administration of contrast media, we also used propensity-score matching to estimate the effect of contrast media on acute kidney injury. The clinical decision to administer contrast media is guided by patient pathology and conditional patient-related factors that might contraindicate contrast media administration. The conditional patient factors included in the estimation of the propensity scores were sex, age, race, initial serum creatinine level or estimated glomerular filtration rate, crystalloid fluid administration, nephrotoxic medication administration, chronic comorbidities (as noted above), and whether the patient was designated as requiring critical care. Propensity-score matching was performed with default parameters (nearest neighbor of one, no caliper restriction, and sampling with replacement), and the average treatment effect was calculated. All comparisons were made for the entire study population and for subgroups stratified by initial serum creatinine level and estimated glomerular filtration rate. Matching for propensity score was performed by group for subgroup analyses. Results are presented as odds ratios (ORs). All analysis, including propensity-score matching, was conducted in Stata (version 14.1; StataCorp, College Station, TX).
Results
During the study period, there were 82,729 patient visits in which a CT was performed among 54,740 unique patients. Of these, 12,700 patient visits by 11,567 patients met all inclusion and no exclusion criteria. Of all CT scans, 56.7% were contrast enhanced. There were 272,961 patient visits during the study period wherein patients did not undergo CT. Of these, 5,234 met all inclusion and no exclusion criteria. Thus, a total of 17,934 patient visits from 16,801 unique patients were included in the final analysis ( Figure 1 ).
All 3 patient groups analyzed (contrast-enhanced CT, unenhanced CT, and non-CT) were demographically similar, although the unenhanced CT group was slightly older ( Table 1 ). Patients in the contrast-enhanced CT group were less likely to have diabetes, congestive heart failure, or chronic kidney disease. Initial serum creatinine values were similar across groups, although the contrast-enhanced CT group had a higher estimated glomerular filtration rate.
| Characteristics | Contrast-Enhanced CT | Unenhanced CT | Non-CT |
|---|---|---|---|
| Number of patient visits (%) | 7,201 (40.2) | 5,499 (30.7) | 5,234 (29.2) |
| Age, y | 53 (40–65) | 60 (48–73) | 55 (41–68) |
| Women (%) | 3,535 (49.1) | 2,727 (49.6) | 2,637 (50.4) |
| Race (%) | |||
| Black | 3,747 (52.0) | 2,951 (53.7) | 2,367 (45.2) |
| White | 2,851 (39.6) | 2,206 (40.1) | 2,415 (46.1) |
| Other | 603 (8.4) | 342 (6.2) | 452 (8.6) |
| Initial SCr value (IQR), mg/dL | 0.9 (0.7–1.1) | 1.0 (0.8–1.6) | 1.0 (0.7–1.3) |
| eGFR (IQR), mL/min per 1.73 m 2 | 95 (74–114) | 77 (44–102) | 84 (55–108) |
| Acute illness severity indicators (%) | |||
| ED critical care designation | 763 (10.6) | 651 (11.8) | 170 (3.2) |
| Hospital admission | 6,749 (93.7) | 5,159 (93.8) | 4,882 (93.3) |
| Hypotension ∗ | 270 (3.7) | 249 (4.5) | 196 (3.7) |
| Anemia ∗ | 3,457 (48.0) | 2,819 (51.3) | 2,658 (50.8) |
| Hypoalbuminemia ∗ | 1,387 (19.3) | 1,010 (18.4) | 978 (18.7) |
| Medications administered (%) | |||
| Nephrotoxic † | 1,072 (14.9) | 596 (10.8) | 2,097 (40.1) |
| Nephroprotective ‡ | 56 (0.8) | 17 (0.3) | 78 (1.5) |
| Crystalloid fluids | 1,748 (24.3) | 783 (14.2) | 2,530 (48.3) |
| Comorbidities (%) § | |||
| Diabetes mellitus | 1,373 (19.1) | 1,461 (26.6) | 1,183 (22.6) |
| Hypertension | 3,050 (42.4) | 2,881 (52.4) | 2,073 (39.6) |
| Congestive heart failure | 918 (12.7) | 979 (17.8) | 928 (17.7) |
| HIV/AIDS | 303 (4.2) | 331 (6.0) | 130 (2.5) |
| Chronic kidney disease | 445 (6.2) | 1,112 (20.2) | 735 (14.0) |
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree







