INTRODUCTION AND EPIDEMIOLOGY
Normally, the pulmonary vascular system is a high-flow, low-resistance circuit, with a mean pulmonary arterial pressure that constitutes approximately 15% to 20% of the systemic circulation.1 Normal pulmonary arterial systolic pressures range from 15 to 30 mm Hg, whereas diastolic pulmonary arterial pressures range from 4 to 12 mm Hg.1 Pulmonary hypertension is defined as a mean pulmonary arterial pressure >25 mm Hg at rest or >30 mm Hg during exertion.1,2
Pulmonary hypertension is classified based on measurements of pulmonary capillary wedge pressure (PCWP) and pulmonary vascular resistance. Patients with pulmonary arterial hypertension have a mean pulmonary arterial pressure >25 mm Hg, a pulmonary vascular resistance >240 dynes/s/cm5, and a PCWP <15 mm Hg.2 In contrast, patients with pulmonary hypertension caused by left heart disease, the most common cause of pulmonary hypertension, have a PCWP >15 mm Hg.2 Although echocardiography can estimate pulmonary arterial pressure in a patient with suspected pulmonary hypertension, definitive diagnosis requires right heart catheterization.
The World Health Organization classifies pulmonary hypertension into five categories based on cause and response to treatment (Table 58-1).1,3 Some patients have features of multiple categories, but the majority have one predominant type of pulmonary hypertension.4 Accurate classification of pulmonary hypertension is key to directing treatments, which vary among the categories. Pulmonary venous hypertension is the most common cause of pulmonary hypertension, affecting almost 4 million patients in the United States.4 In contrast, pulmonary arterial hypertension is the least common cause of pulmonary hypertension, with an estimated prevalence of 15 patients per million.4,5 Pulmonary hypertension develops in up to 4% of patients with chronic thromboembolic disease.4,6,7 Regardless of the cause, patients with pulmonary hypertension have high morbidity and mortality rates,4,8 with a 5-year mortality rate for patients with idiopathic pulmonary arterial hypertension exceeding 30%.5
Group 1: Pulmonary Arterial Hypertension
Group 2: Pulmonary Venous Hypertension (left heart disease)
Group 3: Chronic Hypoxemic Lung Disease
Group 4: Embolic Disease Group 5: Miscellaneous
|
PATHOPHYSIOLOGY
The exact pathophysiology of all forms of pulmonary hypertension remains unknown. In pulmonary arterial hypertension, the initial abnormality is endothelial dysfunction, which results in an imbalance between endogenous vasodilators (e.g., prostacyclin) and vasoconstrictors (e.g., endothelin-1). The net effect is vasoconstriction and the formation of in situ thrombi. Additional pathologic processes include alterations in microvascular permeability, abnormal hypoxic vasoconstriction, microvascular thrombosis, and the formation of plexiform lesions, leading to vascular remodeling. Ultimately, these abnormalities result in sustained elevations of pulmonary vascular resistance and impairment of pulmonary blood flow.
With persistent elevations in pulmonary vascular resistance, the right ventricle (RV) dilates to maintain an adequate stroke volume. RV dilation increases the ventricular wall tension, increases oxygen consumption, and eventually decreases contractility. With progressive RV dilation, the intraventricular septum is displaced toward the left ventricle. This displacement inhibits left ventricular filling and ultimately impairs cardiac output and systemic perfusion.
Perfusion of the right coronary artery (RCA) depends on the gradient between the aorta and RV. Normally, the RCA is perfused during both systole and diastole. In patients with advanced pulmonary hypertension, RCA perfusion occurs almost exclusively during diastole.9,10 Decreased perfusion results in right ventricular ischemia and further impairment of left ventricular output. Eventually, this cycle results in right ventricular failure and cardiovascular collapse.
CLINICAL FEATURES
The most common symptom of pulmonary hypertension is dyspnea, either at rest or with exertion, which is present in over 50% of patients.1,11 Other symptoms include fatigue, chest pain, near syncope, syncope, and exertional lightheadedness.3,11,12 Since these initial symptoms are nonspecific, it is not surprising that delays in diagnosis are common, with an average interval between symptom onset and diagnosis of pulmonary hypertension of 2 years.13 As pulmonary arterial pressure increases, patients can develop early satiety, anorexia, orthopnea, paroxysmal nocturnal dyspnea, and peripheral edema.
The physical examination is often normal in the early stages of pulmonary hypertension.1 As pulmonary hypertension worsens, findings of right ventricular failure emerge (e.g., a holosystolic tricuspid regurgitation murmur, jugular venous distention, hepatomegaly, ascites, and lower extremity edema).1,4 Additional findings include an increased intensity of the pulmonary component of the second heart sound (P2), a parasternal heave, and a subxiphoid thrust in patients with right ventricular hypertrophy.1,4
DIAGNOSTIC TESTING
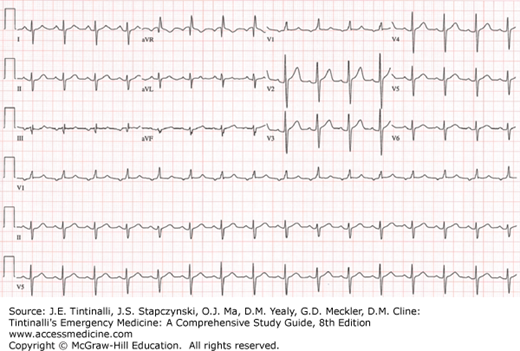
The most common ECG abnormality seen in pulmonary hypertension patients is right axis deviation.12 Additional findings associated with pulmonary hypertension include an R/S ratio >1 in lead V1, an R/S ratio <1 in leads V5 and V6, a qR complex in lead V1, an S1Q3T3, right atrial enlargement in the inferior leads, and an incomplete or complete right bundle branch block14 (Figure 58-1). These findings are neither sensitive nor specific for the identification of pulmonary hypertension.
The ECG may show signs of right ventricular ischemia or dysrhythmia. The most common dysrhythmias in patients with pulmonary hypertension are atrial fibrillation, atrial flutter, and atrioventricular nodal reentrant tachycardia.15,16 Of these, atrial fibrillation is associated with the highest mortality rate.15
Routine laboratory testing (e.g., CBC, comprehensive metabolic panel) is often nonspecific in the initial evaluation of the pulmonary hypertension patient with dyspnea. B-type natriuretic peptide and N-terminal B-type natriuretic peptide are often elevated and correlate with outcomes in patients with pulmonary hypertension but have limited impact in ED care.17,18,19 Elevations in troponin from myocardial ischemia or a strain-induced leak can be seen and are associated with higher morbidity and mortality.20,21
Common chest radiographic abnormalities associated with pulmonary hypertension include enlargement of the right atrium, RV, and hilar pulmonary arteries.12,22
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree