RESPIRATORY DISTRESS
DEBRA L. WEINER, MD, PhD AND J. KATE DEANEHAN, MD, RDMS
Respiratory distress is one of the most common chief complaints of children seeking medical care. It accounts for nearly 10% of all pediatric emergency department visits and 20% of visits of children younger than 2 years. Twenty percent of patients admitted to the hospital and 30% of those admitted to intensive care units are admitted for respiratory distress. Primary respiratory processes account for approximately 5% of deaths in children younger than 15 years and 20% in infants. In addition, respiratory distress contributes substantially to deaths in patients with other primary processes. Respiratory arrest is one of the five leading causes of death in pediatric patients. Respiratory distress results from interruption of the respiratory or ventilatory pathway. Respiratory failure is caused by an inability to meet metabolic demands for oxygen (O2) or by inadequate carbon dioxide (CO2) elimination. Respiratory distress is usually reversible, but failure to treat the condition may result in cardiac arrest with long-term neurologic sequelae or death.
PATHOPHYSIOLOGY
The primary goals of respiration are to meet metabolic demands for O2 and to eliminate CO2. Secondary functions include acid–base buffering, host defense, and hormonal regulation. The upper airway or conducting zone, which includes the nose, nasopharynx, oropharynx, larynx, trachea, major bronchi, and terminal bronchioles, serves as a conduit for air movement. The lower airway, or respiratory zone, consists of respiratory bronchioles, alveolar ducts, sacs, alveoli and interstitium. Exchange of O2 and CO2 between the lungs and the blood occurs at the alveolocapillary membrane and depends on adequate and appropriately matched ventilation and perfusion.
Control of respiration is mediated by central and peripheral neural mechanisms. Respiration is an intrinsic brainstem function of the respiratory centers of the medulla. It is further influenced by the cerebellum, which alters respiration with postural change; by the hypothalamus, which controls respiration on a moment-to-moment basis; by the limbic system, which modulates respiration in response to emotion; and by the motor cerebral cortex, which controls volitional respiratory activity, including hyperventilation and hypoventilation and speech. Impulses are transmitted from the brain via the vagus and spinal nerves to the larynx, trachea, bronchi, bronchioles, and acini; the glossopharyngeal to the pharynx; the hypoglossal (CN XII) to the tongue; and the spinal accessory (CN XI) to accessory muscles. Cervical nerves (C2 to C4), the phrenic nerve (C3 to C5), and the intercostal nerves (T1 to T12), innervate accessory muscles, the respiratory diaphragm, and intercostal muscles, respectively.
Respiratory distress results from dysfunction or disruption of the respiratory tract and/or systems that control or modulate respiration.
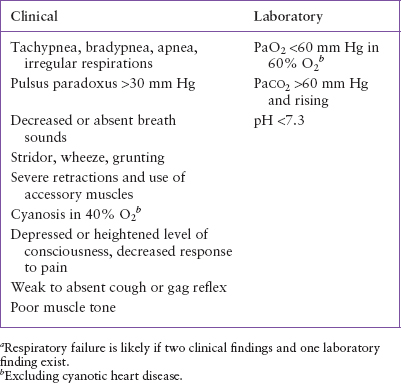
Respiratory failure is the inability to meet the metabolic demand for O2 (hypoxia) or the inability to eliminate CO2 (hypercapnia). Criteria for defining respiratory failure vary widely; one set of criteria is presented in Table 66.1. Hypoxia can be categorized on the basis of mechanism. Arterial hypoxemia results from an inability to deliver adequate O2 to the blood, most often, due to airway obstruction, central respiratory depression or impairment, neuromuscular or skeletal insufficiency, or restricted lung expansion. Other causes include low atmospheric PO2 (e.g., high altitude), diffusion impairment (e.g., pulmonary edema, pulmonary fibrosis, acute respiratory distress syndrome, O2 toxicity), anatomic or physiologic shunt (e.g., atelectasis, pneumonia, abnormal pulmonary blood flow), or increased metabolic demand (e.g., exercise, systemic illness). Anemic hypoxia is the result of the blood’s inability to deliver adequate O2 to tissues as a result of decreased hemoglobin oxygen-carrying capacity. It is caused by anemia (deficiency of red blood cells or of erythrocyte hemoglobin concentration) abnormal hemoglobin, carboxyhemoglobin, or methemoglobin. Hypokinetic, ischemic, or stagnant hypoxia also results in an inability of the blood to transport O2 to the tissues. This type of hypoxia is caused by decreased blood flow to a localized area secondary to compromised cardiac output (e.g., cardiac failure), poor tissue perfusion (e.g., shock), sludging (e.g., polycythemia), or obstructed flow (e.g., vascular obstruction). Histotoxic hypoxia results from inability to metabolize O2 at the tissue level as a result of inactivation of metabolic enzymes (e.g., by a chemical such as cyanide). Hypercapnia is caused by inadequate alveolar ventilation (e.g., central nervous system [CNS] depression, spinal cord injury, neuromuscular disease, diaphragmatic dysfunction), ventilation–perfusion imbalance with relative hypoventilation (e.g., restrictive airway disease, pulmonary embolism), or increased CO2 production (e.g., metabolic/endocrine disturbance). Hypercapnia often contributes to respiratory failure as a result of hypoxemia and is less commonly the primary cause.
Infants are at an increased risk of respiratory distress compared with children and adults because of anatomic and physiologic differences (Table 66.2). These differences result in greater risk of airway obstruction, less efficient respiratory effort, limited respiratory reserve, and dysfunction of CNS respiratory control.
DIFFERENTIAL DIAGNOSIS
Establishing a diagnosis for respiratory distress in part depends on localizing the pathology to a particular organ system. Respiratory distress may result directly from a disturbance of the upper or lower respiratory system. It may also be caused by inability of the CNS or peripheral nervous system to interpret or process respiratory requirements, or of the musculoskeletal system to perform the work of breathing. Alternatively, disease or dysfunction of other organ systems may indirectly result in respiratory disturbance by compromising respiratory system function or by stimulating compensatory respiratory mechanisms (Tables 66.3–66.5). Although respiratory effort can be immediately supported, treatment of the underlying cause is essential for definitive treatment of the respiratory distress.
TABLE 66.1
Criteria for Respiratory Failurea
Respiratory System
Respiratory distress may be caused by upper or lower airway obstruction or by disorders of the parenchyma or interstitium. Upper airway obstruction is common in infants and young children in part because of their airway anatomy and physiology (see Chapter 70 Stridor). The hallmark of complete upper airway obstruction is inability to phonate, that is, no speech, cry, or cough. Manifestations of upper airway obstruction may also include nasal flaring, stertor or snoring, gurgling, drooling, dysphagia, hoarseness, stridor, retractions, and paradoxical chest/abdominal wall movement. In neonates, common causes include nasal obstruction, upper airway anomalies (particularly laryngotracheomalacia), and congenital or postintubation subglottic stenosis. Common causes for upper airway obstruction in infants and children include croup, adenotonsillar hypertrophy, foreign body, retropharyngeal abscess, and tracheitis. Airway edema can be secondary to trauma, thermal or chemical burn, or anaphylaxis. Epiglottitis, although less common, is one of the most life-threatening causes of respiratory distress and is a true emergency. The incidence of epiglottitis has declined significantly since routine immunization against Haemophilus influenzae type b, the pathogen that once caused at least 75% of cases. Epiglottitis should be suspected in children who have abrupt onset of fever, dysphagia, drooling, muffled voice, labored respirations, and stridor. Children appear toxic and anxious and assume a sniffing position with protruding jaw and extended neck. These children are at risk of abrupt onset of respiratory arrest from obstruction. Peritonsillar and retropharyngeal abscess may present with symptoms similar to epiglottitis but are less likely to have stridor and the onset is more gradual. Croup or laryngotracheobronchitis is the most common cause of upper airway obstruction in children 3 months to 3 years of age. Croup causes subglottic narrowing and is characterized by a barky cough, inspiratory stridor, and hoarseness that are worse at night. Viral croup is most often caused by parainfluenza virus, frequently with several days of upper respiratory infection symptoms, which may or may not be accompanied by fever. Respiratory distress often occurs with wakening during the night in a child who was relatively well before going to sleep. Children with croup-like symptoms that are recurrent or prolonged may have an underlying fixed or functional airway abnormality, most commonly subglottic stenosis or hemangioma. Children with chronic stridor, particularly those younger than 2 years, may also have an underlying congenital anomaly. Tracheitis, an infection of the trachea, may occur as a primary infection with abrupt onset, high fever similar to epiglottitis. More commonly, it presents as a secondary infection in a child with an initial croup-like illness but with a worsening clinical course. Although tracheitis is usually due to bacteria, most commonly streptococcus or staphylococcus, cases in which only viruses or no pathogen is identified are not uncommon. Foreign-body aspiration, which has a peak age of occurrence of 1 to 5 years, may cause obstruction of the upper or lower airway and is a leading cause of accidental death in toddlers. A history of abrupt onset of choking or gagging is suggestive. Drooling, dysphagia, and stridor suggest an upper airway foreign body, whereas unilateral wheeze, particularly first-time wheeze with acute onset, suggests lower airway position. Presentation, particularly with lower airway foreign body, may be delayed by days to weeks from time of aspiration.
TABLE 66.2
ANATOMIC/PHYSIOLOGIC DIFFERENCES IN INFANT/CHILD AND ADULT AIRWAYS
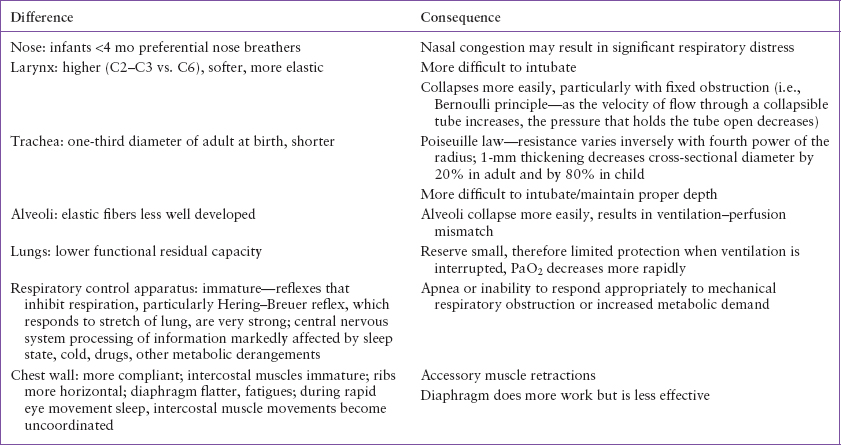
TABLE 66.3
CAUSES OF RESPIRATORY DISTRESS
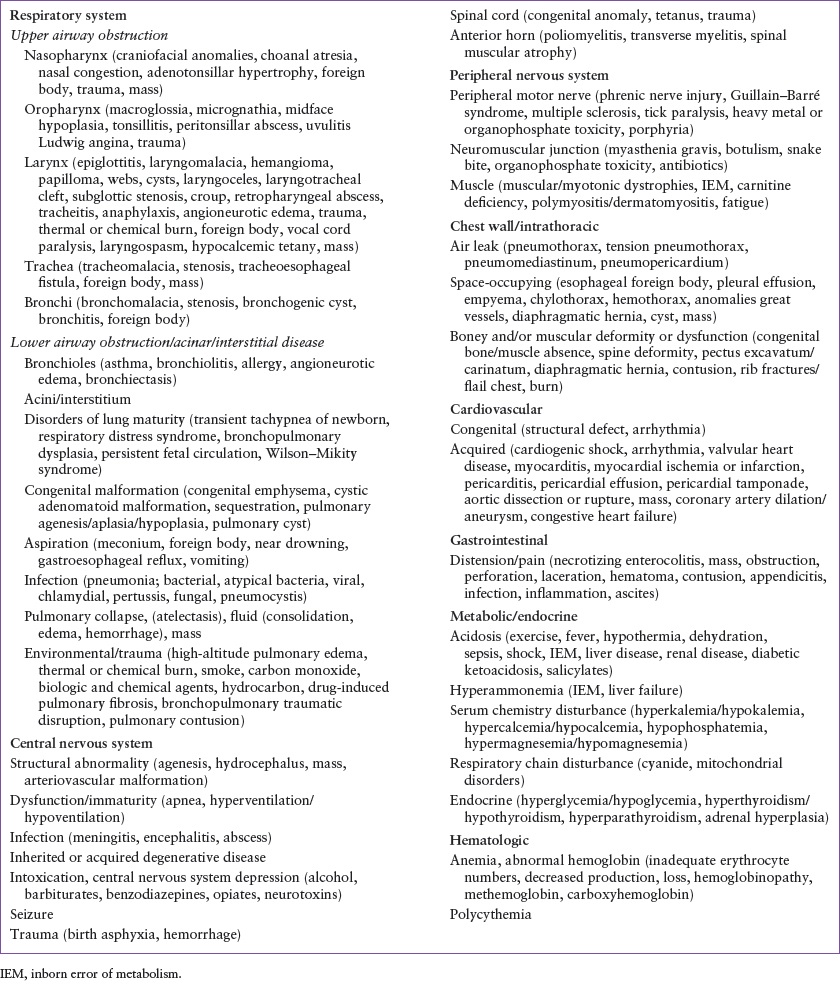
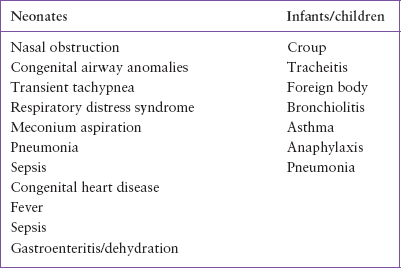
TABLE 66.4
MOST COMMON CAUSES OF RESPIRATORY DISTRESS
Common causes of lower airway obstruction involve inflammation and bronchospasm and include asthma, allergy/anaphylaxis, and bronchiolitis. Wheeze, most often diffuse, is usually a predominant feature of these conditions (see Chapter 80 Wheezing). Asthma may be triggered by infection, exercise, environmental irritants, stress, and/or gastroesophageal reflux. Allergy, usually accompanied by coryza, congestion, mucosal edema, and/or rash, may be in response to environmental exposures, food, or medications. Bronchiolitis may be caused by respiratory syncytial virus as well as parainfluenza, influenza, adenovirus, metapneumovirus, and less commonly other viruses. It is the most common cause of lower respiratory illness in children younger than 2 years. These conditions cause airway obstruction by decreasing airway luminal area secondary to bronchospasm, edema, or thickening of the wall of the lumen. Lower airway obstruction is also caused by filling of the airway lumen by excessive secretions (e.g., from inflammation, infection, or toxin such as organophosphate) or aspirated fluids. External compression can also lead to a decrease in lumen (e.g., with emphysema and masses).
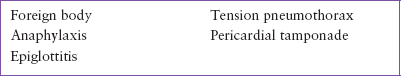
TABLE 66.5
MOST COMMON ACUTE LIFE-THREATENING CAUSES OF RESPIRATORY DISTRESS
Disorders of the alveoli and interstitium involve pus or fluid collection, collapse, and structural or functional abnormality. Alveolar and interstitial disease is characterized by tachypnea, cough, grunting, crackles, rhonchi, wheeze, and decreased and/or asymmetric breath sounds with or without fever. In neonates, transient tachypnea of the newborn and meconium aspiration are common causes. Pneumonia is one of the most common causes of lower airway disease in children of all ages. Findings are more likely to be localized in the setting of bacterial pneumonia, whereas patients with viral and atypical pneumonias (e.g., Mycoplasma infection, Chlamydia infection, and pertussis) tend to have diffuse peribronchial, interstitial processes. Patients presenting during epidemics of severe respiratory illness secondary to coronavirus infections (e.g., SARS and MERS) also commonly have fever, chills, cough, and respiratory distress which can be life-threatening. Less commonly, aspiration, hemorrhage, and pulmonary edema cause fluid collection in the acini and interstitium. Atelectasis, or airway collapse, resulting from loss of air within the pulmonary parenchyma often occurs secondary to other processes, including pneumonia, particularly viral; bronchospasm; and inadequate lung expansion, most often resulting from pain, neuromuscular disease, or inactivity. Structural and/or functional abnormalities include bronchopulmonary dysplasia, respiratory distress syndrome, bronchiectasis (most commonly seen in cystic fibrosis), congenital or acquired emphysema, and pulmonary fibrosis (usually from radiation and chemotherapy).
Several biologic and chemical agents that are potential weapons of terrorism or warfare produce respiratory distress as their most predominant effect. These include the biologic agents inhalational anthrax, pneumonic plague, pneumonic tularemia, melioidosis; the toxins Staphylococcus enterotoxin B and ricin; and the chemical agents chlorine and phosgene (see Chapter 136 Biological and Chemical Terrorism). Respiratory findings include cyanosis, chest pain, cough, hemoptysis, dyspnea, tachypnea, stridor, rales, and/or wheeze. Chest radiographs may reveal infiltrates, pulmonary edema, pleural effusions, widened mediastinum, abscesses, and/or granulomas.
Nervous System
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree







