Chapter 30 Pulmonary embolism
Pulmonary embolism (PE) is a commonly considered, but relatively uncommonly diagnosed, condition. It is important to have an adequate understanding of the pathophysiology, as well as a rapid and reliable strategy of investigation and management. This is particularly important in critically ill patients where diagnosis can be difficult and PE may be life-threatening.
AETIOLOGY
Predisposing risk factors for VTE involve one or more components of Virchow’s triad: (1) venous stasis; (2) vein wall injury; and (3) hypercoagulability of blood. The main factors are immobility (from any cause), surgery, trauma, malignancy, pregnancy and thrombophilia (Table 30.1).
Table 30.1 Risk factors for venous thromboembolism
| Primary hypercoagulable states (thrombophilia) |
| Antithrombin III deficiency |
| Protein C deficiency |
| Protein S deficiency |
| Resistance to activated protein C resistance (inherited factor V Leiden mutation) |
| Hyperhomocysteinaemia |
| Lupus anticoagulant (antiphospholipid antibody) |
| Secondary hypercoagulable states |
| Immobility |
| Surgery |
| Trauma |
| Malignancy |
| Pregnancy and the puerperium |
| Obesity |
| Smoking |
| Oestrogen-containing oral contraception or hormone replacement therapy |
| Indwelling catheters in great veins and the right heart |
| Burns |
| Patients with limb paralysis (e.g. spinal injuries) |
| Heart failure |
| Increasing age |
VTE can be recurrent, which should prompt investigation for thrombophilia, which describes a group of conditions which are inherited and associated with a high incidence of VTE. The most important of these is activated protein C resistance, which is mediated by the factor V Leiden mutation. Up to 50% of patients with recurrent VTE episodes (as well as 20% of patients with a single episode) have this condition; however, its association appears to be greater with DVT than with PE.1 Up to 5% of patients with VTE develop chronic pulmonary hypertension.2
PATHOPHYSIOLOGY
Acute pulmonary hypertension increases right ventricular (RV) afterload and RV wall tension, which leads to RV dilatation and dysfunction, with coronary ischaemia being a major contributing mechanism.3 In massive PE, the combination of coronary ischaemia, RV systolic failure, paradoxical interventricular septal shift and pericardial constraint leads to left ventricular (LV) dysfunction and a ‘low-cardiac-output’ shock state. In patients with underlying cardiorespiratory disease, a small PE can have profound consequences.
CLINICAL PRESENTATION
PE is relatively uncommon in critically ill patients despite the frequent presence of risk factors for VTE. However, when PE does occur, the diagnosis is frequently overlooked or is difficult to confirm because of the presence of coexistent cardiorespiratory disease. Clinical assessment raises the suspicion of PE but is neither sensitive nor specific. A number of clinical prediction systems have been developed, the most widely reported of which are the Wells’ score and the Geneva score.4 The differential diagnosis is listed in Table 30.2.
Table 30.2 Differential diagnosis of pulmonary embolism
| Acute myocardial infarction |
| Acute pulmonary oedema |
| Pneumonia |
| Asthma or exacerbation of chronic obstructive pulmonary disease |
| Pericardial tamponade |
| Pleural effusion |
| Fat embolism |
| Pneumothorax |
| Aortic dissection |
| Rib fracture |
| Musculoskeletal pain |
| Anxiety |
SYMPTOMS
Dyspnoea, pleuritic chest pain, and haemoptysis are the classic symptoms of PE. Most patients will have at least one of these symptoms, with dyspnoea being the most common. The combination of pleuritic chest pain and haemoptysis reflects a late presentation where pulmonary infarction has occurred. If syncope occurs there is a high likelihood that there has been a massive PE. A family history of venous thrombosis raises the possibility of inherited thrombophilia.
INVESTIGATIONS
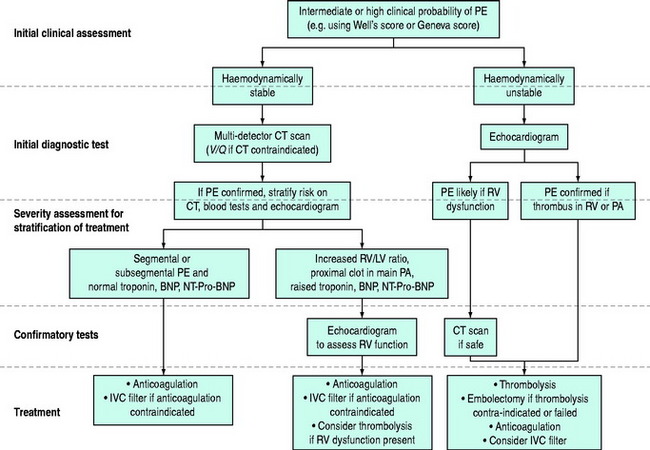
The diagnosis of PE requires a high level of clinical suspicion and the appropriate use of investigations. The aim of these investigations is to confirm or exclude the presence of PE and then to stratify treatment accordingly. The optimal investigation strategy depends upon the individual patient and institution as a number of investigations are available. Pulmonary angiography has traditionally been considered the ‘gold standard’ for the diagnosis of PE. The advent of multidetector row computed tomography (CT) scanning (which compares well with standard pulmonary angiography5) has led to the emergence of this as the ‘first-line’ test in many centres. A suggested investigation algorithm is shown in Figure 30.1.
D-DIMER
The serum D-dimer level is useful for exclusion of VTE, particularly when it is normal and combined with a low-risk clinical assessment.6 A variety of different assays are available. Negative tests, particularly from enzyme-linked immunosorbent assays (ELISA), are highly predictive of the absence of both DVT and PE.7 A high D-dimer concentration is also an independent predictive factor associated with mortality.8
TROPONIN, BRAIN NATRIURETIC PEPTIDE (BNP) AND NT-TERMINAL PRO-BNP
Although of little use for diagnosis, measurement of troponin, BNP or NT-terminal Pro-BNP can add to the risk stratification of patients with known PE. The presence of a raised troponin is associated with haemodynamic instability in patients with non-massive PE independently of clinical, echocardiographic and laboratory findings.9 Raised troponin also predicts a higher mortality.10 Low levels of BNP and NT-terminal Pro-BNP have been shown to correlate with an uneventful course in patients with known PE.11 NT-terminal Pro-BNP appears to be a better predictor of outcome than troponin.12
ARTERIAL BLOOD GASES
A normal arterial blood gas profile does not rule out the diagnosis; however hypoxaemia (with a widened alveolar–arterial oxygen gradient), hypocapnia and an increased end-tidal CO2 gradient13 should raise the suspicion of PE, even though there are many other causes of these findings in critically ill patients.14 Metabolic acidosis may be present if shock from a large PE occurs.
CHEST X-RAY
The chest X-ray is often normal or only slightly abnormal, with non-specific signs such as cardiac enlargement, pleural effusion, elevated hemidiaphragm, atelectasis and localised infiltrates. More specific findings, including focal oligaemia, a peripheral wedge-shaped density above the diaphragm or an enlarged right descending pulmonary artery,15 are uncommon and difficult for non-radiologists to identify. The chest X-ray is also useful in identifying an alternative diagnosis such as pneumothorax, pneumonia, acute pulmonary oedema, rib fracture and pleural effusion.
COMPUTED TOMOGRAPHY
As CT technology has improved, CT angiography (CTA) has emerged as a cost-effective and clinically reliable alternative to the V/Q scan.16 The single-detector row CT has been superseded by multidetector row CT, which allows imaging of the entire chest with high-resolution images in ‘in-plane’ and ‘through-plane’ resolution. High-resolution images to the level of segmental and in some cases subsegmental pulmonary arteries can be obtained in a short time period (often a single breath-hold).
When CTA is compared to conventional angiography it appears reliable, with sensitivity, specificity and accuracy of 100%, 89% and 91% respectively.5 Adding venography of the leg veins to the CTA (CTA-CTV) further increases the diagnostic certainty.17 It is therefore recommended that CTA or CTA-CTV should be the principal radiological test for patients with high and moderate probability of PE.18
Although the ability of many CT scanners to detect PE at the subsegmental level is limited, it is debatable whether this is of clinical significance. Patients who have negative or indeterminate CT scans and in whom anticoagulation is withheld have low subsequent rates of thromboembolic events.19
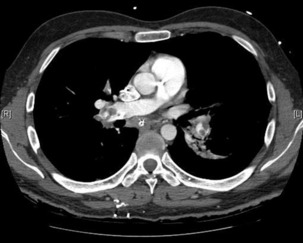
The advantage of CT is that it can not only diagnose PE but can also be used to assess severity of the condition. Increased RV/LV ratio (> 0.9)20 and clot in the proximal branches of the pulmonary artery21 correlate with the clinical severity of PE. Severity stratification is further increased by combining CT with other tests such as troponin9 and BNP or NT-terminal ProBNP.11 CT scanning may also identify the causative DVT in the veins of the legs, pelvis and abdomen or detect alternative or additional diagnoses such as a pulmonary mass, pneumonia, emphysema, pneumothorax, pleural effusion or mediastinal adenopathy (Figure 30.2).
ECHOCARDIOGRAPHY
Because of its portability, echocardiography has become increasingly useful in critically ill patients with possible PE. Many patients with PE have an echocardiographic abnormality, the most common being RV dilatation, RV hypokinesis, paradoxical interventricular septal motion toward the LV, tricuspid regurgitation and pulmonary hypertension.22 The pattern of RV hypokinesis with apical sparing is considered pathognomonic for PE.23 The presence of RV dysfunction correlates with mortality.24 Echocardiography is poor at excluding PE, as a negative echocardiogram can miss up to 50% of PEs.25
Transthoracic echocardiography will also allow estimation of pulmonary arterial pressure, identification of intracardiac thrombi (which usually requires surgical embolectomy) and aids in differential diagnosis by excluding aortic dissection and pericardial tamponade. Transoesophageal echocardiography has the additional benefit of directly identifying embolus in the proximal pulmonary arteries, which is common in patients with haemodynamically significant PE.26
VENTILATION/PERFUSION SCANNING
The lung ventilation/perfusion (V/Q) scan is becoming less commonly used with the advent of multidetector row CT. The perfusion scan identifies defects in perfusion which may be classified as single or multiple, and as subsegmental, segmental or lobar. By combining this with ventilation scanning, these perfusion defects can then be labelled as mismatched (normal ventilation in a zone of perfusion defect) or matched defects (ventilation defect corresponds to perfusion defect). The probability of PE is then classified as high, intermediate or low probability for PE, or normal.27
Despite the increased use of CT, the V/Q scan retains a role when CT is either unavailable or contraindicated (e.g. significant renal impairment, anaphylaxis to intravenous contrast or pregnancy).15V/Q scanning also allows quantification of regional blood flow within the lungs, which may be required in the assessment of chronic pulmonary venous embolism.
SEARCH FOR DEEP VENOUS THROMBOSIS
Leg venography is a more sensitive test; however, it is invasive and now uncommonly performed.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree