(1)
Division of Pulmonary and Critical Care Medicine, Eastern Virginia Medical School, Norfolk, VA, USA
The Chest Radiograph
Interpretation of the bedside (antero-posterior, supine) chest radiograph (CXR) is fraught by numerous pitfalls. These include:
On the AP view, the heart and mediastinum appear about 15 % wider than on an upright PA chest radiograph (false impression of cardiomegaly and mediastinal widening)
Portable chest radiographs may be difficult to interpret due to poor positioning
Pleural effusions and pneumothoraces are frequently “missed” because the patient is in the supine position
The pulmonary vasculature is distorted on supine radiographs because blood no longer flows preferentially to the lower lobes
Because lateral chest films cannot be obtained, abnormalities in the posterior costophrenic angles (retrocardiac), within the mediastinum and adjacent to the spine can easily be missed.
Interstitial infiltrates may be poorly seen on the CXR
It should be appreciated that the CXR is a 2-dimensional image of a complex 3-dimensional structure and that even on the “best” bedside CXR significant pulmonary pathology may be missed; e.g., pneumothorax, air-space consolidation, abscesses and interstitial lung disease [1]. The intensivist should therefore have a low threshold for performing a chest CT scan; however the risks of moving a patient to the radiology suite must be weighed against the possible benefits. Chest CT scans provides a more comprehensive evaluation of the lung parenchyma providing a much better assessment of the nature and extent of lung pathology than the CXR. It is likely that in the future portable CT scans will be performed routinely in the ICU [2].
Despite its inherent limitation, a careful review of the bedside AP CXR provides useful information in the management of critically ill patients. In previous years, the standard practice was to obtain daily CXR’s in all ICU patients. Recently however, a number of well conducted studies indicate that this is not a cost-effective practice and that CXR’s should only be performed on “demand”, i.e. as clinical circumstances dictate [3, 4]. These studies have demonstrated that it is rare that such an approach leads to findings that would have been missed had daily CXR been performed. A meta-analysis by Oba and Zaza which included 8 trials and 7,078 ICU patients demonstrated eliminating routine daily CXR did not affect mortality, length of stay in the hospital or ICU, or ventilator days in either group [5]. However, all patients require a CXR on admission to the ICU, after endotracheal intubation and after insertion of a subclavian or internal jugular central venous catheter [6].
The chest radiograph should be studied systematically; firstly the position of all the tubes and catheters should be evaluated, followed by an evaluation of the lung parenchyma, pleura, mediastinum and diaphragm followed by a search for signs of extra-alveolar air.
Position of Tubes and Catheters
Endotracheal tube. With the head in a neutral position the tip of the tube should be 4–6 cm from the carina. It should be noted that with movement of the head, from a flexed to an extended position, the tube can move by as much as 4 cm. A useful landmark for the tip of the ET tube is the superior border of the aortic notch (Marik’s sign) or the upper border of T4 (see Fig. 50.1). The aortic arch is the “center of an imaginary sphere” so even if the CXR is rotated, Marik’s sign can still be used to determine the position of the ET tube.
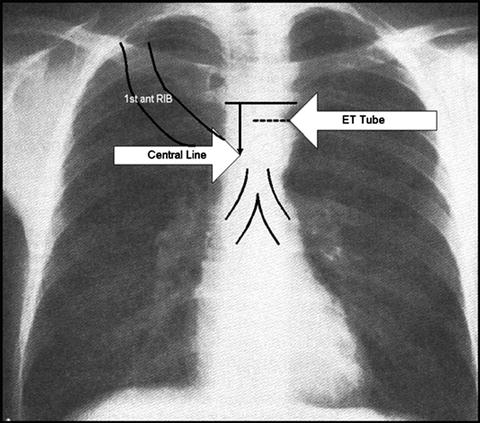
Fig. 50.1
Idealized CXR with optimal position of endotracheal tube and central line
Central venous catheters. The tip of the catheter should be located beyond the venous valves of the subclavian or internal jugular vein but proximal to the right atrium (i.e. above the superior vena cava-right atrial junction). Placement in the right atrium may result in atrial perforation. Two useful radiographic landmarks for the position of the tip of the catheter are:
the first costochondral junction
a point 2 cm inferior to a line joining inferior margins of the clavicular heads (see Fig. 50.1).
The position of other tubes and catheters, such as the nasogastric tube, feeding tube, chest tubes, intra-aortic balloon catheter and pacing wires should be noted.
Lung Parenchyma, Pleura and Mediastinum
The presence of pulmonary infiltrates should be noted. It should be noted whether the infiltrate is interstitial or alveolar (or both), unilateral or bilateral, and patchy or diffuse. An infiltrate may be caused by water (cardiogenic or non-cardiogenic pulmonary edema), cells (infection) and/or blood (pulmonary hematoma, intra-alveolar bleed). It should be appreciated that it may not be possible to distinguish between these entities by examination of the chest film alone. The following radiographic findings may help distinguish cardiac and non-cardiac pulmonary edema:
Non-cardiac pulmonary edema (acute lung injury)
normal heart shape
absence of septal lines
no peribronchial cuffing
frequent air bronchograms
patchy increased lung density
peripheral increased lung density
Cardiogenic pulmonary edema
base-to-apex blood flow inversion
even distribution of increased lung density
septal lines
peribronchial cuffing
It is however critically important to appreciate that the CXR is a very poor indicator of volume status. A number of studies in diverse patient populations have demonstrated a poor relationship between CXR assessment of volume status and measurement of lung water (EVLW) even when interpreted by expert chest radiologists [7–11].
In the supine position fluid tracks posteriorly resulting in a diffuse haziness of the lung fields. It is therefore very easy to miss a significant pleural collection. Fluid collections can be confirmed by ultrasonography. The width of the mediastinum should be noted (normal; <10 cm) as well as the presence of mediastinal nodes or masses.
The traditional apico-lateral collection of air may not be present on a portable CXR in patients with pneumothoraces. Free air will often be located in the anterior costophrenic sulcus as this is the most superior portion of the pleural space in the supine patient. Other radiographic signs of a pneumothorax in the supine position include; a relative hyperlucency over the upper abdominal quadrants and a deep costophrenic angle (the deep sulcus sign). It should be noted that the sensitivity of the supine AP chest radiograph for the diagnosis of pneumothorax averages 50 % [12]. This compares to a sensitivity of >95 % for ultrasonography [13].
The portable chest radiograph is not ideal for evaluating the hilum and lung parenchyma. Conventional and high resolution computed tomography (HRCT) may be useful for evaluating aortic dissection, pleural disease, the lung parenchyma (especially in immunocompromised patients with pulmonary infiltrates), characterization of diffuse infiltrative pulmonary disease and evaluation of suspected masses in the mediastinum or hilum. Routine CT evaluation of the chest can be done with or without intravenous administration of contrast media. Contrast is reserved for those cases in which mediastinal or hilar pathology are suspected. HRCT differs from conventional CT not only in the use of a thinner X-ray beam (e.g. 1.5 mm vs 1 cm), but also the use of digitized X-ray construction which allows for better spatial resolution and for more detailed images of the lung parenchyma. HRCT is therefore useful in the evaluation of patients with diffuse infiltrative lung diseases. Spiral CT differs from conventional CT primarily in that it allows continuous scanning of the patients. In spiral CT, the X-ray tube makes continuous 360-degree revolutions without interruption. The patient is moved through the circulating beam at a predetermined speed, and imaging information is then obtained as a solid cylinder, instead of one slice at a time. Spiral CT is most helpful in evaluating lesions at or near the diaphragm (less motion artifact), evaluating vascular structures (main pulmonary arteries in suspected pulmonary embolism) and small pulmonary nodules.
While CT scanning has revolutionized imaging in critically ill patients it comes at the expense of increased radiation exposure. Recent publications have emphasized the potential future cancer risk from radiation exposure due to CT examinations [14]. It is estimated that 1 individual in 1,000 will develop cancer from an exposure to 10 milliSieverts (mSv) of low-dose radiation [15]. Lutterman et al. estimated the cumulative radiation exposure of hospitalized patients from radiological imaging [16]. The mean dose estimate per ICU patient was 17.9 mSv with CT scans accounting for 82 % of the radiation dose. The estimated radion exposure by radiographic study is listed in Table 50.1 [16]. This data is somewhat alarming and suggests that patients’ cumulative radiation exposure should be monitored during their hospitalization.
Table 50.1
Average radiation exposure for common radiologic studies
Examination | mSv |
|---|---|
PA chest | 0.02 |
Abdomen radiograph | 0.7 |
Ventilation/perfusion lung scan | 2.0 |
Cardiac perfusion isotope scan | 15
Stay updated, free articles. Join our Telegram channel
Full access? Get Clinical Tree
 Get Clinical Tree app for offline access
Get Clinical Tree app for offline access

|


