Fig. 44.1
Ganesha, the elephant-headed Hindu god of new beginnings (eighteenth century, Temple Relic) Credit—British Museum, Public Domain
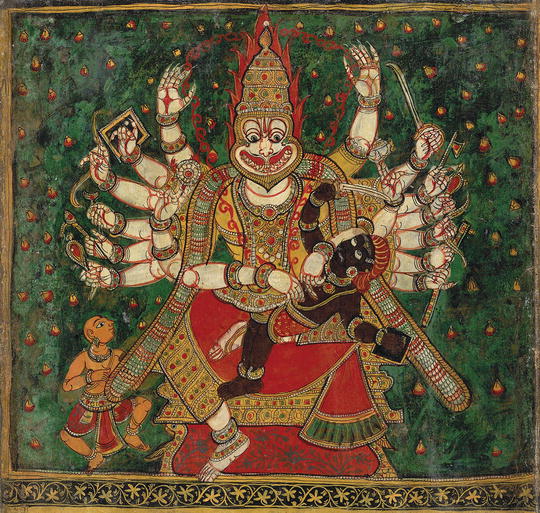
Fig. 44.2
Narasimha, the lion-headed fourth avatar of Vishnu killing the demon Hiranyakashipu on his lap, as Prahlada watches at the left. Credit—eighteenth century, British Museum, Public Domain
The Edwin Smith Papyrus is the oldest known record of the use of local flaps in reconstruction of tissue defects (circa 3000 BC). In 600 BC, the Indian surgeon Sushruta described the earliest forehead flap for nasal reconstruction, the principles of which are still in use today [13]. There are many examples of twin saints with divine healing powers throughout mythology (Ashvins of Rig Veda and the Greco-Roman Dioscuri). Similar accounts exist for the Middle Ages (the Christian patron saints, Cosmas and Damian) [14, 15].
The Middle Ages and Renaissance
Cosmos and Damian, the patron saints attributed to have performed the first extremity transplantation were twin brothers who lived in Egaea, in Cilicia (current day Turkey) in the third century [16].They were known to possess acclaimed powers of healing, which lead to suspicions of mysticism and their death due to persecution in 283AD. Per legend, these martyr saints are credited to have grafted a leg from a deceased Ethiopian in a patient (deacon Justinian) who suffered an amputation of a cancerous limb. This work of Cosmas and Damian is depicted in artistic works by Matteo di Paccino (1350–75); J. Huguet (1415–92), or Fra Angelico (c.1438) (Fig. 44.3) [17, 18].


Fig. 44.3
Saints Cosmas and Damian performing a miraculous cure by transplantation of a leg. c. 1495 (by artist Master of Los Balbases) Credit—Church of Saints Cosmas and Damian, Burgos, Northern Spain. Featured in a book Legenda Aurea by Jacobus de Voragine, c. 1275
The Recent Era
Throughout history, the desire to restore and replace diseased or damaged body parts has been ingrained in human ethos and psyche. However all claims of success with ancient transplantation remained rooted in misleading myth, legend and folklore, or in the realms of philosophical or science fiction for ages [19]. It was not until the mid-twentieth century that the mysteries of immune rejection of grafts were first unraveled, ushering the “fictional-reality” of solid organ or reconstructive transplantation, which was more than a literary oxymoron [20].
The modern era of RT begins with the injuries sustained in World War II that spawned the seminal immunologic work of Medawar, Billingham, and Brent in skin grafts. Scores of Allied sailors and pilots suffering with devastating burn injuries were admitted to the Plastic Surgery unit in Glasgow, Scotland for treatment. It was here that biologist Peter Medawar was investigating the immunogenicity of skin with his colleagues Billingham and Brent. He joined plastic surgeon, Thomas Gibson who performed the first skin allografts in these Allied soldiers. Medawar’s groundbreaking research earned him the Nobel Prize for Medicine in 1960 and later, Knighthood [21].
In 1954, Joseph E. Murray, who was a plastic surgeon, along with his colleagues John P. Merrill and Harwell J. Harrison performed the first kidney isograft between identical twins [22–25].Shortly after, in 1957, Earle Peacock, also a plastic surgeon, transplanted en bloc a digital flexor tendon mechanism. Peacock called this a “composite tissue allograft” (now termed as vascularized composite allograft) [26, 27]. In 1959, Murray and team went on to perform the first successful kidney allograft [28]. Although Murray used total body irradiation for his first transplant, he pioneered in association with Roy Calne, the clinical use in renal transplants of azathioprine (Imuran), a drug discovered by Hitchings and Elion [29, 30]. Murray became the only plastic surgeon in history to receive the Nobel Prize.
Over the next 50 years, successful solid organ transplantation was spurred by advancements in pharmacologic immunosuppression. In 1964, almost a decade after Murray’s and Peacock’s first attempts with organ and composite grafts, Roberto Gilbert Elizalde a young general surgeon in Guayaqil, Ecuador attempted the first unilateral hand transplantation in a sailor that underwent bilateral amputations (Fig. 44.4) [31, 32]. Although Gilbert used the same immunosuppression as that of Murray and Calne (azathioprine and prednisone), the graft failed at 3 weeks, necessitating amputation due to irreversible rejection [33].
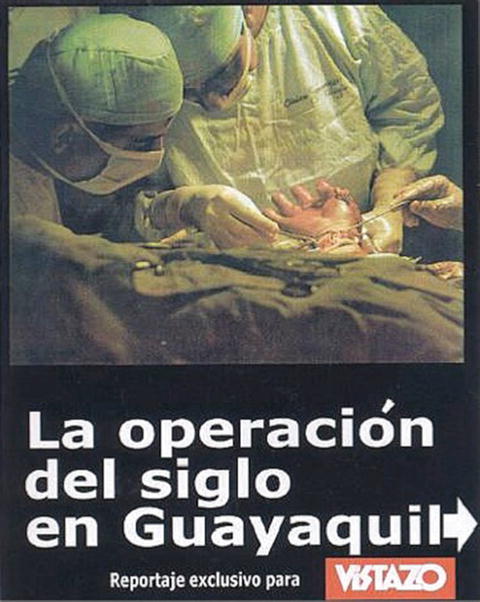
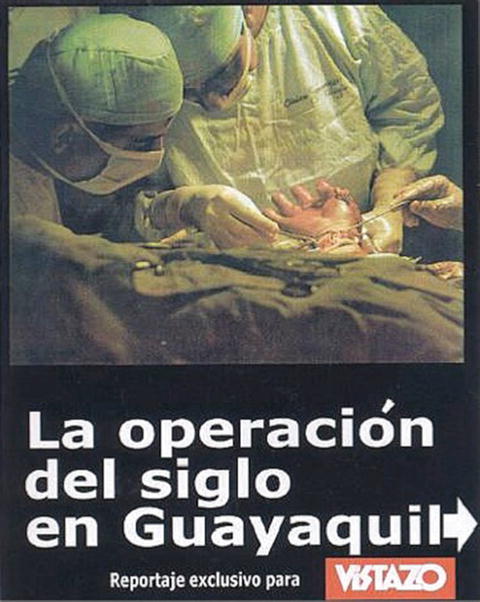
Fig. 44.4
The first hand transplantation in modern human history. Dr. Roberto Gilbert and Dr. Gabriel Panchana performing a hand transplant in a sailor, Julio Luna in Guayaquil, Equador in February 1964. Credit—Vistazo Magazine, Ecuador
The discovery and clinical approval of novel and more effective immunosuppressive drugs such as cyclosporine (CsA) in 1980s improved the success of solid organ transplantation but was toxic in limb transplant studies in non human primates [34, 35]. These results reinforced scientific dogma that skin was an insurmountable antigenic barrier to conventional immunosuppression, hampering research progress.
It was drugs such as tacrolimus and mycophenolic acid mofetil discovered in the 1990s [36], that enabled reproducible survival of skin bearing limb transplants in small animals (rodents) and large animals (pigs) [37]. It was also not until the early 1990s when skin grafts placed synchronously in renal transplant patients successfully survived with routine immunosuppression [38, 39]. These developments and insights were watershed moments that overturned prevailing dogma about skin antigenicity in reconstructive transplants, spawning the groundbreaking field of vascularized composite allotransplantation (VCA) [40].
The first skin bearing upper extremity allotransplants under modern combination immunosuppression (tacrolimus, mycophenolate mofetil and prednisone) were performed in the late 1990s. Jean-Michel Dubernard and team performed the world’s first unilateral hand transplant in September 1998 in Lyon, France [41] followed by the first hand transplant in the USA by Warren Breidenbach and team in January 1999 in Louisville, Kentucky [42]. Ever since, the field of RT has expanded and rapidly emerged to become one of the most promising, challenging, and controversial fields of solid organ transplantation [43].
This chapter reviews the world experience, ethical considerations, and emerging prospects in this exciting field.
World Experience
Reconstructive Transplantation: State of the Art
Unlike routine solid organ transplantation (SOT), RT involves transplantation of composites of multiple tissue types that may include skin, muscle, tendon, vessel, nerve, bone, cartilage, lymph nodes, and bone marrow [44]. Since these grafts are derived from either deceased (or in some cases living donors), and since they are “primarily vascularized,” the Organ Procurement and Transplantation Network (OPTN) has recently enacted policy changes to designate these VCAs as “solid organs” for the purposes of donation and transplantation [45].
The reconstructive ladder is the cornerstone of soft tissue reconstruction with treatment principles that are tiered from the simplest to the most complex [46]. Transfer of vascularized tissues across sites in the body has been the most complex step in the reconstructive ladder. Advancements in microsurgery over the past 50 years have enabled the transfer of functional units of muscle and nerve as well as allowed expansion and prefabrication of flaps prior to transfer [47]. The advent of RT and progress in transplant immunology has allowed VCA to replace free tissue transfer and overcome its inherent limitations in reconstructive surgery by eliminating donor site morbidity secondary to use of autologous tissues for major tissue loss [48].
Undoubtedly, VCAs when successful have the potential to restore the appearance, anatomy, and function of debilitating or devastating civilian or combat injuries, not conducive to conventional reconstruction. Successful RT procedures can also avoid the need for multiple revisions or achieve superior functional and/or aesthetic outcomes, without the high costs of multiple surgeries/hospitalizations seen in conventional reconstruction [49, 50].
RT is now the new realm of solid organ transplantation. Despite such promising initial results, growth of this groundbreaking field has been slow, primarily due to concerns for risks of lifelong, high-dose, multidrug immunosuppression. Unique from solid organs, RT allow visual monitoring, directed biopsies and enable timely, site-specific therapeutic interventions, which may help sustain rejection-free RT survival, while minimizing/eliminating the risks of chronic systemic immunosuppression [51].
Unlike SOT, RT offers unique opportunities for graft access (targeted therapies) and monitoring (clinicopathologic correlation of rejection). Yet current “state of the art” RT management is with chronic systemic or adjunctive topical immunosuppression with morbidity, risks, and complications (including deaths) that have been reported in RT recipients of VCA [52].
Emerging Insights
Devauchelle and team in Amiens, France performed the first facial VCA in 2005, 5 years after the first upper extremity transplantations. The recipient had tissue loss due to a dog bite involving the mid face (lips, nose, central cheeks) [53–56]. This patient and the first Louisville patient respectively remain the recipients of the longest surviving face transplant (11 years) and upper extremity transplant (16 years) in the world [57, 58].
Over the past 15 years, more than 100 upper extremity transplants and over 30 craniofacial transplants have been performed across multiple centers around the world. Patient/allograft survival and immunologic/functional outcomes have been mixed, ranging from poor to suboptimal to encouraging across different VCAs. A summary of outcomes with upper extremity in the USA is shown in Fig. 44.5 and around the world in Figs. 44.6, 44.7, and 44.8 (Tables 44.1 and 44.2). The world outcomes with craniofacial transplantation are shown in Fig. 44.9 (Table 44.3).
Fig. 44.5
Total number of upper extremity allotransplantations (unilateral and bilateral) performed in the USA
Fig. 44.6
Total number of upper extremity allotransplantations (unilateral) performed in the world
Fig. 44.7
Total number of upper extremity allotransplantations (bilateral) performed in the world
Fig. 44.8
World experience with uppe r extremity allotransplantations (unilateral and bilateral) performed in the world
Table 44.1
Outcomes in upper extremity transplantation : world experience
Country | Center | Total number of UE transplants | Number of graft losses | Mortalities | Reported in lay media | Reported in peer literature |
|---|---|---|---|---|---|---|
Australia | Melbourne | 1 | ||||
Austria | Innsbruck | 9 | ||||
Belgium | Brussels | 1 | ||||
China | Six centers | 15 | 7 | No | Yes (partially) | |
France | Lyon | 11 | 1 | Yes | Yes | |
Paris | 2 | 2 | 1 | Yes | Yes | |
Germany | Munich | 2 | ||||
India | Kochi | 4 | ||||
Iran | Tehran | 1 | 1 | No | No | |
Italy | Milan | 3 | ||||
Monza | 2 | |||||
Malaysia | Selayang | 1 (twin–twin) | ||||
Mexico | Mexico City | 4 | 2 | 1 | Yes | Yes |
Poland | Wroclaw | 7 | 1 | No | ||
Spain | Madrid | 2 | ||||
Valencia | 6 | |||||
Turkey | Ankara | 2 | 2 | 1 | Yes | Yes |
Antalya | 8 | 2 | 1 | Yes | No | |
UK | Leeds | 1 | ||||
Total world | 82 | 18 | 4 |
Table 44.2
Outcomes in upper extremity transplantation : US experience
Center | Total number of UE transplants | Number of graft losses | Mortalities | Reported in lay media | Reported in peer literature |
|---|---|---|---|---|---|
Brigham and Women’s Hosp | 4 | 2 | No | No | |
Emory | 3 | 2 | No | No | |
U. Pittsburgh/Johns Hopkins | 12 | 2 | No | No | |
MGH | 1 | ||||
U. Louisville | 9 | 2 | 1 | Yes | No |
UCLA | 1 | 1 | No | No | |
U. Pennsylvania | 4 | ||||
Wilford Hall (SAMMC) | 1 | ||||
Total | 35 | 9 | 1 |
Fig. 44.9
World experience with craniofacial allotransplantations (partial, total face, scalp, ear, and other craniofacial components) performed in the world
Table 44.3
Outcomes in craniofacial transplantation : world and US experience
Center | Total number of CF transplants | Number of graft losses | Mortalities | Reported in lay media | Reported in peer literature |
|---|---|---|---|---|---|
Brigham and Women’s Hosp | 5 | ||||
Cleveland Clinic | 2 | ||||
NYU | 1 | ||||
U. Maryland | 1 | ||||
Poland | 2 | ||||
Spain | 4 | 1 | 1 | Yes | Yes |
Turkey | 9 | 2 | 2 | No | No |
France | 9 | 1 | 1 | Yes | Yes |
Belgium | 1 | ||||
China | 1 | 1 | 1 | Yes | No |
Total | 35 | 5 | 5 |
The experience with clinical RT over the past 15 years has providing insights into the multifaceted aspects of these innovative procedures. We have learned that (1) RT is not life saving but, when successful, these procedures can enhance quality of life; (2) RT recipients are otherwise healthy without accompanying diseases but need lifelong immunosuppressive treatments that result in a range of life-shortening, quality of life limiting or even life threatening morbidity; (3) acute rejection can be monitored visually (not in all instances) which allows for timely local graft or systemic intervention; (4) topical therapies of skin potentially allow reduction or supplementation of systemic therapy; and (5) risk–benefits in RT can vary between different VCAs and thus such consideration for RT patients must be individualized for each VCA and for each defect include a comprehensive risk–benefit analysis including a robust exit strategy [59, 60].
Although the most common RT procedures are upper extremity and craniofacial VCAs, to date, close to 200 VCA procedures, including but not limited to, extremity, craniofacial, genitourinary, tracheal, or abdominal tissues have been performed at active clinical RT centers spanning the globe across most continents.
Other Types of VCA
With the advent of RT and rapid expansion of the field around the world since the 1990s, a host of other types of VCA have been performed by centers including but not limited to laryngotracheal, bone and joint, abdominal wall, uterine, penile, tongue, ear, scalp, and lower extremity transplantations. Pediatric and combination VCAs (face and upper extremity or upper and lower extremity transplants) have also been performed.
Abdominal Wall Transplantation
The first abdominal wall VCA was performed by Tzakis and colleagues in 2003 in recipients of intestinal or multivisceral transplants with loss of abdominal domain [61].These VCAs were unique as the patients were already on immunosuppression for SOT. Since then 38 full-thickness vascularized abdominal wall transplants, six partial-thickness vascularized, and 17 partial-thickness nonvascularized rectus fascia grafts have been reported worldwide [62]. Despite failures in some patients, these grafts have been used to facilitate primary, tension free closure of abdominal wall in SOT patients with visceral coverage and reduced complications [63, 64]. Taken together, despite mixed success, the numbers of abdominal wall transplantations exceeds that of craniofacial VCA.
Laryngotracheal Transplantation
Kluyskens and Ringoir performed the first laryngeal transplant in 1969 for reconstruction after tumor extirpation [65, 66]. However, the tumor recurred leading to death at 8 months and the graft was lost to rejection when immunosuppression was withdrawn. Following this early attempt, Strome and colleagues performed the first successful laryngotracheal VCA (including thyroid and parathyroid glands) in 1998 in Cleveland prior to the first upper extremity transplantation in Louisville [67, 68]. The patient who suffered from laryngeal trauma recovered swallowing and phonation with excellent quality of life outcomes until this graft was lost to chronic rejection 14 years later [69]. Following this, Tintinago et al. from Medellin, Colombia performed over 18 laryngotracheal VCA, including the first esophageal VCA [70–72]. Majority of patients were weaned from tracheostomies. There is a report of two graft losses, but this experience remains mostly unpublished with long-term outcomes unknown.
Knee Joint and Femur Transplantation
Hofmann and colleagues performed the first series of knee joint and femur VCAs in Munich between 1996 and 2006 [73]. These include six human vascularized allogeneic knee transplantations and three femoral diaphyseal transplants for long segmental bone defects [74]. All of these grafts were successful in the short term but were lost within the first 56 months due to reasons including infections, non-adherence to medications and chronic graft rejection [75, 76].
Tongue, Ear, and Scalp Transplantation
In 2003, Ewers and colleagues performed the first total tongue VCA in Vienna, Austria in a recipient following carcinoma resection [77]. Following a short period of success, the patient succumbed to tumor recurrence. In 2004, Hui and team transplanted both ears bridged by cephalocervical scalp skin in a recipients following extirpation of melanoma [78]. Again, the patient succumbed to tumor recurrence. More recently, in 2015, a team from MD Anderson Cancer Center performed a combined partial calvarial and scalp transplant in a SOT recipient suffering from a wound defect secondary to tumor removal from the scalp. Long-term outcomes remain to be seen.
Penile Transplantation
Hu et al. performed the first penis allotransplantation in Guangzhou, China in 2006, in a patient suffering from traumatic penile amputation [79]. After a short course of success with normal urination, the transplant was electively removed at 2 weeks due to psychosocial rejection experienced by the recipient and his spouse [80]. More recently, in 2014, a team lead by Andre van der Merve from South Africa performed a penis transplant in a recipient suffering from complicated circumcision [81]. A year later, this patient is reported to have ejaculatory and erectile sexual function, although it is unclear if erogenous sensation has recovered. Two programs have recently received OPTN approval to perform penile transplants in the USA.
Uterus Transplantation
The earliest attempt at uterine transplantation was in Saudi Arabia by Fageeh et al. in 2000 [82]. The graft failed at 99 days due to ischemic uterine torsion. This attempt was followed by another transplant in Antalya, Turkey, in 2013, lead by Ozkan et al. [83–85]. Both these early attempts were based on deceased donors. Despite survival of the transplant, pregnancy was not accomplished in this recipient. In 2014, Brannstrom and colleagues achieved the first successful pregnancy in uterine transplantation in a recipient with absolute uterine infertility (AUI) . This team performed a total of 9 deceased donor uterine transplants with four live births [86, 87].
Uterus transplantation may be the first available treatment for AUI, which is caused by absence of the uterus or the presence of a nonfunctional uterus. Similar to abdominal wall transplants, where the patient is usually on immunosuppression for the SOT, uterine transplants benefit from reduced immunosuppressive drug exposure (coverage only needed during gestation) [88–91].
Lower Extremity and Simultaneous Combination Reconstructive Transplantation
Four cases of lower extremity VCA have been reported (two bilateral and two unilateral) [92]. In 2006, Zuker and colleagues performed the first unilateral lower limb VCA in ischiopagus conjoined twin infants [93]. Given that this was a twin–twin VCA, postoperative immunosuppression was not needed. Over a 6-year period, the patient recovered motor and sensory function to allow ambulation with assistance [93].
In 2010, Cavadas and colleagues performed the first bilateral above knee lower extremity VCA in a 21-year-old recipient in Valencia, Spain [94, 95]. At 1 year, there was recovery of knee flexion and extension with some ankle function. In 2012, Ozkan and colleagues performed a simultaneous bilateral upper limb VCA in combination with a unilateral lower extremity VCA in Antalya, Turkey. Both the Spanish and Antalya patients succumbed after transplant, one to post transplant lymphoma and the other to post transplant end organ failure secondary to disseminated aspergillosis. In the same year, Nasir and coworkers performed a bilateral lower extremity VCA in combination with upper extremity VCA in Ankara, Turkey. The patient died perioperatively due to surgical complications [96].
Other simultaneous complex transplants have been reported across the world involving combination face and upper extremity or upper and lower extremity VCA (bilateral or unilateral) [97]. Three of four of these reported tandem transplants have died due to operative or perioperative complications that include overwhelming sepsis or shock [98, 99]. One patient survived but had to undergo removal of both upper extremities only to preserve a face transplant. Uniformly, quadruple VCA and triple VCA have been associated with very high failure. There are risks of the large antigenic burden, overwhelming ischemia–reperfusion injury, large volume resuscitation requirements, extended anesthesia times among a host of surgical and technical challenges [100].
Ethical Considerations
Ethics of Equipoise, Autonomy, Informed Consent, and Risk–Benefit Balance
Although much has been learned in hand and face transplantation, equipoise continues to be important for VCA procedures gaining recent attention (lower extremity, penis, uterus) [103]. In all attempts, old or new, the prospect of unintentional and unanticipated harm must be balanced or preferably exceeded by the potential known or anticipated. Such “equipoise” is the reasonable yet deliberate educated judgment of VCA teams initiating new programs in the uncertainty of research setting and must be accomplished prior to ethically proceeding with larger clinical trials [104].
All VCA teams must recognize the individual variability of subjects in prior life experiences, level of education and processing of information, conceptual and theoretical capacities, and subjective weight or trade-off given to estimations of benefits and risks. Any or all of these factors may affect decision making by patients [105]. “Autonomy” is the concept that addresses the respect for the subject as detailed in the Belmont Report and is defined as “at a minimum, self-rule that is free from both controlling interference by others and from limitations, such as inadequate understanding, that prevent meaningful choice” [106].
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree





