BASICS
![]() Neglect or failure of the individual responsible to provide needs and protection to a vulnerable person
Neglect or failure of the individual responsible to provide needs and protection to a vulnerable person
![]() Considered elder abuse in patients >60 years old
Considered elder abuse in patients >60 years old
![]() Failure to provide food, water, medicine, and clothing or financial exploitation
Failure to provide food, water, medicine, and clothing or financial exploitation
![]() Risk factors include advanced age, disability in self-care, low socioeconomic status, or institutional staffing shortages
Risk factors include advanced age, disability in self-care, low socioeconomic status, or institutional staffing shortages
SIGNS AND SYMPTOMS
![]() Suspicious pressure ulcers, skin tears, wounds, and burns
Suspicious pressure ulcers, skin tears, wounds, and burns
![]() Fractures, bruises
Fractures, bruises
![]() Malnutrition and dehydration
Malnutrition and dehydration
![]() Signs of sexual abuse such as sores or bleeding genital/anal areas
Signs of sexual abuse such as sores or bleeding genital/anal areas
DIAGNOSTICS
![]() Detailed history and clinical exam findings for signs of abuse
Detailed history and clinical exam findings for signs of abuse
![]() Screening questions
Screening questions
TREATMENT
![]() Social work consultation
Social work consultation
![]() Report reasonable suspicion to designated governmental resources
Report reasonable suspicion to designated governmental resources
BASICS
![]() Nonconsensual sexual mistreatment against a vulnerable individual
Nonconsensual sexual mistreatment against a vulnerable individual
![]() Occurs at any age in domestic or institutional settings
Occurs at any age in domestic or institutional settings
![]() Typically by someone in a position of authority over the victim
Typically by someone in a position of authority over the victim
SIGNS AND SYMPTOMS
![]() Sexually transmitted diseases or unplanned pregnancies
Sexually transmitted diseases or unplanned pregnancies
![]() Evidence of forced penetration into oral cavity, rectum, or female genitalia
Evidence of forced penetration into oral cavity, rectum, or female genitalia
![]() Trauma of the genitalia or anal area, including lesions, sores, or irritation
Trauma of the genitalia or anal area, including lesions, sores, or irritation
![]() Sexually abused children can be hypersexual or sexually permissive
Sexually abused children can be hypersexual or sexually permissive
DIAGNOSTICS
![]() Clinical exam findings, including genital, pelvic, and rectal exam
Clinical exam findings, including genital, pelvic, and rectal exam
![]() Screening questions
Screening questions
TREATMENT
![]() Social work consultation
Social work consultation
![]() Medical treatment for sexually transmitted infection and wounds
Medical treatment for sexually transmitted infection and wounds
![]() Report reasonable suspicion to designated governmental resources
Report reasonable suspicion to designated governmental resources
Intimate Partner Abuse (Spousal or Domestic Abuse)
BASICS
![]() Physical, psychological, or sexual harm is inflicted or threatened by a spouse or partner
Physical, psychological, or sexual harm is inflicted or threatened by a spouse or partner
SIGNS AND SYMPTOMS
![]() Inappropriate or distant affect
Inappropriate or distant affect
![]() Injuries similar to abused patient, including fractures, bruising, bleeding, or sores on genitals or anal area
Injuries similar to abused patient, including fractures, bruising, bleeding, or sores on genitals or anal area
![]() Inconsistent explanations, missed appointments
Inconsistent explanations, missed appointments
DIAGNOSTICS
![]() Detailed history and clinical exam findings
Detailed history and clinical exam findings
![]() Screening questions
Screening questions
TREATMENT
![]() Social support consultation
Social support consultation
![]() Report reasonable suspicion to designated governmental resources
Report reasonable suspicion to designated governmental resources
BASICS
![]() Physical or psychological harm imposed upon a child
Physical or psychological harm imposed upon a child
![]() Neglect or failure to provide protection and basic needs
Neglect or failure to provide protection and basic needs
![]() Includes Munchausen syndrome by proxy, abuse inflicted by a parent or guardian
Includes Munchausen syndrome by proxy, abuse inflicted by a parent or guardian
SIGNS AND SYMPTOMS
![]() Suspicious injuries for which the mechanism is not adequately explained
Suspicious injuries for which the mechanism is not adequately explained
![]() Bruises, fractures (commonly spiral fractures), and burns
Bruises, fractures (commonly spiral fractures), and burns
![]() Retinal hemorrhages can be seen in shaken baby syndrome
Retinal hemorrhages can be seen in shaken baby syndrome
![]() Psychological or psychiatric disturbances as a result of the abuse
Psychological or psychiatric disturbances as a result of the abuse
DIAGNOSTICS
![]() Detailed history and clinical exam findings
Detailed history and clinical exam findings
![]() Screening questions
Screening questions
TREATMENT
![]() Social work consultation
Social work consultation
![]() Report reasonable suspicion to designated governmental resources
Report reasonable suspicion to designated governmental resources
![]() BEHAVIORAL AND PERSONALITY DISORDERS
BEHAVIORAL AND PERSONALITY DISORDERS
Attention Deficit Disorder/Attention Deficit Hyperactivity Disorder
BASICS
![]() Impulsivity, inattentiveness, and/or hyperactivity causing impaired social function
Impulsivity, inattentiveness, and/or hyperactivity causing impaired social function
![]() Typically diagnosed in childhood and can persist throughout adulthood
Typically diagnosed in childhood and can persist throughout adulthood
SIGNS AND SYMPTOMS
![]() Fails to follow instructions
Fails to follow instructions
![]() Poor concentration
Poor concentration
![]() Difficulty organizing
Difficulty organizing
![]() Easily distracted by outside stimuli
Easily distracted by outside stimuli
![]() Forgetful
Forgetful
DIAGNOSTICS
![]() Diagnosis requires hyperactivity, impulsivity, or inattentiveness
Diagnosis requires hyperactivity, impulsivity, or inattentiveness
![]() Before age 7
Before age 7
![]() Demonstrates in two separate environmental settings
Demonstrates in two separate environmental settings
TREATMENT
![]() First line: methylphenidate, dextroamphetamine, or combination medications
First line: methylphenidate, dextroamphetamine, or combination medications
![]() Noncontrolled substances, including antidepressant medications or some serotonin-norepinephrine reuptake inhibitors
Noncontrolled substances, including antidepressant medications or some serotonin-norepinephrine reuptake inhibitors
![]() Behavioral therapy should be used in addition to pharmacotherapy
Behavioral therapy should be used in addition to pharmacotherapy
BASICS
![]() Childhood behavioral disorders
Childhood behavioral disorders
![]() Conduct disorder
Conduct disorder
• Violates social norms and basic rights of other people, animals, or property
![]() Oppositional defiant disorder
Oppositional defiant disorder
• Deliberately defies authority and rules
• Purposely annoys or angers others
SIGNS AND SYMPTOMS
![]() Hostile, defiant, negative attitude, loses temper easily
Hostile, defiant, negative attitude, loses temper easily
TREATMENT
![]() Focused individual, group or family psychotherapy
Focused individual, group or family psychotherapy
Pervasive Developmental Disorder
BASICS
![]() Causes severe deficit in social interaction with impaired communication
Causes severe deficit in social interaction with impaired communication
![]() Autism, Asperger syndrome
Autism, Asperger syndrome
SIGNS AND SYMPTOMS
![]() Methodical, repetitive, or stereotyped behavior
Methodical, repetitive, or stereotyped behavior
![]() Impaired social interaction
Impaired social interaction
![]() Difficult communication or nonverbal
Difficult communication or nonverbal
![]() Poor relationship development
Poor relationship development
TREATMENT
![]() Individual therapy according to needs
Individual therapy according to needs
BASICS
![]() Characteristics that range across social, interpersonal, and environmental contexts
Characteristics that range across social, interpersonal, and environmental contexts
![]() Impair adaptation and function in social, occupational, and domestic settings (Table 12.1)
Impair adaptation and function in social, occupational, and domestic settings (Table 12.1)
| Personality Disorders |
Cluster A “wild and mad” | Cluster B “wild and bad” | Cluster C “whiny and sad” |
|
|
|
SIGNS AND SYMPTOMS
![]() See above chart for specific characteristics of each type of personality disorder
See above chart for specific characteristics of each type of personality disorder
TREATMENT
![]() Tend to be unaware of their disorder and may not seek treatment
Tend to be unaware of their disorder and may not seek treatment
![]() Individual and group therapy with insight orientation
Individual and group therapy with insight orientation
![]() Referral to psychiatric services
Referral to psychiatric services
![]() Comorbidities include substance abuse, suicidal ideation, depression, anxiety, and functional impairment
Comorbidities include substance abuse, suicidal ideation, depression, anxiety, and functional impairment
![]() Medical therapy with antidepressant, antianxiety, and mood-stabilizing medications to treat associated symptoms
Medical therapy with antidepressant, antianxiety, and mood-stabilizing medications to treat associated symptoms
BASICS
![]() Prolonged depression with episodes of mania
Prolonged depression with episodes of mania
![]() Females > males
Females > males
![]() High suicide risk
High suicide risk
SIGNS AND SYMPTOMS
![]() Mania
Mania
• Decreased need for sleep
• Pressured speech
• Increased libido
• Reckless behavior, excessive spending without regard
• Grandiosity
• Severe thought disturbances
DIAGNOSTICS
![]() Manic episode criteria
Manic episode criteria
• Greater than 1 week of elation, irritability, or expansiveness plus three mania symptoms
TREATMENT
![]() Drug and alcohol screen
Drug and alcohol screen
![]() Assess for suicidal ideations
Assess for suicidal ideations
![]() Anxiolytics, benzodiazepines (lorazepam, clonazepam)
Anxiolytics, benzodiazepines (lorazepam, clonazepam)
![]() Psych consult for consideration of hospital admission
Psych consult for consideration of hospital admission
BASICS
![]() Three types:
Three types:
• Major depression
• Minor depression
• Dysthymic disorder
ETIOLOGY
![]() Genetics
Genetics
![]() Environmental, that is, major life event
Environmental, that is, major life event
![]() Disturbance in central nervous system 5-hydroxytryptamine levels and neuroendocrine abnormalities
Disturbance in central nervous system 5-hydroxytryptamine levels and neuroendocrine abnormalities
SIGNS AND SYMPTOMS
![]() Depressed mood, diminished interest or pleasure in activities
Depressed mood, diminished interest or pleasure in activities
![]() Weight change, sleep disturbances
Weight change, sleep disturbances
![]() Psychomotor agitation or retardation, fatigue, feeling of worthlessness
Psychomotor agitation or retardation, fatigue, feeling of worthlessness
![]() Thoughts of death or suicide
Thoughts of death or suicide
![]() Diminished ability to concentrate
Diminished ability to concentrate
DIAGNOSTICS
![]() Major depression: five depressive symptoms daily >2 weeks
Major depression: five depressive symptoms daily >2 weeks
![]() Minor depression: two depressive symptoms for >2 weeks
Minor depression: two depressive symptoms for >2 weeks
![]() Dysthymic disorder: mild depressive symptoms >2 years
Dysthymic disorder: mild depressive symptoms >2 years
TREATMENT
![]() Selective serotonin reuptake inhibitors (SSRIs), serotonin-norepinephrine reuptake inhibitors, atypical antidepressants, MAOIs (do not combine with SSRI; serotonin syndrome risk), tricyclic antidepressant s (avoid in suicidal patients)
Selective serotonin reuptake inhibitors (SSRIs), serotonin-norepinephrine reuptake inhibitors, atypical antidepressants, MAOIs (do not combine with SSRI; serotonin syndrome risk), tricyclic antidepressant s (avoid in suicidal patients)
![]() Outpatient referral for consideration of psychotherapy, electroconvulsive therapy, light therapy
Outpatient referral for consideration of psychotherapy, electroconvulsive therapy, light therapy
![]() If patient expresses suicidal ideations in the emergency department:
If patient expresses suicidal ideations in the emergency department:
• Must search and/or remove belongings
• 1:1 sitter for safety monitoring
• Place patient on section 12
• Psychiatry consult to determine disposition
BASICS
![]() Powerful emotional stressor relating to the loss of someone close
Powerful emotional stressor relating to the loss of someone close
![]() Grief reaction in response, causing emotional pain
Grief reaction in response, causing emotional pain
![]() Anticipatory grief with the knowledge of impending loss
Anticipatory grief with the knowledge of impending loss
![]() Complicated bereavement is prolonged or persistent grief
Complicated bereavement is prolonged or persistent grief
SIGNS AND SYMPTOMS
![]() Feelings of shock, disbelief, numbness
Feelings of shock, disbelief, numbness
![]() Overwhelming sadness, depression, anxiety
Overwhelming sadness, depression, anxiety
TREATMENT
![]() Self-limiting with resolution within 6 months
Self-limiting with resolution within 6 months
![]() Prolonged or complicated bereavement persists longer than 6 months
Prolonged or complicated bereavement persists longer than 6 months
BASICS
![]() Panic attack: acute episode of intense physical symptoms and fear, rapidly peaks in 10 minutes, resolves in ~20 minutes
Panic attack: acute episode of intense physical symptoms and fear, rapidly peaks in 10 minutes, resolves in ~20 minutes
![]() Panic disorder: recurrent panic attacks or fear of another attack
Panic disorder: recurrent panic attacks or fear of another attack
![]() Genetic, family history is common
Genetic, family history is common
ETIOLOGY
![]() Limbic system: release of norepinephrine and serotonin
Limbic system: release of norepinephrine and serotonin
![]() Risk factors:
Risk factors:
• Female
• Family history
• Illness
• Drug abuse
• History of recent major life event (<1 year)
SIGNS AND SYMPTOMS
![]() Cardiac: palpitations, tachycardia, chest pain
Cardiac: palpitations, tachycardia, chest pain
![]() Respiratory: shortness of breath, choking
Respiratory: shortness of breath, choking
![]() Neurologic: dizzy, tremor, faint, paresthesia, sweating, chills, flushing
Neurologic: dizzy, tremor, faint, paresthesia, sweating, chills, flushing
![]() Gastrointestinal: nausea, abdominal pain
Gastrointestinal: nausea, abdominal pain
![]() Intense fear of myocardial infarction (MI) or death
Intense fear of myocardial infarction (MI) or death
DIAGNOSTICS
![]() Detailed history
Detailed history
![]() Labs: toxicology screen, complete blood count (CBC), basic metabolic panel, thyroid-stimulating hormone
Labs: toxicology screen, complete blood count (CBC), basic metabolic panel, thyroid-stimulating hormone
![]() Consider EKG to rule out cardiac etiology
Consider EKG to rule out cardiac etiology
TREATMENT
![]() Patient education of symptoms
Patient education of symptoms
![]() High-potency benzodiazepines
High-potency benzodiazepines
• Lorazepam: quick onset, long duration
• Clonazepam: slow onset, long duration
• Alprazolam: avoid if possible, risk of rebound anxiety
![]() Avoid low-potency benzodiazepines (diazepam, chlordiazepoxide)
Avoid low-potency benzodiazepines (diazepam, chlordiazepoxide)
![]() Panic disorder outpatient treatment
Panic disorder outpatient treatment
• SSRI, clonazepam
BASICS
![]() Anxiety so intense and long lasting that it interferes with daily functioning
Anxiety so intense and long lasting that it interferes with daily functioning
![]() Not focused on a particular objection or situation
Not focused on a particular objection or situation
![]() Lasts at least 6 months in duration
Lasts at least 6 months in duration
ETIOLOGY
![]() Previous life experiences
Previous life experiences
![]() Environmental factors, genetic component
Environmental factors, genetic component
SIGNS AND SYMPTOMS
![]() Excessive worry, restlessness, feeling on edge, easily fatigued, difficulty concentrating, irritability, muscle tension, sleep disturbance, increased heart rate (HR), diaphoresis, tachypnea, dry mouth
Excessive worry, restlessness, feeling on edge, easily fatigued, difficulty concentrating, irritability, muscle tension, sleep disturbance, increased heart rate (HR), diaphoresis, tachypnea, dry mouth
DIAGNOSTICS
![]() Consider labs, imaging to rule out physiologic or medical explanations behind signs and symptoms
Consider labs, imaging to rule out physiologic or medical explanations behind signs and symptoms
TREATMENT
![]() Combination therapy: psychotherapy and psychopharmacology
Combination therapy: psychotherapy and psychopharmacology
![]() Stress reduction techniques
Stress reduction techniques
![]() Antidepressants (often SSRIs) for long-term therapy
Antidepressants (often SSRIs) for long-term therapy
![]() Benzodiazepines for short-term use
Benzodiazepines for short-term use
BASICS
![]() Gross impairment of reality
Gross impairment of reality
![]() Broad term to categorize a condition that can result from a variety of psychiatric and medical illnesses
Broad term to categorize a condition that can result from a variety of psychiatric and medical illnesses
ETIOLOGY
![]() Psychiatric disorders:
Psychiatric disorders:
• Schizophrenia
• Schizoaffective disorder
• Mood disorders
• Delusional disorder
• Post-traumatic stress disorder
![]() Medical conditions:
Medical conditions:
• Delirium, stroke, malignancy, endocrine disease, autoimmune disorders, nutritional deficiencies, electrolyte imbalance, neurodevelopmental disorders, multiple sclerosis, Alzheimer disease, Parkinson disease
![]() Substance abuse:
Substance abuse:
• Cannabis, cocaine, amphetamines, psychedelic drugs, alcohol, prescription medications
SIGNS AND SYMPTOMS
![]() Hallucinations and delusions
Hallucinations and delusions
![]() Thought disorder: incoherence, thought blocking, clanging, echolalia, concreteness, poverty of speech, overinclusiveness
Thought disorder: incoherence, thought blocking, clanging, echolalia, concreteness, poverty of speech, overinclusiveness
DIAGNOSTICS
![]() Labs and imaging must be performed to rule out psychosis as a secondary cause (toxicology, brain MRI, electrolyte levels, etc.)
Labs and imaging must be performed to rule out psychosis as a secondary cause (toxicology, brain MRI, electrolyte levels, etc.)
TREATMENT
![]() Atypical antipsychotics: clozapine, olanzapine, risperidone, quetiapine, aripiprazole
Atypical antipsychotics: clozapine, olanzapine, risperidone, quetiapine, aripiprazole
![]() Psychotherapy
Psychotherapy
Neuroleptic Malignant Syndrome
BASICS
![]() Life-threatening neurologic reaction to antipsychotic medications
Life-threatening neurologic reaction to antipsychotic medications
ETIOLOGY
![]() Most commonly from antipsychotic drugs
Most commonly from antipsychotic drugs
• Haldol
• Chlorpromazine
![]() Atypical psychotics:
Atypical psychotics:
• Clozapine
• Risperidone
• Olanzapine
![]() Dopaminergic drugs:
Dopaminergic drugs:
• Levodopa
• Reglan
SIGNS AND SYMPTOMS
![]() Muscle cramps and tremors
Muscle cramps and tremors
![]() Fever
Fever
![]() Hypertension, tachycardia
Hypertension, tachycardia
![]() Alerted mental status
Alerted mental status
DIAGNOSTICS
![]() Detailed history, including medication list
Detailed history, including medication list
![]() Labs including CBC, creatine kinase, myoglobin, LFTs
Labs including CBC, creatine kinase, myoglobin, LFTs
TREATMENT
![]() ABCs, IV fluids, supportive
ABCs, IV fluids, supportive
![]() Discontinue antipsychotics
Discontinue antipsychotics
![]() Dantrolene: treats symptoms including muscle rigidity
Dantrolene: treats symptoms including muscle rigidity
BASICS
![]() Abuse: self-administration of psychoactive drugs in ways that deviate from a culture’s social norms
Abuse: self-administration of psychoactive drugs in ways that deviate from a culture’s social norms
![]() Dependence can be physical (addiction) or psychological
Dependence can be physical (addiction) or psychological
![]() Tolerance: increasingly larger drug doses are required to produce the same effect
Tolerance: increasingly larger drug doses are required to produce the same effect
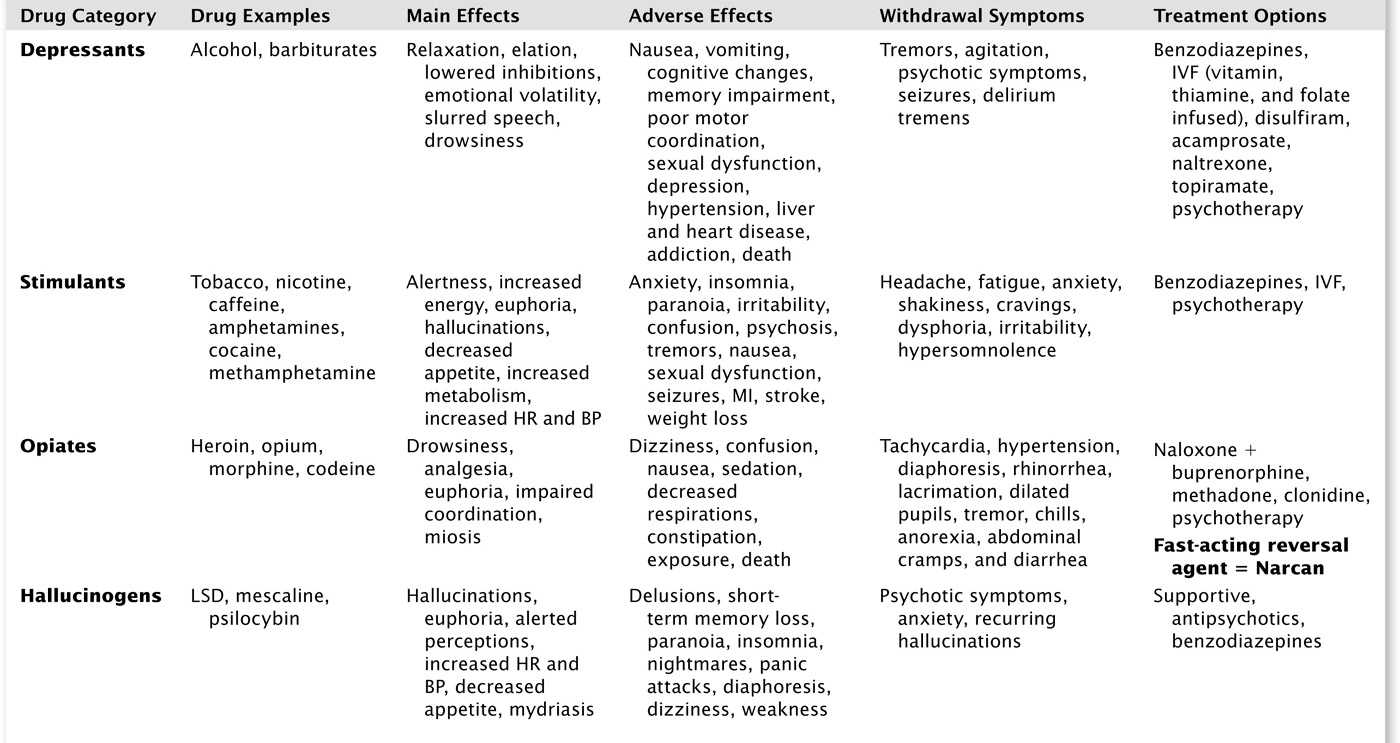
![]() Withdrawal syndrome: symptoms associated with discontinuation of habit forming substance (Table 12.2)
Withdrawal syndrome: symptoms associated with discontinuation of habit forming substance (Table 12.2)
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree