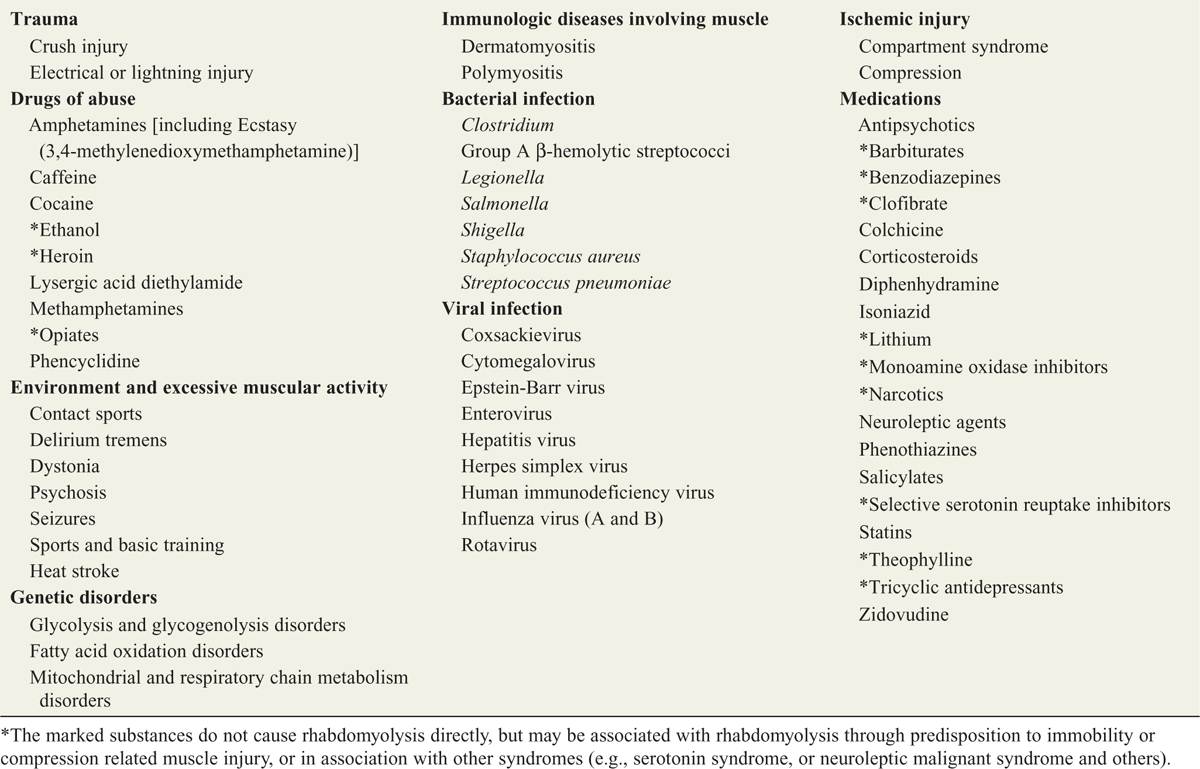
Conditions associated with rhabdomyolysis are listed in Table 53-1.
![]() Comatose patients are at risk for rhabdomyolysis due to prolonged immobilization with continual pressure on gravity-dependent parts of the body.
Comatose patients are at risk for rhabdomyolysis due to prolonged immobilization with continual pressure on gravity-dependent parts of the body.
TABLE 53-1 Common Conditions Associated with Rhabdomyolysis in Adults
PATHOPHYSIOLOGY
![]() Skeletal muscle injury results in cellular death with resultant leakage of previously intracellular contents into the vasculature.
Skeletal muscle injury results in cellular death with resultant leakage of previously intracellular contents into the vasculature.
![]() Common cellular agents that leak into the circulation include myoglobin, creatinine kinase, aldolase, lactate dehydrogenase, potassium, and aspartate aminotransferase.
Common cellular agents that leak into the circulation include myoglobin, creatinine kinase, aldolase, lactate dehydrogenase, potassium, and aspartate aminotransferase.
![]() Disruption of the sodium/potassium/ATPase and calcium transport results in increased intracellular calcium which, ultimately triggers cellular death.
Disruption of the sodium/potassium/ATPase and calcium transport results in increased intracellular calcium which, ultimately triggers cellular death.
CLINICAL FEATURES
![]() A number of clinical histories should raise the clinician’s suspicion for this syndrome, the most common of which follow.
A number of clinical histories should raise the clinician’s suspicion for this syndrome, the most common of which follow.
![]() Prolonged immobilization from any cause may lead to rhabdomyolysis, especially in association with drug intoxication such as that caused by narcotics, sedative-hypnotic medications, or ethanol consumption.
Prolonged immobilization from any cause may lead to rhabdomyolysis, especially in association with drug intoxication such as that caused by narcotics, sedative-hypnotic medications, or ethanol consumption.
![]() Drug intoxication with sympathomimetics may lead to rhabdomyolysis without immobilization, including cocaine, amphetamine, or phencyclidine (PCP) abuse, or antihistamine use.
Drug intoxication with sympathomimetics may lead to rhabdomyolysis without immobilization, including cocaine, amphetamine, or phencyclidine (PCP) abuse, or antihistamine use.
![]() Excessive muscular activity or strenuous exercise may lead to rhabdomyolysis; see Table 53-1 for common causes.
Excessive muscular activity or strenuous exercise may lead to rhabdomyolysis; see Table 53-1 for common causes.
![]() Injuries that can cause a compartment syndrome or prolonged muscular compression such as crush injuries, heat stroke, and electrical injuries may lead to rhabdomyolysis.
Injuries that can cause a compartment syndrome or prolonged muscular compression such as crush injuries, heat stroke, and electrical injuries may lead to rhabdomyolysis.
![]() Certain diseases or disease states are associated with rhabdomyolysis such as polymyositis, dermatomyositis, and neuroleptic malignant syndrome.
Certain diseases or disease states are associated with rhabdomyolysis such as polymyositis, dermatomyositis, and neuroleptic malignant syndrome.
![]() Common complaints include muscle ache/stiffness, malaise, muscle tenderness (especially thigh or calf muscle), and dark-colored urine. However, these signs and symptoms are neither sensitive nor specific.
Common complaints include muscle ache/stiffness, malaise, muscle tenderness (especially thigh or calf muscle), and dark-colored urine. However, these signs and symptoms are neither sensitive nor specific.
DIAGNOSIS AND DIFFERENTIAL
![]() Diagnosis is made by measuring the serum creatinine kinase (CK). An elevation of at least five times the upper limit of normal, with the exclusion of cardiac etiologies is diagnostic of rhabdomyolysis.
Diagnosis is made by measuring the serum creatinine kinase (CK). An elevation of at least five times the upper limit of normal, with the exclusion of cardiac etiologies is diagnostic of rhabdomyolysis.
![]() The serum CK rises 2 to 12 hours after the initial injury, and peaks 1 to 3 days after the injury resolves.
The serum CK rises 2 to 12 hours after the initial injury, and peaks 1 to 3 days after the injury resolves.
![]() Myoglobinuria can be detected once plasma myoglobin concentration exceeds 1.5 milligrams/dL.
Myoglobinuria can be detected once plasma myoglobin concentration exceeds 1.5 milligrams/dL.
![]() The presence of heme on the urine dipstick without observing blood cells on microscopy is a diagnostic clue.
The presence of heme on the urine dipstick without observing blood cells on microscopy is a diagnostic clue.
![]() Obtain CK levels and basic metabolic studies for all patients suspected of having rhabdomyolysis.
Obtain CK levels and basic metabolic studies for all patients suspected of having rhabdomyolysis.
EMERGENCY DEPARTMENT CARE AND DISPOSITION
![]() The primary focus is intravenous hydration with crystalloids. Typically, several liters of normal saline are given; use caution in patients who cannot tolerate rapid infusions of fluid.
The primary focus is intravenous hydration with crystalloids. Typically, several liters of normal saline are given; use caution in patients who cannot tolerate rapid infusions of fluid.
![]() Urinary alkalinization is often performed, but has not been clearly demonstrated to improve outcome.
Urinary alkalinization is often performed, but has not been clearly demonstrated to improve outcome.
![]() Electrolytes should be monitored carefully as therapy is given in severe cases.
Electrolytes should be monitored carefully as therapy is given in severe cases.
![]() Phosphorus and should only be treated when above 7 milligrams/dL or below 1 milligram/dL.
Phosphorus and should only be treated when above 7 milligrams/dL or below 1 milligram/dL.
![]() Hyperkalemia requires aggressive therapy (see Chapter 6); avoid agents that would dehydrate the patient.
Hyperkalemia requires aggressive therapy (see Chapter 6); avoid agents that would dehydrate the patient.
![]() Monitor urine output closely.
Monitor urine output closely.
![]() Avoid potentially nephrotoxic drugs, if possible.
Avoid potentially nephrotoxic drugs, if possible.
![]() Hydrate patients with mild rhabdomyolysis without comorbidities in the emergency department, after which they may be discharged.
Hydrate patients with mild rhabdomyolysis without comorbidities in the emergency department, after which they may be discharged.
![]() Admit patients with acute kidney injury, significant comorbid conditions, or marked elevations in the CK.
Admit patients with acute kidney injury, significant comorbid conditions, or marked elevations in the CK.
![]() Complications include acute kidney injury, hyper-calcemia (late), hyperphosphatemia (early), hypo-phosphatemia (late), hyperkalemia, hyperuricemia, hypocalcemia, and disseminated intravascular coagulation.
Complications include acute kidney injury, hyper-calcemia (late), hyperphosphatemia (early), hypo-phosphatemia (late), hyperkalemia, hyperuricemia, hypocalcemia, and disseminated intravascular coagulation.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree



