Fig. 38.1
The diagnosis of facet joint pain
Common Diagnoses/Symptoms Treated
Common diagnoses relating to the z-joint include cervical, thoracic, or lumbar facet arthropathy, facet syndrome, and spondylosis. Several other diagnoses often implicate the z-joint as a potential source of pain including whiplash syndrome, cervicogenic headache, and degenerative spondylolisthesis. The z-joints can cause a variety of symptoms including both local axial pain and referred extremity pain. In the cervical spine, the z-joints often cause pain in well-known distributions [12] (Fig. 38.2), with the upper cervical joints capable of causing headaches. Referral patterns from the lumbar z-joints are less specific [11, 13]. No historical features have proven pathognomonic for identification of z-joint pain, but these patients often complain of sharp or aching pain that is worse with loading the joint, such as during spine extension or extension with rotation or with stretching the capsule of the joint, such as extremes of flexion or rotation. Isolated z-joint pain should not cause burning, tingling, numbness, or extremity weakness typical of neuropathic processes. Common diagnoses are described in more detail in the subsections below.
Fig. 38.2
Classical pain referral patterns in cervical z-joints
Cervicogenic Headaches from the C2-3 Joint
The cervical spine is often overlooked as a potential source for chronic headaches. Cervicogenic headaches are those that appear to emanate from the upper cervical spine and tend to create headaches in the suboccipital region, with occasional radiation into the forehead. They can be unilateral or bilateral and are often mistaken for migraines or tension-type headaches. Cervicogenic headaches can evolve from any of the upper cervical spine segments , including the C0-1 (atlanto-occipital (AO) joint), C1-2 (atlanto-axial (AA) joint) , and the C2-3 or C3-4 z-joints. Of these potential sources, the C2-3 z-joint has been identified as the cause of cervicogenic headaches 54% of the time [14] and is considered the most common source of chronic post-whiplash headaches [10, 15]. Biomechanical factors can predispose to upper cervical z-joint pain, including a forward-head position with resultant upper cervical hyperextension. Cervicogenic headaches from the C2-3 z-joint can be reliably confirmed via third occipital nerve block or well-placed intra-articular injection of anesthetic and treated with RFN .
Neck Pain from Cervical Z-Joints C3-4 to C6-7
The cervical z-joints refer pain in classic referral patterns (Fig. 38.2). These joints should be considered as potential sources of pain in anyone with neck pain referring to the upper trapezius and/or periscapular regions. The cervical z-joints are commonly the source of chronic axial neck pain in older patients or following whiplash-type injuries [15]. The most commonly affected z-joints in whiplash are C2-3 followed by C5-6 [10, 15], while degenerative osteoarthritis most commonly affects C3-4 and C4-5 [13]. Adjacent segments to prior cervical fusions are predisposed to z-joint arthropathy. It is especially important to identify the cervical z-joints as sources of chronic pain because this condition is potentially treatable without surgery.
Low Back Pain from the Lumbar Z-Joints
In a general population, at least 15% of low back pain is z-joint mediated [16]. The prevalence rises to 40% in older patients (median age 59 years) with chronic back pain [16]. Assuming typical anatomy, the lumbar z-joints begin with L1-2 and extend to L5-S1. The most commonly affected joints are L4-5 and L5-S1. Atypical lumbosacral transitional anatomy, such as a sacralized lumbar vertebra or a lumbarized sacral vertebra, occurs 10–20% of the time [17]. The referral patterns of pain from the lumbar z-joints are less well defined than those from the cervical spine. Pain can refer to the buttock, hip, groin, and proximal thigh [11]. Typically, pain is present along the corresponding paraspinal muscles and less so midline. Pain tends to be worse with loading the joints in standing, extension, and extension-rotation maneuvers, but can also be exacerbated with capsular stretch at end ranges of flexion or rotation. Many find some relief with lying down. Some associated biomechanical factors include lumbar hyperlordosis, tight hip flexors, weak core muscles, and history of lumbar fusion. When properly diagnosed and treated, individuals with chronic z-joint pain can see functional improvements with physical therapy to optimize spine mechanics and interventional treatments, such as medial branch RFN [18, 19].
Thoracic Spine Pain from Thoracic Z-Joints
Thoracic region pain is less common and less studied than cervical or lumbar pain. Among those with chronic thoracic pain, estimates suggest up to 48% emanates from the thoracic z-joints [9]. RFN of the thoracic medial branches is considered a possible treatment option, but should be considered with caution only after careful evaluation to rule out other potential sources of pain. The pain referral patterns from the thoracic z-joints can overlap considerably, which makes it difficult to isolate specific joints to target for intervention. At this time, there is insufficient literature to predict outcomes following thoracic RFN; therefore, this treatment should only be pursued when less invasive options have been exhausted. Those who perform thoracic RFN must be aware of the unique characteristics of the thoracic medial branches, including more lateral anatomic course around the transverse processes compared to the lumbar spine and more cutaneous innervation [20].
Assessment
There are currently no historical features, physical exam maneuvers, or radiographic findings that can definitively and specifically identify z-joint pain. History should focus on identification of red flag conditions, such as cancer, infection, and unstable fracture, and can help to distinguish between mechanical pain and inflammatory arthropathies, as well as to differentiate somatic pain from neuropathic pain. At a minimum, the physical exam should attempt to rule out neurological injury, identify biomechanical factors that may predispose to z-joint pain, such as forward-head position or lumbar hyperlordosis, and should include a manual examination of the painful region. Careful segmental deep palpation can identify a joint level of maximal tenderness, especially in the cervical spine. Localizing signs may be absent in the lumbar spine, but the L4-5 and L5-S1 levels are most commonly affected [16].
Diagnostic imaging options include plain X-rays , dynamic bending X-rays, MRI, CT, and single photon emission CT (SPECT) . All of these modalities can demonstrate z-joint osteoarthritis. Dynamic X-rays , including flexion and extension sequences, can show a mobile spondylolisthesis, which may support a specific joint level as being the pain generator. MRI can show increased signal in the peri-facet bone marrow, or in the z-joint itself especially on STIR sequences. SPECT can demonstrate metabolically active z-joint arthropathy that has been linked to injection response in some studies [21, 22], but involves significant radiation exposure and is not recommended for routine use. Studies continue to look at radiographic predictors of response to diagnostic blocks [23, 24]. While patients with z-joint pain are likely to have imaging abnormalities, many asymptomatic individuals also demonstrate these same findings. Furthermore, diagnostic imaging can often overlook microscopic injuries to the joint capsule or cartilage, and cannot be used to definitively rule out a particular joint as a pain generator. This is especially true in the post-whiplash population [10, 15], where imaging may be more helpful in ruling out competing diagnoses.
The current gold standard to diagnose z-joint pain remains controlled diagnostic blocks to the specific joint in question or its nerve supply [13]. A single anesthetic block has a false positive rate as high as 40% [16]. A dual blockade protocol can be used to improve specificity and is recommended in most situations where RFN is considered. For example, on one occasion a short-acting anesthetic such as xylocaine is used, then at a separate time the block is repeated using a longer-acting anesthetic, such as bupivacaine. Patients are blinded as to which anesthetic was used and should complete a pain diary including percentage of relief from their index pain and duration of response. While a well-placed intra-articular injection and medial branch block (MBB) may be equally efficacious for the diagnosis of z-joint pain, MBBs may be a better predictor of response to RFN [25]. Debate continues regarding the most appropriate cutoffs for a “positive response.” Most accept 80% improvement as definitively positive for the lumbar spine, but some argue that 50% is adequate to reduce false-negative responses for selection of patients for RFN [25]. Some studies and insurance companies advocate stricter cutoffs as high as 100% improvement, especially in the cervical spine [15]. A positive concordant response entails a patient demonstrating improvement for a length of time that approximates the duration of action of the anesthetics used. Positive concordant dual blocks reduce false-positives and increase the probability of a successful RFN.
Treatment/Technical Considerations
When pursuing diagnoses and interventional treatments for z-joint pain, some common technical standards should be considered. All procedures should be performed only after thorough informed consent, including a discussion of the procedure, risks, benefits, and alternatives. Sedation should be minimized for any diagnostic procedures. For an effective diagnostic block, patients need to have the index pain at time of the procedure or need to be able to consistently trigger the pain with a movement or activity, such that a pre- and post-procedure comparison can be made. Therapeutic procedures can be performed with or without sedation depending on patient and provider preference, as well as availability of cardiopulmonary monitoring and emergency resuscitative supplies. All procedures should be image-guided, most commonly with biplanar fluoroscopy , and should follow strict sterile precautions. Unless contraindicated, radio-opaque contrast dye should be utilized for all diagnostic blocks to ensure accurate placement and to avoid intravascular injection. For diagnostic intra-articular z-joint injections , no more than 1 mL of volume should be used to avoid capsular rupture or extravasation to surrounding structures including the nerve roots and epidural space (Fig. 38.3). For diagnostic MBBs , no more than 0.5 mL should be used to maintain specificity.


Fig. 38.3
Fluoroscopic image showing successful intra-articular injection of contrast into a cervical facet joint
After diagnosis, therapeutic interventional options include therapeutic intra-articular injection or RFN . Therapeutic intra-articular injection typically involves instillation of corticosteroid with local anesthetic into the joint itself and can provide primarily short-term pain relief. For chronic z-joint pain, RFN can be considered with goal of more sustained improvement of pain and function. The above procedural setup applies to RFN ; however, rather than relying on local anesthetic to block the joint’s nerve supply, a radiofrequency electrode is used to heat the needle tip immediately adjacent to the nerve target (Fig. 38.4).
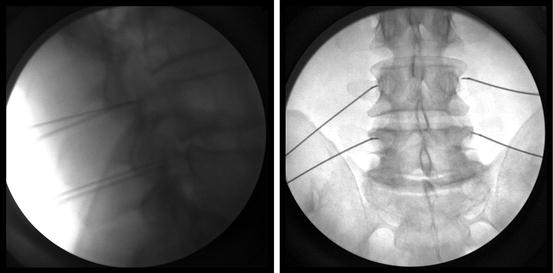
Fig. 38.4
Fluoroscopic images showing lateral and AP images of the radiofrequency electrodes along the L3 and L4 medial branches
Several techniques of RFN are described including pulsed, conventional, or cooled. Pulsed RFN utilizes a lower temperature (~42 °C) for a longer duration (120 s), compared to conventional RFN (~80 °C for 90 s). The rationale for pulsed RFN is to alter neural transmission without fully coagulating the nerve; it may be considered in higher risk areas, such as the upper cervical spine or when there is concern for aberrant anatomy. Conventional RFN aims to coagulate/destroy the target nerve for a longer therapeutic effect. The RF needle tip can sense temperature and shuts off the lesion if temperatures are exceeding 95 °C, a temperature at which surrounding tissues are at risk. Outcomes from conventional RFN are highly dependent on technique, with the best outcomes achieved when the needle tip lies parallel to the target nerve. Cooled RFN is a newer technique that maintains some special advantages over conventional RFN, but carries higher equipment costs that may not be reimbursed by insurance. Cooled RFN utilizes a fluid pump, which circulates sterile water to cool the needle tip and adjacent tissue. With a probe tip temperature of 60 °C, coagulation time is longer (150 s), but the lesion size is larger. Moreover, the lesion extends beyond the needle tip allowing for easier perpendicular needle placement, which is helpful in complex anatomy or SI joint RFN. Added caution is also required with cooled RFN because of the larger lesion size.
Following RFN, the lesioned nerves typically regenerate and can restore nociception to the joint. While duration of effect from RFN varies, positive outcome can be considered at least 50% improvement for at least 6 months.
Cervicogenic Headaches from the C2-3 Joint
Multiple interventional treatments for cervicogenic headaches have been described, with targets including the A-O joints, A-A joints, C2-3 and C3-4 z-joints, C2 spinal nerve, third occipital nerve (TON) , C3 and C4 medial branches, greater occipital nerve (GON) , lesser occipital nerve (LON) , and overlying upper cervical soft-tissue/musculature. Studies estimate about 50% of cervicogenic headaches after whiplash injury emanate from the C2-3 z-joint, which will be emphasized here [14, 15]. The C2-3 z-joint is innervated by the TON . The TON arises from the dorsal ramus of C3 and supplies the C2-3 z-joint capsule, as well as the semispinalis, communicating branches to the GON and LON, and cutaneous innervation of the midline occiput. Treatment options include intra-articular injections or RFN. The intra-articular injection can be performed as described for the other cervical z-joints below. Due to variable course of the TON, RFN is optimally performed by blockade of three adjacent locations of the TON along the lateral pillars of C2 and C3. Dual blockade protocol is recommended for diagnosis, prior to considering RFN. Successful blockade of the TON can be confirmed by the expected sensory alteration in the occipital region.
Neck Pain from Cervical Z-Joints C3-4 to C6-7
The cervical z-joints are predominately coronal in orientation. Cervical z-joint intra-articular injections or MBBs can be performed in the side-lying or prone positions. Cervical RFN is typically performed with the patient prone. The cervical medial branches are targeted after they split from the primary dorsal ramus and when they wrap around the lateral margin of the articular pillar, as they travel posterior to the joint capsule (Fig. 38.1). The medial branch also supplies the multifidus and interspinales muscles and care should be taken to avoid blocking the lateral branch, which supplies many of the larger paraspinal muscles. The medial branches can occasionally have some segmental cutaneous innervation, thus some local numbness is possible with MBBs or RFN . With the exception of C2-3, each cervical z-joint is innervated by two medial branches, numbered consistent with their corresponding vertebral level. For instance, in order to block the C3-4 z-joint, one must block both the C3 and C4 medial branches (Fig. 38.5). The numbering scheme transitions at the cervicothoracic junction, where the C7-T1 z-joint gets innervation from the C7 and C8 (rather than T1) medial branches. This numbering scheme continues through the thoracic and lumbar spine. Dual block protocol with positive concordant response of at least 80–100% improvement is recommended prior to proceeding with RFN.


Fig. 38.5
Fluoroscopic image showing the needle placement for cervical medial branch blocks for the C3 and C4 medial branches
Low Back Pain from the Lumbar Z-Joints
The lumbar z-joints are predominately oblique in orientation, with more variability at L5-S1. The patient is prone for lumbar z-joint procedures. Each lumbar z-joint gets innervation from two medial branches, but the numbering scheme is distinct from the cervical spine. For example, the L3-4 z-joint is supplied by the L2 and L3 medial branches, and the L4-5 z-joint is supplied by the L3 and L4 medial branches (Fig. 38.4). The nomenclature changes again at L5-S1, where the L5-S1 z-joint is supplied by the L4 medial branch and the L5 primary dorsal ramus. The lumbar medial branches go on to innervate the segmental multifidi muscles and do not provide cutaneous innervation. Care should be taken to avoid neurotomy of the lateral branches, which supply larger paraspinal muscles and sometimes overlying skin.
Potential Treatment Complications
Serious complications are very rare (<1%) following intra-articular z-joint injections, MBBs, or RFN. All z-joint procedures carry the usual risk of infection, hematoma, allergic or adverse reaction to the medications used, unintended nerve injury, and vasovagal reaction, including syncope. Risk of catastrophic bleeding, which could lead to spinal cord compression, is extremely low as these procedures all remain outside of the spinal canal. RFN carries some additional unique risks including post-RFN neuritis, anesthesia dolorosa, and muscle injury/denervation. Risk to the dorsal and ventral nerve roots is very low when correct technique is utilized. Post-RFN neuritis can occur with perfect technique and typically involves painful dysesthesias in the distribution of the targeted nerve lasting days to several weeks. Anesthesia dolorosa is a rare chronic deafferentation pain, such that an individual experiences neuropathic pain in a region of cutaneous numbness. Both post-RFN neuritis and anesthesia dolorosa are more common in the upper cervical spine (e.g., TON) with neuritis occurring around 20% of the time and lasting 7–10 days on average [26]. Post-RFN neuritis is frequently treated with corticosteroids. An expected side effect of RFN is local, segmental denervation of the multifidi muscles at the levels of the RFN . While multifidi denervation has not been shown to be clinically significant in cases of successful lumbar RFN [27], significant cervical muscle weakness and kyphosis has been reported following multilevel cervical RFN [28]. It is rare to require RFN to more than two joint levels, to achieve clinical benefit and the fewest number of joints possible to achieve good outcome should be targeted.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree





